FEN1 Blockade for Platinum Chemo-Sensitization and Synthetic Lethality in Epithelial Ovarian Cancers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BER and Folate Deficiency: a Comprehensive Overview of DNA Base Excision Repair and the Effect of Dietary Folate Lydia Lanni [email protected]
Wayne State University Honors College Theses Irvin D. Reid Honors College Winter 5-7-2012 BER and Folate Deficiency: A comprehensive overview of DNA base excision repair and the effect of dietary folate Lydia Lanni [email protected] Follow this and additional works at: https://digitalcommons.wayne.edu/honorstheses Part of the Human and Clinical Nutrition Commons Recommended Citation Lanni, Lydia, "BER and Folate Deficiency: A comprehensive overview of DNA base excision repair and the effect of dietary folate" (2012). Honors College Theses. 2. https://digitalcommons.wayne.edu/honorstheses/2 This Honors Thesis is brought to you for free and open access by the Irvin D. Reid Honors College at DigitalCommons@WayneState. It has been accepted for inclusion in Honors College Theses by an authorized administrator of DigitalCommons@WayneState. Running head: BER AND FOLATE DEFICIENCY 1 BER and Folate Deficiency: A comprehensive overview of DNA base excision repair and the effect of dietary folate Lydia Lanni Wayne State University Honors Thesis Winter 2012 Author Note A special thank you to Dr. Diane Cabelof and all those in her lab for their instruction and support. BER AND FOLATE DEFICIENCY 2 Abstract Folate is the naturally occurring form of water-soluble B vitamin that is found in foods such as leafy vegetables, fruits, legumes, etc. Dietary supplementation of folate has shown to be protective against neural tube defects and other congenital disorders, and of recent, its role in carcinogenesis has been of special interest. Though mechanistically unclear, a positive correlation has been observed between folate deficiency in the diet and decrease function of DNA base excision repair pathways. -
Oxidative Stress in Sperm Affects the Epigenetic Reprogramming in Early
Wyck et al. Epigenetics & Chromatin (2018) 11:60 https://doi.org/10.1186/s13072-018-0224-y Epigenetics & Chromatin RESEARCH Open Access Oxidative stress in sperm afects the epigenetic reprogramming in early embryonic development Sarah Wyck1,2,3, Carolina Herrera1, Cristina E. Requena4,5, Lilli Bittner1, Petra Hajkova4,5, Heinrich Bollwein1* and Rafaella Santoro2* Abstract Background: Reactive oxygen species (ROS)-induced oxidative stress is well known to play a major role in male infer- tility. Sperm are sensitive to ROS damaging efects because as male germ cells form mature sperm they progressively lose the ability to repair DNA damage. However, how oxidative DNA lesions in sperm afect early embryonic develop- ment remains elusive. Results: Using cattle as model, we show that fertilization using sperm exposed to oxidative stress caused a major developmental arrest at the time of embryonic genome activation. The levels of DNA damage response did not directly correlate with the degree of developmental defects. The early cellular response for DNA damage, γH2AX, is already present at high levels in zygotes that progress normally in development and did not signifcantly increase at the paternal genome containing oxidative DNA lesions. Moreover, XRCC1, a factor implicated in the last step of base excision repair (BER) pathway, was recruited to the damaged paternal genome, indicating that the maternal BER machinery can repair these DNA lesions induced in sperm. Remarkably, the paternal genome with oxidative DNA lesions showed an impairment of zygotic active DNA demethylation, a process that previous studies linked to BER. Quantitative immunofuorescence analysis and ultrasensitive LC–MS-based measurements revealed that oxidative DNA lesions in sperm impair active DNA demethylation at paternal pronuclei, without afecting 5-hydroxymethyl- cytosine (5hmC), a 5-methylcytosine modifcation that has been implicated in paternal active DNA demethylation in mouse zygotes. -

DNA Damage in Neurodegenerative Diseases
Mutation Research 776 (2015) 84–97 Contents lists available at ScienceDirect Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis j ournal homepage: www.elsevier.com/locate/molmut Comm unity address: www.elsevier.com/locate/mutres Review DNA damage in neurodegenerative diseases ∗ ∗∗ Fabio Coppedè , Lucia Migliore Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy a r t i c l e i n f o a b s t r a c t Article history: Following the observation of increased oxidative DNA damage in nuclear and mitochondrial DNA Available online 9 December 2014 extracted from post-mortem brain regions of patients affected by neurodegenerative diseases, the last years of the previous century and the first decade of the present one have been largely dedicated to Keywords: the search of markers of DNA damage in neuronal samples and peripheral tissues of patients in early, Alzheimer’s disease intermediate or late stages of neurodegeneration. Those studies allowed to demonstrate that oxidative Parkinson’s disease DNA damage is one of the earliest detectable events in neurodegeneration, but also revealed cytoge- Amyotrophic Lateral Sclerosis netic damage in neurodegenerative conditions, such as for example a tendency towards chromosome DNA damage 21 malsegregation in Alzheimer’s disease. As it happens for many neurodegenerative risk factors the Chromosome damage Epigenetics question of whether DNA damage is cause or consequence of the neurodegenerative process is still open, and probably both is true. The research interest in markers of oxidative stress was shifted, in recent years, towards the search of epigenetic biomarkers of neurodegenerative disorders, following the accu- mulating evidence of a substantial contribution of epigenetic mechanisms to learning, memory processes, behavioural disorders and neurodegeneration. -

Commercial Partnerships Annual Review 19/20
1 Overview Commercial Partnerships Annual Review 19/20 Together we will beat cancer 2 Overview Our missions & values Contents CRUK’s vision is to bring forward the day when all cancers Overview are cured. Over the last 40 years, cancer survival rates in 4 CBO’s statement the UK have doubled. In the 1970s just a quarter of people 5 Highlights from the 19/20 financial year survived. Today that figure is half. In order to improve on this, we need to work with industry partners to progress Introduction the best ideas to market. This is where the Commercial Partnerships team can help. 2 What we do and why 7 Where we do it 8 Our principles for doing business 9 Our commitment to CRUK funded researchers Our Our Our 10 Our Commercial Objectives mission vision ambition Our achievements 11 - 17 Objective 1: Supporting researchers with translational activity The mission of CRUK Commercial Together we will 18 - 19 Objective 2: Encouraging entrepreneurial culture and skills in CRUK Commercial Partnerships will be beat cancer and our research community Partnerships is to the world’s leading see 3/4 of people maximise the translation cancer translation and survive by 2034 20 - 26 Objective 3: Develop industry partnerships in therapeutics of cancer research for commercialisation 27 - 29 Objective 4: Diversify and maximise opportunities beyond therapeutics patient benefit group 30 - 31 Objective 5: Invest in our people and processes, promote diversity See our objectives on See our achievements on See our impact on 32 - 35 Objective 6: Leverage and return -

The Francis Crick Institute
Clinical Medicine 2017 Vol 17, No 2: 105–7 PROFESSIONAL ISSUES T h e F r a n c i s C r i c k I n s t i t u t e A u t h o r s : K e i t h P e t e r s A a n d J i m S m i t h B The Francis Crick Institute Laboratory, opened in 2016, is sup- is within easy reach of GlaxoSmithKine (GSK) and Astra ported by the Medical Research Council, Cancer Research UK, Zeneca’s principal research laboratories in Stevenage and the Wellcome Trust, and University College London, King’s Col- Cambridge, respectively. lege London and Imperial College London. The emphasis on But in order to justify investment on the scale required, the research training and early independence of gifted scientists new institute needed to be more than a simple translocation to ABSTRACT in a multidisciplinary environment provides unique opportuni- a new site. ties for UK medical science, including clinical and translational After discussion and negotiation, the MRC, Cancer Research research. UK (CRUK), the Wellcome Trust and University College London (UCL) created a partnership: CRUK’s London Research K E Y W O R D S : MRC , CRUK , Wellcome , Crick , UCL , King’s , Imperial Institute (LRI) would join the NIMR, with researchers from UCL contributing expertise in the physical and clinical sciences. Importantly, the Crick was not simply to be a merger The Francis Crick Institute has been referred to as the most of LRI and NIMR but a new entity with a different ethos – a significant development in UK biomedical science for a multidisciplinary institute with a substantial new investment in generation. -

Cancer Research UK Submission to the European Commission Assessment of The
Cancer Research UK submission to the European Commission assessment of the January 2010 About Cancer Research UK Cancer Research UK (CR-UK)1 is leading the world in finding new ways to prevent, diagnose and independent funder of cancer research in Europe. Over half of all cancer research in the UK is carried out by our doctors and scientists. Cancer Re s entirely funded by the public and in 2008/09 we spent £355 million on research, supporting the work of more than 4,500 scientists, doctors and nurses. CR-UK funds research into all aspects of cancer from exploratory biology to clinical trials of novel and existing drugs as well as population-based studies and prevention research. Our scientists, doctors and nurses have contributed to the development of 19 of the top 20 drugs used to treat cancer patients worldwide today. At CR-UK we are involved with all stages of clinical trials, and we have a perspective both as a funder of academics conducting trials and as a Sponsor of early phase trials. For further information about our involvement in clinical trials, please see appendix 1. For further information about the implementation of the Clinical Trials Directive (CTD) in the UK, please see appendix 2. For a glossary of terms used throughout this response, please see appendix 3. Acknowledgements Our response has been collated following internal staff discussion and with contributions from the follow additional groups/individuals: Cancer Research UK Clinical Trials Unit, University of Birmingham Charles Coombes, Director, Department of Oncology, -

Uracil DNA Glycosylase (UDG) Sugar, Leaving an Abasic Site in Uracil-Containing Single Or Double-Stranded DNA
Product Specifications G5010L Rev F Product Description: Uracil-DNA Glycosylase catalyzes the Product Information hydrolysis of the N-glycosylic bond between the uracil and sugar, leaving an abasic site in uracil-containing single or Uracil DNA Glycosylase (UDG) double-stranded DNA. The enzyme shows no measurable Part Number G5010L activity on short oligonucleotides (<6 bases), or RNA substrates. Concentration 2,000 U/mL Unit Size 10,000 U Storage Temperature -25⁰C to -15⁰C Product Specifications G5010 Specific SS DS E. coli DNA Assay SDS Purity DS Exonuclease Activity Exonuclease Endonuclease Contamination Units Tested n/a n/a 100 100 100 100 >99% 77,000 U/mg <5.0% <1.0% No Conversion <10 copies Specification Released Released Source of Protein: A recombinant E. coli strain carrying the Uracil DNA Glycosylase gene from E. coli K-12. Unit Definition: 1 unit is defined as the amount of enzyme that catalyzes the release of 1.8 nmol of Uracil in 30 minutes from double-stranded, tritiated, Uracil containing-DNA at 37°C in 1X UDG Reaction Buffer. Molecular weight: 25,693 Daltons Quality Control Analysis: Unit Activity is measured using a 2-fold serial dilution method. Dilutions of enzyme were made in 1X reaction buffer and added to 50 µL reactions containing a 3H-dUTP PCR product and 1X UDG Reaction Buffer. Reactions were incubated for 10 minutes at 37°C, plunged on ice, and analyzed using a TCA-precipitation methods. Protein Concentration (OD 280 ) is determined by OD 280 absorbance. Physical Purity is evaluated by SDS-PAGE of concentrated and diluted enzyme solutions followed by silver stain detection. -

April 28 Sir Paul Nurse
MONDAY, APRIL 26th 8 pm We look forward to welcoming to Kenton SIR PAUL NURSE RATHER THAN GIVE A TALK, WE ARE VERY FORTUNATE IN THAT SIR PAUL IS HAPPY TO ANSWER QUESTIONS ON HIS EXTENSIVE CAREER AND HOBBIES PLEASE HAVE YOUR QUESTIONS READY OR SEND THEM IN BEFORE THE MEETING Paul Nurse is a geneticist and cell biologist who has worked on how the eukaryotic cell cycle is controlled. His major work has been on the cyclin dependent protein kinases and how they regulate cell reproduction. He is Director of the Francis Crick Institute in London, and has served as President of the Royal Society, Chief Executive of Cancer Research UK and President of Rockefeller University. He shared the 2001 Nobel Prize in Physiology or Medicine and has received the Albert Lasker Award, the Gairdner Award, the Louis Jeantet Prize and the Royal Society's Royal and Copley Medals. He was knighted by The Queen in 1999, received the Legion d'honneur in 2003 from France, and the Order of the Rising Sun in 2018 from Japan. He served for 15 years on the Council of Science and Technology, advising the Prime Minister and Cabinet, and is presently a Chief Scientific Advisor for the European Union. As well as his many medical accomplishments, amazingly Paul also has time to fly planes and engage in varied hobbies Paul flies gliders and vintage aeroplanes and has been a qualified bush pilot. He also likes the theatre, hill-walking, going to museums and art galleries, and running very slowly. All our Zoom sessions are available on the Kenton https://us02web.zoom.us/j/3531782577? YouTube channel: pwd=N0tlSWxxUGZmOEUrM1ZzclJFN1pzdz09 Kenton Shul In The Park Goes Live. -

3-Methyladenine DNA Glycosylases: Structure, Function, and Biological Importance Michael D
Review articles 3-Methyladenine DNA glycosylases: structure, function, and biological importance Michael D. Wyatt,1 James M. Allan,1 Albert Y. Lau,2 Tom E. Ellenberger,2 and Leona D. Samson1* Summary The genome continuously suffers damage due to its reactivity with chemical and physical agents. Finding such damage in genomes (that can be several million to several billion nucleotide base pairs in size) is a seemingly daunting task. 3-Methyladenine DNA glycosylases can initiate the base excision repair (BER) of an extraordinarily wide range of substrate bases. The advantage of such broad substrate recognition is that these enzymes provide resistance to a wide variety of DNA damaging agents; however, under certain circumstances, the eclectic nature of these enzymes can confer some biological disadvantages. Solving the X-ray crystal struc- tures of two 3-methyladenine DNA glycosylases, and creating cells and animals altered for this activity, contributes to our understanding of their enzyme mechanism and how such enzymes influence the biological response of organisms to several different types of DNA damage. BioEssays 21:668–676, 1999. 1999 John Wiley & Sons, Inc. Introduction ately interpreted by DNA-processing enzymes. Unfortunately, DNA carries life’s genetic information encoded in the arrange- these bases are also chemically reactive, and the inevitable ment of bases along the length of the DNA molecule. Each base modifications produce a variety of biological outcomes, DNA base has a distinct chemical structure that is appropri- depending on how a cell recognizes and responds to the modification. Cellular DNA repair mechanisms target these inappropriate DNA structures, and play a vital role in maintain- 1Department of Cancer Cell Biology, Harvard School of Public Health, ing genomic integrity. -

(12) United States Patent (10) Patent No.: US 9,689,046 B2 Mayall Et Al
USOO9689046B2 (12) United States Patent (10) Patent No.: US 9,689,046 B2 Mayall et al. (45) Date of Patent: Jun. 27, 2017 (54) SYSTEM AND METHODS FOR THE FOREIGN PATENT DOCUMENTS DETECTION OF MULTIPLE CHEMICAL WO O125472 A1 4/2001 COMPOUNDS WO O169245 A2 9, 2001 (71) Applicants: Robert Matthew Mayall, Calgary (CA); Emily Candice Hicks, Calgary OTHER PUBLICATIONS (CA); Margaret Mary-Flora Bebeselea, A. et al., “Electrochemical Degradation and Determina Renaud-Young, Calgary (CA); David tion of 4-Nitrophenol Using Multiple Pulsed Amperometry at Christopher Lloyd, Calgary (CA); Lisa Graphite Based Electrodes', Chem. Bull. “Politehnica” Univ. Kara Oberding, Calgary (CA); Iain (Timisoara), vol. 53(67), 1-2, 2008. Fraser Scotney George, Calgary (CA) Ben-Yoav. H. et al., “A whole cell electrochemical biosensor for water genotoxicity bio-detection”. Electrochimica Acta, 2009, 54(25), 6113-6118. (72) Inventors: Robert Matthew Mayall, Calgary Biran, I. et al., “On-line monitoring of gene expression'. Microbi (CA); Emily Candice Hicks, Calgary ology (Reading, England), 1999, 145 (Pt 8), 2129-2133. (CA); Margaret Mary-Flora Da Silva, P.S. et al., “Electrochemical Behavior of Hydroquinone Renaud-Young, Calgary (CA); David and Catechol at a Silsesquioxane-Modified Carbon Paste Elec trode'. J. Braz. Chem. Soc., vol. 24, No. 4, 695-699, 2013. Christopher Lloyd, Calgary (CA); Lisa Enache, T. A. & Oliveira-Brett, A. M., "Phenol and Para-Substituted Kara Oberding, Calgary (CA); Iain Phenols Electrochemical Oxidation Pathways”, Journal of Fraser Scotney George, Calgary (CA) Electroanalytical Chemistry, 2011, 1-35. Etesami, M. et al., “Electrooxidation of hydroquinone on simply prepared Au-Pt bimetallic nanoparticles'. Science China, Chem (73) Assignee: FREDSENSE TECHNOLOGIES istry, vol. -
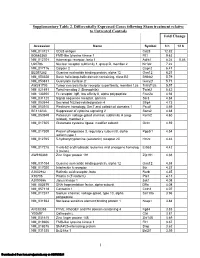
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

Biochemical Characterization and Mutational Studies of a Novel 3
Biochemical characterization and mutational studies of a novel 3-methlyadenine DNA glycosylase II from the hyperthermophilic Thermococcus gammatolerans Donghao Jiang, Likui Zhang, Kunming Dong, Yong Gong, Philippe Oger To cite this version: Donghao Jiang, Likui Zhang, Kunming Dong, Yong Gong, Philippe Oger. Biochemical characteriza- tion and mutational studies of a novel 3-methlyadenine DNA glycosylase II from the hyperthermophilic Thermococcus gammatolerans. DNA Repair, Elsevier, 2021. hal-03035060 HAL Id: hal-03035060 https://hal.archives-ouvertes.fr/hal-03035060 Submitted on 2 Dec 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. REVISED Manuscript (text UNmarked) Biochemical characterization and mutational studies of a novel 3-methlyadenine DNA glycosylase II from the hyperthermophilic Thermococcus gammatolerans Donghao Jianga, Likui Zhanga,b#, Kunming Donga, Yong Gongc# and Philippe Ogerd# aMarine Science & Technology Institute, College of Environmental Science and Engineering, Yangzhou University, China bGuangling College, Yangzhou University, China cBeijing Synchrotron Radiation Facility, Institute of High Energy Physics, Chinese Academy of Sciences, China dUniv Lyon, INSA de Lyon, CNRS UMR 5240, Lyon, France The first corresponding author: Dr. Likui Zhang E-mail address: [email protected] Tel: +86-514-89795882 Fax: +86-514-87357891 Corresponding author: Dr.