Systematic Review and Economic Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Riffa House Farm Harrogate Road Leathley Lifestyledetached Benefit Family Homepull out Statementwith Breath Can Taking Go to Viewstwo Orand Three Land Lines
Riffa House Farm Harrogate Road Leathley LifestyleDetached benefit family homepull out statementwith breath can taking go to viewstwo orand three land lines.. XXX35 2 X FirstRiffa Houseparagraph, Farm editorial is an impressive style, short, detached considered country headline home 11.23 benefitsoffering excellent of living accommodationhere. One or two sentencesover two floors that andconvey perfectly what youpositioned would say with in far person. reaching views across open countryside. SecondOccupying paragraph, a generous additional and private details plot of withnote eleven about theacres of good property.grass land. Wording The property to add isvalue ideal and for supportthe commuter image selection.with excellent Temroad volumlinks to is Harrogate, solor si aliquation Leeds, Yorkrempore and thepuditiunto A1. qui utatis adit, animporepro experit et dolupta ssuntio mos apieturere ommosti squiati busdaecus cus dolorporum volutem Internal Page1 Single Pic Inset FirstUpon paragraph,entry this fantastic editorial familystyle, home short, extends considered to over headline 2,800 sq ft benefitsof internal of accommodation living here. One andor two in briefsentences comprises; that convey vestibule, what a youwelcoming would say reception in person. hall, dual aspect sitting room spanning the width of the ground floor and log burning stove. To the right of the Secondhallway isparagraph, a home office, additional separate details dining of note room about with the double doors property. Wording to add value and support image selection. allowing access to the the triple aspect dining kitchen - fitted with Tem volum is solor si aliquation rempore puditiunto qui utatis adit,log burning animporepro stove. experitW/C and et separate dolupta ssuntio utility room mos areapieturere accessed off ommostianother hallway squiati which busdaecus also provides cus dolorporum access to volutem. -
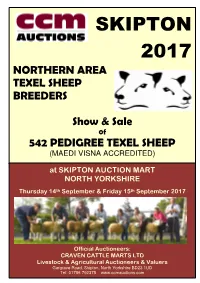
Skipton 2017
SKIPTON 2017 NORTHERN AREA TEXEL SHEEP BREEDERS Show & Sale 0f 542 PEDIGREE TEXEL SHEEP (MAEDI VISNA ACCREDITED) at SKIPTON AUCTION MART NORTH YORKSHIRE th th Thursday 14 September & Friday 15 September 2017 Official Auctioneers: CRAVEN CATTLE MARTS LTD Livestock & Agricultural Auctioneers & Valuers Gargrave Road, Skipton, North Yorkshire BD23 1UD Tel: 01756 792375 www.ccmauctions.com Date received……………………… Number [ ] Northern Area Texel Sheep Breeders’ Club Membership Application Form The Committee of the NATSB has agreed to keep a waiting list of prospective members who reside outside the club area, and therefore are not eligible for automatic membership. If you live OUTSIDE the Club postal code areas, which are: NE/ SR/ DH/ DL/ TS/ BD/ HG/ YO/ LS/ HU/ HD/ HX/ WF/ DN you may apply to be placed onto the waiting list. Please note: 1. No application is guaranteed membership status either now or in the future. 2. Applications will only be accepted on this form. No phone, fax or email applications. 3. Applications will be placed in strict order of receipt onto a waiting list. NAME……………………………………………………………………… ADDRESS………………………………………………………………… ……………………………………………………………………………… ……………………………………………………………………………… POSTCODE………………………….... TEL(inc.STD)………………..………… SIGNED………………………………………………………… Please tear out the form, complete and return by post to the Secretary: c/o Pear Tree Farm, Battersby, Gt. Ayton, North Yorkshire TS9 6LU NORTHERN AREA TEXEL SHEEP BREEDERS TEXEL SALE 2017 PROGRAMME THURSDAY 14th SEPTEMBER INSPECTION (ALL SHEEP) STRICTLY 9.30am – 12.00noon -

Washburn & Mid-Wharfe United Benefice Hon Assistant Clergy
Washburn & Mid-Wharfe Methodist Ministers for United Benefice Farnley, Fewston with Blubberhouses, Norwood & Timble Leathley, Weston with Denton. Rev Shannon DeLaureal Rector: Revd Stephen McCaulay 01943 430345 The Vicarage, Askwith LS21 2HX [email protected] Tel: 01943 513340 [email protected] Rev Tim Perkins 20 Far Mead Croft, Burley in Wharfedale. LS29 7RR Hon Assistant Clergy 01943 864187 The Revd Michael Cleverley [email protected] Tel: 01943 851234 The Revd Stewart Hartley Norwood Retreat Centre Tel: 01943 464106 Norwood, Otley LS21 2RA, Email: [email protected] Tel: 07946 423309 Lent The Revd Barry Miller Tel: 01943 467641 [email protected] Methodist Chapels are in the circuit of Wharfedale & Aireborough Readers John Charman, Norwood Hall Cottage, Norwood LS21 2RA Websites: Tel: 01943 466712 St Oswalds Church, Leathley Peter Wiggins, 32 Manley Road, Ben www.leathleychurch.org Rhydding, Ilkley LS29 8QP Farnley Church Tel: 01943 609599 www.farnleyallsaints.org Fewston and Blubberhouses www.fewstonwithblubberhouses.org.uk Churchwardens Weston Church Blubberhouses: Pat Anderson www.westonchurch.wordpress.com Tel: 01943 880284 Norwood Retreat Centre Denton Ann Chadwick www.yorkshirewestmethodist.org.uk/ 01943 600 604. people-places/norwood-retreat-centre Farnley: Peter Goodwin Tel: 01943 969953 Benefice Administrator Fewston: Cheri Beaumont Hazel Pullan Tel: 01943 465977 Hours Mon, Weds, Fri, 9.30-11.30am Leathley: Terry Bramall CBE [email protected] Tel: 07802 877799 01943 466098 & Liz Webster 01943 468376 Weston: Ann Chadwick 01943 600 604. Our Magazine Front cover image Please see page 25. If you would like to contribute, advertise or Title: St Oswald's Church Leathley Church subscribe, to the magazine. -

Washburn Heritage Centre Archive Handlist
WASHBURN HERITAGE CENTRE ARCHIVE HANDLIST The WHC Archive is a specialist collection of photographs, film, video and sound recordings, documents, memorabilia and ephemera relevant to the History, Heritage and Environment of the Washburn Valley. Our work to catalogue the collections is ongoing and this handlist will change as more of our current collections are catalogued. Please email us if you have a specific enquiry not covered by this handlist. The General Collections include: DOC Documents held by the centre either virtually and/or physically EX Past Exhibition panels PRI printed materials held in the centre RES Research materials including documents and notes on: RESVAR-Vernacular Architecture RESSOC-Social History RESNAT-The Natural World RESIND- Industry RESCHU- Churches and Chapels RESARCH-Archaeology RESWAT-Waterways and Bridges MAP Digital images of maps of the area including ordnance survey maps. PHO Photographs on various themes of interest to the local area including: PHOCHUR-churches and chapels PHOHIST- general history PHONAT-the natural World PHOHIST-general history () PHOWAR-War PHOLIP-Landscape, Industry and Places () PHOWHC-General events at Washburn Heritage centre, including the building and opening of the Centre VID - series of OHP films including: War memories, Water and leisure, Working wood, working Washburn, Haymaking-Washburn Show, Schools, Memories Day-launch of the OHP WHC-Opening Ceremony. · The special collections include: ARCH and - PHOFEW Fewston Assemblage-the archaeology reports and images of the finds PHOALH Alex Houseman Collection- images of the Washburn valley donated by Alex Houseman Ruth Brown Collection - includes images of the local area and a scrapbook of PHOBRO information on the Tuly and Peel families. -

X52 Bus Time Schedule & Line Route
X52 bus time schedule & line map X52 Harrogate <-> Ilkley View In Website Mode The X52 bus line (Harrogate <-> Ilkley) has 4 routes. For regular weekdays, their operation hours are: (1) Harrogate <-> Ilkley: 8:30 AM - 4:30 PM (2) Harrogate <-> Otley: 5:30 PM (3) Ilkley <-> Harrogate: 9:25 AM - 5:25 PM (4) Otley <-> Harrogate: 7:50 AM - 8:50 AM Use the Moovit App to ƒnd the closest X52 bus station near you and ƒnd out when is the next X52 bus arriving. Direction: Harrogate <-> Ilkley X52 bus Time Schedule 52 stops Harrogate <-> Ilkley Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 8:30 AM - 4:30 PM Hgte Bus Stn Stand 6, Harrogate Station Parade, Harrogate Tuesday 8:30 AM - 4:30 PM The Odeon, Harrogate Wednesday 8:30 AM - 4:30 PM Station Avenue, Harrogate Thursday 8:30 AM - 4:30 PM Queen Parade, Harrogate Friday 8:30 AM - 4:30 PM Slingsby Walk, Harrogate Saturday 8:30 AM - 4:30 PM St Aidans School, Harrogate Coach Road, Oatlands X52 bus Info Hornbeam Crescent, Oatlands Direction: Harrogate <-> Ilkley Stops: 52 Mount Gardens, Oatlands Trip Duration: 50 min Line Summary: Hgte Bus Stn Stand 6, Harrogate, Coronation Avenue, Oatlands The Odeon, Harrogate, Queen Parade, Harrogate, Slingsby Walk, Harrogate, St Aidans School, 27 Hookstone Road, Harrogate Harrogate, Coach Road, Oatlands, Hornbeam Appleyards, Oatlands Crescent, Oatlands, Mount Gardens, Oatlands, Coronation Avenue, Oatlands, Appleyards, Oatlands, Firs Avenue, Fulwith, Fulwith Mill Lane, Fulwith, Firs Avenue, Fulwith Cragside Garage, Spacey Houses, The Garage, Spacey -

Moorside Farmhouse, Stainburn, Near Harrogate, Ls21 2Lr
= MOORSIDE FARMHOUSE, STAINBURN, NEAR HARROGATE, LS21 2LR GUIDE PRICE £925,000 MOORSIDE FARMHOUSE Stainburn, Near Harrogate, LS21 2LR A beautifully presented detached family home enjoying stunning, unrivalled long-distance views with a self-contained annexe, occupying a plot extending to over TWO ACRES with paddock, barns and outbuildings, with potential for further development, subject to obtaining the necessary consents. This individual property offers flexible and generous accommodation, with the main house providing four reception rooms, kitchen, utility and three bedrooms. The main house links to a self-contained annexe with separate kitchen, sitting room and bedroom, making it ideal for home buyers who wish accommodate elderly relatives or grow-up children, or simply to produce an income by renting out the accommodation separately. The property also has the benefit of substantial outbuildings. This attractive and most convenient location is just a five-minute drive from the popular village of Beckwithshaw and ten minutes from Harrogate, being well place for daily commuting to Yorkshire’s principal business districts. Main House: 4 reception rooms · breakfast kitchen · cloakroom · utility room · 3 bedrooms · bathroom Annexe Accommodation: separate kitchen, living room, bedroom and shower room Extensive Grounds extending to over 2 acres including gardens, paddock, extensive outbuildings and stunning views ACCOMMODATION Setting Main House Annexe The property stands within The front door leads to a The main house links to attractive lawned grounds and spacious reception hall, which a potential self-contained gardens extending in total to in turn gives access to four annexe, with a well-equipped over two acres, with unrivalled reception rooms, all enjoying kitchen on the ground floor, views across the adjoining long-distance views. -

Stainburn Lane, Leathley Guide Price: £100,000
Stainburn Lane, Leathley Guide Price: £100,000 Stainburn Lane Leathley LS21 2LF GEORGIAN DETACHED GRADE II* LISTED FORMER CHAPEL WITH BEAUTIFUL VIEWS ACROSS OPEN COUNTRYSIDE Offered for sale with NO ONWARD CHAIN is this stone built former chapel with a Grade II* Listing, which has been used in more recent times as a meeting room and concert venue. Enclosed by stone walling, their is a small paved courtyard affording picturesque views over the adjoining countryside. Our clients ideally would like unconditional offers but are willing to consider conditional offers, i.e subject to gaining listed building planning approval. BEST OFFERS ARE INVITED IN WRITING BY 12 NOON ON WEDNESDAY 18TH NOVEMBER 2015 TO DALE EDDISON'S OTLEY OFFICE INTERNAL MEASUREMENTS 27' x 19' (8.23m x 5.79m) The property is registered with Historic England. Methodist Church and Retaining Wall with Gate and Steps. List Entry Summary This building is listed under the planning (Listed Buildings and Conservation Areas) Act 1990 as amended for its special architectural or historic interest List Entry Number 1150014 * Please indicate in your offer whether finance is available for the purchase or whether funding has County: North Yorkshire yet to be arranged. If your bid is accepted by the District: Harrogate vendors this will be subject to providing Dale District Type: District Authority Eddison with proof of funding with immediate Parish: Leathley effect. Grade: II* * All offers must clearly identify the name and address of the proposed purchaser and the name Date First Listed: 22-Feb-1985 and address of their solicitors. SERVICES: We have not made specific enquiries as FOR FURTHER INFORMATION PLEASE VISIT to the mains services to this property. -

Cause Papers Project Standardization
1 Cause Papers in the Diocesan Courts of the Archbishopric of York, 1300–1858 Editing and Standardisation in the Cause Papers Database The Cause Papers project provided an on-line searchable catalogue of more than 13,000 cause papers relating to cases heard between 1300 and 1858 in the Church Courts of the diocese of York, the original records for which are held at the Borthwick Institute for Archives at the University of York. The project aimed to pioneer a new standard of excellence in data accuracy and standardization. Cataloguing such a large and varied number of records posed numerous challenges in these areas, including the problem of how to incorporate spelling and language variations of surname and place names. The following document provides information on the methods used by the project team in compiling, editing and standardizing the data. It is split into the following sections:- 1) Information provided by the database 2) List of standard reference works used by the project team 3) List of types and sub-types of cases commonly used in the database 4) Standardization of Forenames 5) Standardization of Surnames – Part A 6) Standardization of Surnames – Part B 7) Problematic Place-names – Identification and Standardization Please note that this text is not intended as a guide to on-line catalogue. Users requiring assistance with searching the catalogue should consult the on-screen help text. 2 Editing and standardisation for the Cause Paper Database 1) Information provided by the database Owing to the volume and complexity of manuscript material involved, it was not possible to provide full transcriptions of the cause papers. -

Neighbourhood Plan 2019-2028
POOL-IN-WHARFEDALE NEIGHBOURHOOD PLAN 2019-2028 PRE-SUBMISSION PLAN DRAFT VERSION 8.3 29 April 2019 1 Contents FOREWORD ............................................................................................................................................. 6 1. Introduction ........................................................................................................................................ 8 2. The Neighbourhood Plan Area – Yesterday and Today ...................................................................... 9 3. The Neighbourhood Plan Preparation Process ................................................................................. 10 4. The Vision and Objectives for Pool-in-Wharfedale ........................................................................... 13 5. The Plan Policies and Community Actions ........................................................................................ 15 5.1 Green Environment ..................................................................................................................... 15 Introduction .................................................................................................................................. 15 Otley Chevin and Wharfe Valley Southern Slopes Special Landscape Areas ................................ 15 Local Green Infrastructure ............................................................................................................ 16 Protection of Local Green Space .................................................................................................. -

Otter, Pine Marten, Stoat, Weasel, Polecat, American Mink, Wildcat and Domestic Cat
Changes in the status and distribution of mammals of the order Carnivora in Yorkshire from 1600. County history of the fox, badger, otter, pine marten, stoat, weasel, polecat, American mink, wildcat and domestic cat. Item Type Thesis Authors Howes, Colin Anthony Rights <a rel="license" href="http://creativecommons.org/licenses/ by-nc-nd/3.0/"><img alt="Creative Commons License" style="border-width:0" src="http://i.creativecommons.org/l/by- nc-nd/3.0/88x31.png" /></a><br />The University of Bradford theses are licenced under a <a rel="license" href="http:// creativecommons.org/licenses/by-nc-nd/3.0/">Creative Commons Licence</a>. Download date 30/09/2021 16:30:47 Link to Item http://hdl.handle.net/10454/4306 CHAPTER 5 OTTER (Lutra lutra L.) Introduction A programme of regional historical studies of otter status, distribution and persecution pressures has been undertaken to provide a background to current monitoring of the otter (Lutra lutra L.) in river catchments, drain network systems and still waters of the Yorkshire and Humber region. An archive of over 750 historical and current otter records up to 2000 has been collated in Appendix 5.1 and displayed in Figure 5.1 to create a general distribution map covering all Yorkshire river catchments. Otter 3 2 1 0 9 8 7 6 5 4 3 2 1 0 9 pre 19th century 19th century 8 1900-1954 1955 onwards 6 7 8 9 0 1 2 3 4 5 6 7 8 9 0 1 2 3 4 5 Figure 5.1. Historical distribution map of otters throughout Yorkshire. -

Public Notices 2
11922 THE LONDON GAZETTE, 31sT AUGUST 1976 20. Holbeck from Gilling East, Gilling East Parish, 49. The River Rother and Barlow Brook, from Hasland together with Wath Beck from Slingsby Parish, to the Parish, North East Derbyshire District to Chesterfield, River Rye near Brawby, Brawby Parish, Ryedale District, Chesterfield Borough, Derbyshire. North Yorkshire. 50. The River Doe Lea, from Bramley Vale, Ault 21. Thornton Beck, from near Thorntoni Dale, Thornton Hucknall Parish, Bolsover District to near Renishaw, Dale Parish, Ryedale District, North Yorkshire. Staveley Parish, Chesterfield Borough, Derbyshire. 22. The River Worth, Keighley, Bradford City, West Plans bearing the reference YA/YOA2 on which the pro- Yorkshire. posals are more precisely defined by lines in green colour 23. The River Calder together with Walsden Water, Tod- (additions) are available for public inspection at the offices morden Parish, Calderdale Borough, West Yorkshire. of the Chief Executive, Richmondshire District Council, 24. The River Washburn, from Lindley Green, Lindley Swale House, Frenchgate, Richmond, North Yorkshire, Parish, to beyond Leathley Bridge, Leathley Parish, Harro- DL10 4JE (items 1-5) ; at the offices of the Chief Executive, gate Borough, North Yorkshire.- North Yorkshire County Council, County Hall, Northaller- 25. The River Spen from Cleckheaton to Dewsbury, ton, North Yorkshire, DL7 8AD (items 3-6 and 13) ; at Kirklees Borough, West Yorkshire. the offices of the Chief Executive, Craven District Council, 26. The River Colne, Huddersfield, together with Fenay Council Offices, Granville Street, Skipton, North Yorkshire, Brook, Kirkburton Parish, Kirklees Borough, West York- BD23 IPS (item 9) ; at the offices of the Chief Executive shire. Scarborough Borough Council, Town Hall, St. -

(West Yorkshire)………
LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND REVIEW OF WEST YORKSHIRE THE CITY OF LEEDS Boundaries with:- HARROGATE & SELBY (NORTH YORKSHIRE) HARROGATE BRADFORD SELBY REPORT NO.606 LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND REPORT NO 606 LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND CHAIRMAN Mr G J Ellerton MEMBERS Mr K F J Ennals Mr G Prentice Mrs H R V Sarkany Mr C W Smith Professor K Young THE RT HON MICHAEL HESELTINE MP SECRETARY OF STATE FOR THE ENVIRONMENT REVIEW OF WEST YORKSHIRE THE CITY OF LEEDS AND ITS BOUNDARIES WITH HARROGATE AND SELBY IN NORTH YORKSHIRE COMMISSION'S FINAL REPORT INTRODUCTION 1. On 1 September 1987 we wrote to Leeds city Council announcing our intention to undertake a review of Leeds as part of our review of the Metropolitan County of West Yorkshire and its Metropolitan Districts under section 48(1) of the Local Government Act 1972. Copies of our letter were sent to the adjoining Metropolitan District Councils; the County and District Councils bordering the Metropolitan County; Parish Councils in the adjoining districts; the Local Authority Associations; Members of Parliament with constituency interests; and the headquarters of the main political parties. In addition, copies were sent to those government departments, regional health authorities and statutory undertakers which might have an interest, as well as to the English Tourist Board, the local- press, and the local television and radio stations serving the area. 2. The Metropolitan District Councils were requested, in co-operation as necessary with the other principal authorities, to assist us in publishing the start of the review by inserting a notice for two successive weeks in local newspapers, so as to give a wide coverage in the areas concerned.