Procedure Guideline for Somatostatin Receptor Scintigraphy with 111In-Pentetreotide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Novel Drug-Like Somatostatin Receptor 4 Agonists Are Potential Analgesics for Neuropathic Pain
International Journal of Molecular Sciences Article Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain 1,2, 3, 1,2 4 1,2 Boglárka Kántás y, Rita Börzsei y, Éva Sz˝oke ,Péter Bánhegyi , Ádám Horváth , 1,2 1,2 1 1,2, Ágnes Hunyady , Éva Borbély , Csaba Hetényi , Erika Pintér y and 1,2, , Zsuzsanna Helyes * y 1 Department of Pharmacology and Pharmacotherapy, Medical School, University of Pécs, Szigeti str. 12, H-7624 Pécs, Hungary 2 Szentágothai Research Centre and Centre for Neuroscience, University of Pécs, Ifjúság str. 20, H-7624 Pécs, Hungary 3 Department of Pharmacology, Faculty of Pharmacy, University of Pécs, Szigeti str. 12, H-7624 Pécs, Hungary 4 Avicor Ltd., Herman Ottó str. 15, H-1022 Budapest, Hungary * Correspondence: [email protected] These authors contributed equally to this work. y Received: 14 October 2019; Accepted: 9 December 2019; Published: 11 December 2019 Abstract: Somatostatin released from the capsaicin-sensitive sensory nerves mediates analgesic and anti-inflammatory effects via the somatostatin sst4 receptor without endocrine actions. Therefore, sst4 is considered to be a novel target for drug development in pain including chronic neuropathy, which is an emerging unmet medical need. Here, we examined the in silico binding, the sst4-linked G-protein activation on stable receptor expressing cells (1 nM to 10 µM), and the effects of our novel pyrrolo-pyrimidine molecules in mouse inflammatory and neuropathic pain models. All four of the tested compounds (C1–C4) bind to the same binding site of the sst4 receptor with similar interaction energy to high-affinity reference sst4 agonists, and they all induce G-protein activation. -

Somatostatin Receptor Type 2A Immunohistochemistry in Neuroendocrine Tumors: a Proposal of Scoring System Correlated with Somatostatin Receptor Scintigraphy
Modern Pathology (2007) 20, 1172–1182 & 2007 USCAP, Inc All rights reserved 0893-3952/07 $30.00 www.modernpathology.org Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy Marco Volante1, Maria Pia Brizzi1, Antongiulio Faggiano2, Stefano La Rosa3, Ida Rapa1, Anna Ferrero1, Gelsomina Mansueto4, Luisella Righi1, Silvana Garancini5, Carlo Capella3, Gaetano De Rosa4, Luigi Dogliotti1, Annamaria Colao2 and Mauro Papotti1 1Department of Clinical and Biological Sciences, San Luigi Hospital, University of Turin, Orbassano, Turin, Italy; 2Department of Molecular and Clinical Endocrinology and Oncology, ‘Federico II’ University, Naples, Italy; 3Section of Anatomic Pathology, Department of Human Morphology, University of Insubria and Ospedale di Circolo, Varese, Italy; 4Department of General Pathology, Medicine, Human Pathology and Clinical Pathology, University of Naples ‘Federico II’, Naples, Italy and 5Department of Nuclear Medicine, Ospedale di Circolo, Varese, Italy Typing somatostatin receptor expression in neuroendocrine tumors is of relevance to target somatostatin analogue-based diagnostic approach and treatment. The expanding use of immunohistochemistry to detect somatostatin receptors is to date not paralleled by an accurate methodological setting and standardized interpretation of the results. A multicentric study was designed to compare somatostatin receptor immunohistochemical expression with in vivo scintigraphic data and verify its usefulness in the clinical management of neuroendocrine tumors. After methodological setting by testing different somatostatin receptor antibodies, 107 cases of neuroendocrine tumors with available somatostatin receptor scintigraphy data and pathological material were retrospectively analyzed for somatostatin receptor types 2A, 3 and 5 immunohis- tochemical expression, and compared with scintigraphic images and, whenever available, with the clinical response to somatostatin analogue treatment. -

Targeting Neuropeptide Receptors for Cancer Imaging and Therapy: Perspectives with Bombesin, Neurotensin, and Neuropeptide-Y Receptors
Journal of Nuclear Medicine, published on September 4, 2014 as doi:10.2967/jnumed.114.142000 CONTINUING EDUCATION Targeting Neuropeptide Receptors for Cancer Imaging and Therapy: Perspectives with Bombesin, Neurotensin, and Neuropeptide-Y Receptors Clément Morgat1–3, Anil Kumar Mishra2–4, Raunak Varshney4, Michèle Allard1,2,5, Philippe Fernandez1–3, and Elif Hindié1–3 1CHU de Bordeaux, Service de Médecine Nucléaire, Bordeaux, France; 2University of Bordeaux, INCIA, UMR 5287, Talence, France; 3CNRS, INCIA, UMR 5287, Talence, France; 4Division of Cyclotron and Radiopharmaceutical Sciences, Institute of Nuclear Medicine and Allied Sciences, DRDO, New Delhi, India; and 5EPHE, Bordeaux, France Learning Objectives: On successful completion of this activity, participants should be able to list and discuss (1) the presence of bombesin receptors, neurotensin receptors, or neuropeptide-Y receptors in some major tumors; (2) the perspectives offered by radiolabeled peptides targeting these receptors for imaging and therapy; and (3) the choice between agonists and antagonists for tumor targeting and the relevance of various PET radionuclides for molecular imaging. Financial Disclosure: The authors of this article have indicated no relevant relationships that could be perceived as a real or apparent conflict of interest. CME Credit: SNMMI is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing education for physicians. SNMMI designates each JNM continuing education article for a maximum of 2.0 AMA PRA Category 1 Credits. Physicians should claim only credit commensurate with the extent of their participation in the activity. For CE credit, SAM, and other credit types, participants can access this activity through the SNMMI website (http://www.snmmilearningcenter.org) through October 2017. -

Identification of Neuropeptide Receptors Expressed By
RESEARCH ARTICLE Identification of Neuropeptide Receptors Expressed by Melanin-Concentrating Hormone Neurons Gregory S. Parks,1,2 Lien Wang,1 Zhiwei Wang,1 and Olivier Civelli1,2,3* 1Department of Pharmacology, University of California Irvine, Irvine, California 92697 2Department of Developmental and Cell Biology, University of California Irvine, Irvine, California 92697 3Department of Pharmaceutical Sciences, University of California Irvine, Irvine, California 92697 ABSTRACT the MCH system or demonstrated high expression lev- Melanin-concentrating hormone (MCH) is a 19-amino- els in the LH and ZI, were tested to determine whether acid cyclic neuropeptide that acts in rodents via the they are expressed by MCH neurons. Overall, 11 neuro- MCH receptor 1 (MCHR1) to regulate a wide variety of peptide receptors were found to exhibit significant physiological functions. MCH is produced by a distinct colocalization with MCH neurons: nociceptin/orphanin population of neurons located in the lateral hypothala- FQ opioid receptor (NOP), MCHR1, both orexin recep- mus (LH) and zona incerta (ZI), but MCHR1 mRNA is tors (ORX), somatostatin receptors 1 and 2 (SSTR1, widely expressed throughout the brain. The physiologi- SSTR2), kisspeptin recepotor (KissR1), neurotensin cal responses and behaviors regulated by the MCH sys- receptor 1 (NTSR1), neuropeptide S receptor (NPSR), tem have been investigated, but less is known about cholecystokinin receptor A (CCKAR), and the j-opioid how MCH neurons are regulated. The effects of most receptor (KOR). Among these receptors, six have never classical neurotransmitters on MCH neurons have been before been linked to the MCH system. Surprisingly, studied, but those of most neuropeptides are poorly several receptors thought to regulate MCH neurons dis- understood. -

Current Status of Radiopharmaceuticals for the Theranostics of Neuroendocrine Neoplasms
Review Current Status of Radiopharmaceuticals for the Theranostics of Neuroendocrine Neoplasms Melpomeni Fani 1,*, Petra Kolenc Peitl 2 and Irina Velikyan 3 1 Division of Radiopharmaceutical Chemistry, University Hospital of Basel, 4031 Basel, Switzerland; [email protected] 2 Department of Nuclear Medicine, University Medical Centre Ljubljana, 1000 Ljubljana, Slovenia; [email protected] 3 Department of Medicinal Chemistry, Uppsala University, 751 23 Uppsala, Sweden; [email protected] * Correspondence: [email protected]; Tel.: +41-61-556-58-91; Fax: +41-61-265-49-25 Academic Editor: Klaus Kopka Received: 7 February 2017; Accepted: 9 March 2017; Published: 15 March 2017 Abstract: Nuclear medicine plays a pivotal role in the management of patients affected by neuroendocrine neoplasms (NENs). Radiolabeled somatostatin receptor analogs are by far the most advanced radiopharmaceuticals for diagnosis and therapy (radiotheranostics) of NENs. Their clinical success emerged receptor-targeted radiolabeled peptides as an important class of radiopharmaceuticals and it paved the way for the investigation of other radioligand-receptor systems. Besides the somatostatin receptors (sstr), other receptors have also been linked to NENs and quite a number of potential radiolabeled peptides have been derived from them. The Glucagon- Like Peptide-1 Receptor (GLP-1R) is highly expressed in benign insulinomas, the Cholecystokinin 2 (CCK2)/Gastrin receptor is expressed in different NENs, in particular medullary thyroid cancer, and the Glucose-dependent Insulinotropic Polypeptide (GIP) receptor was found to be expressed in gastrointestinal and bronchial NENs, where interestingly, it is present in most of the sstr-negative and GLP-1R-negative NENs. Also in the field of sstr targeting new discoveries brought into light an alternative approach with the use of radiolabeled somatostatin receptor antagonists, instead of the clinically used agonists. -

Development of a Universal High-Throughput Calcium Assay for G-Protein-Coupled Receptors with Promiscuous G-Protein Gα15/16
Acta Pharmacol Sin 2008 Apr; 29 (4): 507–516 Full-length article Development of a universal high-throughput calcium assay for G-pro- tein-coupled receptors with promiscuous G-protein Gα15/161 Ting ZHU2,4, Li-yan FANG2,3, Xin XIE2,3,5 2The National Center for Drug Screening, 3Shanghai Institute of Materia Medica, 4Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences, Shanghai 201203, China Key words Abstract G-protein-coupled receptors; G-protein; Aim: To develop a universal high-throughput screening assay based on Gα15/16- Gα15/16; high-throughput screening; mediated calcium mobilization for the identification of novel modulators of G- calcium assay; GTPγS binding protein-coupled receptors (GPCR). Methods: In the present study, CHO-K1 or 1Project supported by grants from the Chinese HEK293 cells were co-transfected with plasmids encoding promiscuous G-protein Academy of Sciences (No KSCX2-YW-R- Gα15/16 and various receptors originally coupled to Gαs, Gαi, or Gαq pathways. 18), the Ministry of Science and Technology of China (No 2006AA020602), and the Intracellular calcium change was monitored with fluorescent dye Fluo-4. Results: Shanghai Commission of Science and We found out for all the receptors tested, Gα15/16 could shift the receptors’ Technology (No 05PJ14313, 06DZ22907). coupling to the calcium mobilization pathway, and the EC50 values of the ligands 5Correspondence to Dr Xin XIE. Phn 86-21-5080-1313, ext 156. generated with this method were comparable with reported values that were ob- Fax 86-21-5080-0721. tained using traditional methods. This assay was validated and optimized with E-mail [email protected] the δ-opioid receptor, which originally coupled to Gαi and was recently found to play important roles in neurodegenerative and autoimmune diseases. -

26985.Full.Pdf
Regulating quantal size of neurotransmitter release through a GPCR voltage sensor Quanfeng Zhanga,1, Bing Liua,1, Yinglin Lia,1, Lili Yina, Muhammad Younusa, Xiaohan Jianga, Zhaohan Lina, Xiaoxuan Suna, Rong Huanga, Bin Liua, Qihui Wua, Feipeng Zhua, and Zhuan Zhoua,2 aState Key Laboratory of Membrane Biology and Beijing Key Laboratory of Cardiometabolic Molecular Medicine, Institute of Molecular Medicine and Peking-Tsinghua Center for Life Sciences and PKU-IDG/McGovern Institute for Brain Research, Peking University, 100871 Beijing, China Edited by Robert H. Edwards, University of California, San Francisco, CA, and approved September 11, 2020 (received for review March 25, 2020) Current models emphasize that membrane voltage (Vm) depolarization- ATP is the ligand of two families of purinergic receptors, P2Xs induced Ca2+ influx triggers the fusion of vesicles to the plasma and P2Ys. P2Xs are ion channels and P2Ys are GPCRs, in- membrane. In sympathetic adrenal chromaffin cells, activation of cluding Gq (P2Y1, 2, 4, 6, 11) and Gi types (P2Y12, 13, 14) (27, 28). a variety of G protein coupled receptors (GPCRs) can inhibit quantal Among the P2Ys, P2Y1 exists in most tissues, including epithelial size (QS) through the direct interaction of G protein Giβγ subunits and endothelial cells, platelets, and immune cells (27, 29), and with exocytosis fusion proteins. Here we report that, independently P2Y12 is strongly expressed on platelets, where it plays funda- from Ca2+, Vm (action potential) per se regulates the amount of mental roles in their activation and aggregation (28, 30, 31), as catecholamine released from each vesicle, the QS. The Vm regula- well as in microglia (32, 33), smooth muscle cells (34), and tion of QS was through ATP-activated GPCR-P2Y12 receptors. -
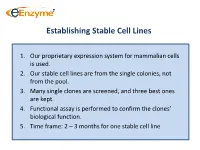
Establishing Stable Cell Lines
Establishing Stable Cell Lines 1. Our proprietary expression system for mammalian cells is used. 2. Our stable cell lines are from the single colonies, not from the pool. 3. Many single clones are screened, and three best ones are kept. 4. Functional assay is performed to confirm the clones’ biological function. 5. Time frame: 2 – 3 months for one stable cell line List of In-Stock ACTOne GPCR Stable Clones Transduced Gi-coupled receptors (22) Transduced Gs coupled receptors (34) Cannabinoid receptor 1 (CB1) Vasoactive Intestinal Peptide Receptor 2 (VIPR2) Dopamine Receptor 2 (DRD2) Melanocortin 4 Receptor (MC4R) Melanocortin 5 Receptor (MC5R) Somatostatin Receptor 5 (SSTR5) Parathyroid Hormone Receptor 1 (PTHR1) Adenosine A1 Receptor (ADORA1) Glucagon Receptor (GCGR) Chemokine (C-C motif) receptor 5 (CCR5) Dopamine Receptor 1 (DRD1) Melanin-concentrating Hormone Receptor 1 (MCHR1) Prostaglandin E Receptor 4 (EP4) Vasoactive Intestinal Peptide Receptor 1 (VIPR1) Cannabinoid receptor 2 (CB2) Gastric Inhibitor Peptide Receptor (GIPR) Glutamate receptor, metabotropic 8 (GRM8) Dopamine Receptor 5 (DRD5) Opioid receptor, kappa 1 (OPRK1) Parathyroid Hormone Receptor 2 (PTHR2) Adenosine A3 receptor (ADORA3) 5-hydroxytryptamine (serotonin) receptor 6 (HTR4) Corticotropin Releasing Hormone Receptor 2 (CRHR2) Glutamate receptor, metabotropic 8 (GRM8) Adenylate Cyclase Activating Polypeptide 1 Receptor type I (ADCYAP1R1) Neuropeptide Y Receptor Y1 (NPY1R) Secretin Receptor (SCTR) Neuropeptide Y Receptor Y2 (NPY2R) Follicle -

(Hsstr4) Agonist CNTX-0290 for Mixed Pain Conditions
407 Preclinical Evaluation of Human Somatostatin Receptor 4 (hSSTR4) Agonist CNTX-0290 for Mixed Pain Conditions Randall M. Stevens, MD1; Laura Corradini, PhD2; Henri Doods, PhD2 1Centrexion Therapeutics Corp, Boston, MA, USA; 2Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany ─ MED was 0.1 mg/kg, corresponding to a minimal effective Partial Nerve Ligation Model: Mononeuropathic Pain ● CNTX-0290 did not affect glucose tolerance (Figure 7), while Figure 5. CNTX-0290 Efficacy in the STZ Rat Model of INTRODUCTION Figure 1. Mechanism of Action of CNTX-0290 (cont’d) concentration (MEC) of 32 nM octreotide significantly increased glucose levels Analgesic Efficacy Diabetic Neuropathy ● Various mediators released during pathological pain states B. Mechanism of Action of CNTX-0290 ─ Efficacy was observed up to 24 hours ● Paw withdrawal threshold was determined for oral CNTX- 300 contribute to the sensitization and hyperexcitability of Figure 7. Effect of CNTX-0290 on Glucose Levels 0290 0.03 to 0.3 mg/kg vs vehicle, with lamotrigine 30 mg/kg nociceptive neurons1 Figure 2. CNTX-0290 Dose Response in the Rat CFA Model of Inflammatory Pain serving as a positive control 12 ● Stimulation of somatostatin receptor 4 (SSTR4) inhibits 200 nociception in animals, and SSTR4 knockout mice have ● Maximum efficacy 2 hours after CNTX-0290 administration 10 125 heightened responses to painful stimuli compared with wild- K+ was achieved at 0.3 mg/kg and was comparable to 8 type mice Ca2+/Na+ lamotrigine (Figure 4) 100 100 6 ● SSTR4 agonists can induce normalization of neuronal ─ MED=0.1 mg/kg, corresponding to MEC=25 nM 2 excitability, reducing inflammatory and neuropathic pain, and 75 4 are a novel target for pain therapy Figure 4. -

Fine-Tuning of GPCR Activity by Receptor-Interacting Proteins
REVIEWS Fine-tuning of GPCR activity by receptor-interacting proteins Stefanie L. Ritter and Randy A. Hall Abstract | G protein-coupled receptors (GPCRs) mediate physiological responses to various ligands, such as hormones, neurotransmitters and sensory stimuli. The signalling and trafficking properties of GPCRs are often highly malleable depending on the cellular context. Such fine-tuning of GPCR function can be attributed in many cases to receptor-interacting proteins that are differentially expressed in distinct cell types. In some cases these GPCR-interacting partners directly mediate receptor signalling, whereas in other cases they act mainly as scaffolds to modulate G protein-mediated signalling. Furthermore, GPCR-interacting proteins can have a big impact on the regulation of GPCR trafficking, localization and/or pharmacological properties. Agonist G protein-coupled receptors (GPCRs) are the largest arrestin-mediated recruitment of signalling proteins to 2 A molecule that binds to and family of transmembrane proteins in vertebrates and they activated GPCRs . Furthermore, arrestins can directly link stimulates a receptor to trigger are the molecular targets for nearly half of the therapeutic active receptors to clathrin-coated pits to facilitate receptor a cellular response. drugs that are prescribed worldwide1. The approximately endocytosis, which is an important process controlling the 5 Clathrin-coated pit 1,000 members of the GPCR family exhibit a conserved desensitization and resensitization of GPCR activity . An invaginated membrane 7-transmembrane domain topology and can be divided Interactions with G proteins, GRKs and arrestins have structure involved in receptor into 3 main subfamilies, termed A, B and C, based on been intensively studied for numerous GPCRs and endocytosis. -

Dynamic Mass Redistribution Reveals Diverging Importance of PDZ
Pharmacological Research 105 (2016) 13–21 Contents lists available at ScienceDirect Pharmacological Research j ournal homepage: www.elsevier.com/locate/yphrs Dynamic mass redistribution reveals diverging importance of PDZ-ligands for G protein-coupled receptor pharmacodynamics a b b b Nathan D. Camp , Kyung-Soon Lee , Allison Cherry , Jennifer L. Wacker-Mhyre , b b b b Timothy S. Kountz , Ji-Min Park , Dorathy-Ann Harris , Marianne Estrada , b b a b,∗ Aaron Stewart , Nephi Stella , Alejandro Wolf-Yadlin , Chris Hague a Department of Genome Sciences, University of Washington School of Medicine, Seattle, WA 98195, USA b Department of Pharmacology, University of Washington School of Medicine, Seattle, WA 98195, USA a r t i c l e i n f o a b s t r a c t Article history: G protein-coupled receptors (GPCRs) are essential membrane proteins that facilitate cell-to-cell Received 19 October 2015 communication and co-ordinate physiological processes. At least 30 human GPCRs contain a Type I PSD- Received in revised form 95/DLG/Zo-1 (PDZ) ligand in their distal C-terminal domain; this four amino acid motif of X-[S/T]-X-[] 28 December 2015 sequence facilitates interactions with PDZ domain-containing proteins. Because PDZ protein interactions Accepted 1 January 2016 have profound effects on GPCR ligand pharmacology, cellular localization, signal-transduction effector Available online 7 January 2016 coupling and duration of activity, we analyzed the importance of Type I PDZ ligands for the function of 23 full-length and PDZ-ligand truncated (PDZ) human GPCRs in cultured human cells. SNAP-epitope tag Keywords: polyacrylamide gel electrophoresis revealed most Type I PDZ GPCRs exist as both monomers and mul- G protein-coupled receptor timers; removal of the PDZ ligand played minimal role in multimer formation. -

A Histopathological Review of Six Lymphoma Subtypes
ORIGINAL RESEARCH published: 08 July 2021 doi: 10.3389/fonc.2021.710900 Somatostatin Receptors and Chemokine Receptor CXCR4 in Lymphomas: A Histopathological Review of Six Lymphoma Subtypes † † Tiina Juntikka 1* , Samuli Vaittinen 2 , Tero Vahlberg 3, Sirkku Jyrkkiö 1 and Heikki Minn 1 1 Department of Oncology and Radiotherapy, Turku University Hospital, University of Turku, Turku, Finland, 2 Department of Pathology, Turku University Hospital, University of Turku, Turku, Finland, 3 Department of Clinical Medicine, Biostatistics, University of Turku, Turku, Finland Edited by: Background: Somatostatin receptors (SSTR) and chemokine receptor CXCR4 are Thomas Ollila, Warren Alpert Medical School of expressed in lymphomas, while the abundance is known to be heterogeneous in Brown University, United States different subtypes of lymphomas. Targeting tumor cells expressing these receptors Reviewed by: might add to therapeutic opportunities while radiolabeled ligands for both imaging and Katelyn Dannheim, therapy have been developed. The aim of this study was to establish SSTR subtype 2, 3 Warren Alpert Medical School of Brown University, United States and 5 and also CXCR4 status immunohistochemically in six different lymphoma subtypes: Minggang Fang, diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), mantle cell lymphoma University of Massachusetts Medical School, United States (MCL), mucosa-associated marginal B-cell lymphoma (MALT), Hodgkin lymphoma (HL) *Correspondence: and peripheral T-cell lymphoma (PTCL). Tiina Juntikka Material and Methods: This study included a total of 103 lymphoma patients (24 DLBCL, timaru@utu.fi 22 FL, 18 HL, 9 MALT, 20 MCL and 10 PTCL) diagnosed in the Southwest hospital district †These authors have contributed equally to this work of Finland during 2010-2019.