Achieving Best Health Outcomes for Māori: a Resource
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multimorbidity, Clinical Decision Making and Health Care Delivery In
Stokes et al. BMC Family Practice (2017) 18:51 DOI 10.1186/s12875-017-0622-4 RESEARCHARTICLE Open Access Multimorbidity, clinical decision making and health care delivery in New Zealand Primary care: a qualitative study Tim Stokes1* , Emma Tumilty1, Fiona Doolan-Noble1 and Robin Gauld2 Abstract Background: Multimorbidity is a major issue for primary care. We aimed to explore primary care professionals’ accounts of managing multimorbidity and its impact on clinical decision making and regional health care delivery. Methods: Qualitative interviews with 12 General Practitioners and 4 Primary Care Nurses in New Zealand’s Otago region. Thematic analysis was conducted using the constant comparative method. Results: Primary care professionals encountered challenges in providing care to patients with multimorbidity with respect to both clinical decision making and health care delivery. Clinical decision making occurred in time-limited consultations where the challenges of complexity and inadequacy of single disease guidelines were managed through the use of “satisficing” (care deemed satisfactory and sufficient for a given patient) and sequential consultations utilising relational continuity of care. The New Zealand primary care co-payment funding model was seen as a barrier to the delivery of care as it discourages sequential consultations, a problem only partially addressed through the use of the additional capitation based funding stream of Care Plus. Fragmentation of care also occurred within general practice and across the primary/secondary care interface. Conclusions: These findings highlight specific New Zealand barriers to the delivery of primary care to patients living with multimorbidity. There is a need to develop, implement and nationally evaluate a revised version of Care Plus that takes account of these barriers. -

New Zealand's China Policy
澳大利亚-中国关系研究院 NEW ZEALAND’S CHINA POLICY Building a Comprehensive Strategic Partnership July 2015 FRONT COVER IMAGE: Chinese President Xi Jinping shakes hands with New Zealand’s Prime Minister John Key at the Great Hall of the People in Beijing, March 19 2014. © AAP Photo Published by the Australia-China Relations Institute (ACRI) Level 7, UTS Building 11 81 - 115 Broadway, Ultimo NSW 2007 t: +61 2 9514 8593 f: +61 2 9514 2189 e: [email protected] © The Australia-China Relations Institute (ACRI) 2015 ISBN 978-0-9942825-1-4 The publication is copyright. Other than for uses permitted under the Copyright Act 1968, no part may be reproduced by any process without attribution. CONTENTS List of Figures 4 List of Tables 5 Acknowledgements 5 Executive Summary 6 The Historical Context 11 Politics Above All Else 17 Early Days 17 The Pace Quickens 21 Third-country relations 29 Defence and Security 33 New Zealand’s Military Responses to China 34 To The Future 38 Economic and Trade Relations 41 A Larger Share of Global Trade 41 Free Trade Agreements 42 Merchandise Trade 48 Trade in Services 52 Investment Flows 52 Chinese Students in New Zealand 60 Tourism 62 Lessons from the New Zealand-China FTA 64 People 70 Immigration 70 Chinese Language in New Zealand 72 People-To-People 74 Conclusion 75 About The Centre 76 LIST OF FIGURES Figure 1: New Zealand-China Exports and Imports (1972-2014) 48 Figure 2: Top Six Sources of New Zealand 49 Merchandise Imports (2000-13) Figure 3: Top Six Destinations for New Zealand 50 Merchandise Exports (2000-13) Figure 4: -

Secure Dementia Care Home Design Information Resource
Secure Dementia Care Home Design Information Resource A person-centred perspective Released 2016 health.govt.nz Acknowledgements The Secure Dementia Care Home Design Information Resource was produced collaboratively by the Ministry of Health and the University of Auckland – School of Nursing. The development team of this information resource held workgroups across New Zealand that included over 150 people, representing key interest groups including aged care providers, district health board (DHB) leaders and clinicians, academics, architects, and family and friends of people with dementia. The development team would like to thank all those who attended workshops and those who provided feedback to the team. Citation: Ministry of Health. 2016. Secure Dementia Care Home Design: Information Resource. Wellington: Ministry of Health. Published in August 2016 by the Ministry of Health PO Box 5013, Wellington 6140, New Zealand ISBN: 978-0-947515-53-9 (online) HP 6468 This document is available at health.govt.nz This work is licensed under the Creative Commons Attribution 4.0 International licence. In essence, you are free to: share, ie, copy and redistribute the material in any medium or format; adapt, ie, remix, transform and build upon the material. You must give appropriate credit, provide a link to the licence and indicate if changes were made. Contents Introduction 1 Structure 1 Background 2 Types of aged residential care in New Zealand 2 Previous guidelines 2 The new resource 4 Dignity, human rights and person-centred care 5 Cultural identity -

Our Population- Canterbury Wellbeing Index
Our Population Demographics are quantifiable characteristics of a given population. Downloaded from https://www.canterburywellbeing.org.nz/our-population/ on 28/09/2021 3:37 PM These characteristics provide a picture of the current population and of changes to the population over time (including future projections). The health and wellbeing status of the population is influenced by population structure and demographic change. Changes in the size and structure of the population can also have significant impacts on the natural, physical, economic, and social environments, including the demand for health and social services, cultural and recreational services, schools, transport, water, waste management, energy, and housing. The New Zealand census is a key source of demographic information for the population. The most recent census was held on 6 March 2018 and had a lower than expected response rate, impacting the quality and coverage of some census variables. To adjust for missing information, Statistics New Zealand combined census form data and administrative data to create a census dataset with records for approximately 4.7 million people (approximately 1.4% less than the best estimate of the population on census day). Further detail about data quality is provided in the metadata for each indicator. This section presents 2018 Census data, other Statistics New Zealand population measures (such as population estimates and projections), and additional demographic data (such as deprivation and disability data) to show population structure and changes over time. Relevant local-level versus national-level comparisons are also highlighted. Key trends within demographics The greater Christchurch area has experienced unprecedented population change following the Canterbury earthquakes in September 2010 and February 2011. -

Creative Reflections of Pasifika Ethnic Mixedness
‘The Bitter Sweetness of the Space Between’: Creative Reflections of Pasifika Ethnic Mixedness By Emily Fatu A thesis submitted to the Victoria University of Wellington in fulfilment of the requirements for the degree of Master of Arts in Pacific Studies Pacific Studies, Va‘aomanū Pasifika Victoria University 2016 Abstract This Master of Arts thesis investigates and draws conclusions regarding how creative arts present accommodating spaces for articulating and understanding cultural mixedness amongst Pacific populations in New Zealand. New Zealand is home to an expanding Pacific population; statistics identify a growing number of these Pacific people who are multi-ethnic, and who are claiming their mixedness in official census data. As Pacific populations have grown, Pacific artists have risen to national prominence in visual, literary and performing arts. Many of these artists have themselves been of mixed ancestry. This thesis examines the work of three female New Zealand artists of mixed Samoan-English or Samoan- Indian descent, asking, “How do these artists and their work express their cultural mixedness?” Discussion centres on mixed media visual artist Niki Hastings-McFall, who is of English and Samoan descent; spoken word poet Grace Taylor, also of English and Samoan descent; and musical performer Aaradhna Patel, who is of Indian and Samoan descent. Placing both the creative work and public commentary of these three artists at its centre, this thesis explores how these artists publicly identify with their Samoan heritage as well as their other heritage(s); how they use their art as a platform for identity articulation; and how creative arts provide flexible and important spaces for self-expression. -

Growth and Change in Auckland
December 2013 MRQ Monitoring Research Quarterly Monitoring Research Quarterly, MRQ is produced by Auckland Council’s Research, Investigations and Monitoring Unit, RIMU. Each edition of the newsletter contains reports of RIMU’s current work including information about recent publications, research, facts and trends about Auckland. RIMU publications are available on the Auckland Council and Knowledge Auckland websites. Growth and change in Auckland Statistics New Zealand has released results a substantial increase in the number of More data will be released throughout from the 2013 New Zealand Census of Aucklanders who were in the broad Asian 2014 and available on the Statistics New Population and Dwellings held on 5 March. category. This was driven by large increases in Zealand website. In addition, the Research, They confirm that Auckland continues to residents who identify as Chinese, Indian and Investigations and Monitoring Unit is working grow and change, and that Auckland is now a Filipino. As Figure 1 shows, almost one in four closely with Statistics New Zealand to bring multi-cultural centre. Aucklanders are now Asian, an increase from the results from the 2013 census to Auckland 18.9 per cent in 2006, while the proportions Council. If you have queries about the census At the 2013 census there were 1,415,550 usual of Maori and Pacific peoples remains relatively or you are considering purchasing customised residents in Auckland, an increase of 110,592 unchanged. data, please contact RIMU first. Send your people since the 2006 census. This represents queries to [email protected] an 8.5 per cent change between 2006 and Other highlights from the 2013 census results 2013. -

Our Population- Canterbury Wellbeing Index
Our Population Demographics are quantifiable characteristics of a given population. Downloaded from https://www.canterburywellbeing.org.nz/our-population/ on 25/09/2021 6:50 PM These characteristics provide a picture of the current population and of changes to the population over time (including future projections). The health and wellbeing status of the population is influenced by population structure and demographic change. Changes in the size and structure of the population can also have significant impacts on the natural, physical, economic, and social environments, including the demand for health and social services, cultural and recreational services, schools, transport, water, waste management, energy, and housing. The New Zealand census is a key source of demographic information for the population. The most recent census was held on 6 March 2018 and had a lower than expected response rate, impacting the quality and coverage of some census variables. To adjust for missing information, Statistics New Zealand combined census form data and administrative data to create a census dataset with records for approximately 4.7 million people (approximately 1.4% less than the best estimate of the population on census day). Further detail about data quality is provided in the metadata for each indicator. This section presents 2018 Census data, other Statistics New Zealand population measures (such as population estimates and projections), and additional demographic data (such as deprivation and disability data) to show population structure and changes over time. Relevant local-level versus national-level comparisons are also highlighted. Key trends within demographics The greater Christchurch area has experienced unprecedented population change following the Canterbury earthquakes in September 2010 and February 2011. -

Making Disciples of the Post-Christian Generation: a Strategy for Auckland Bible Church Tim Collins
Fuller Theological Seminary Digital Commons @ Fuller Doctor of Ministry Projects School of Theology 9-2018 Making Disciples of the Post-Christian Generation: A Strategy for Auckland Bible Church Tim Collins Follow this and additional works at: https://digitalcommons.fuller.edu/dmin Part of the Christianity Commons Ministry Focus Paper Approval Sheet This ministry focus paper entitled MAKING DISCIPLES OF THE POST-CHRISTIAN GENERATION: A STRATEGY FOR AUCKLAND BIBLE CHURCH Written by TIM COLLINS and submitted in partial fulfillment of the requirements for the degree of Doctor of Ministry has been accepted by the Faculty of Fuller Theological Seminary upon the recommendation of the undersigned readers: _____________________________________ Tim Morey _____________________________________ Kurt Fredrickson Date Received: September 10, 2018 MAKING DISCIPLES OF THE POST-CHRISTIAN GENERATION: A STRATEGY FOR AUCKLAND BIBLE CHURCH A MINISTRY FOCUS PAPER SUBMITTED TO THE FACULTY OF THE SCHOOL OF THEOLOGY FULLER THEOLOGICAL SEMINARY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE DOCTOR OF MINISTRY BY TIM COLLINS SEPTEMBER 2018 ABSTRACT Making Disciples of the Post-Christian Generation: A Strategy for Auckland Bible Church Tim Collins Doctor of Ministry School of Theology, Fuller Theological Seminary 2018 The purpose of this doctoral project is to develop a relational approach as an apologetic for Auckland Bible Church (ABC) to reach the younger, more post- Christian generations in New Zealand and to help them grow as disciples of Jesus Christ. The current religious climate in New Zealand shows that church attendance is declining. Many young people today consider that what the church is offering is irrelevant and disconnected to their everyday existence. -
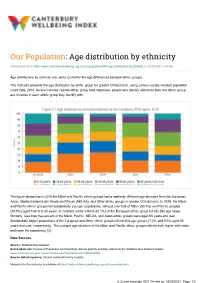
Age Distribution by Ethnicity- Canterbury Wellbeing Index
Our Population: Age distribution by ethnicity Downloaded from https://www.canterburywellbeing.org.nz/our-population/#link-age-distribution-by-ethnicity on 26/09/2021 1:36 AM Age distributions by ethnicity are useful to identify the age differences between ethnic groups. This indicator presents the age distribution by ethnic group for greater Christchurch, using census usually-resident population count data, 2018. As this indicator reports ethnic group total responses, people who identify with more than one ethnic group are included in each ethnic group they identify with. The figure shows that in 2018 the Māori and Pacific ethnic groups had a markedly different age structure from the European, Asian, Middle Eastern/Latin American/African (MELAA), and Other ethnic groups in greater Christchurch. In 2018, the Māori and Pacific ethnic groups had substantially younger populations, with just over half of Māori (50.7%) and Pacific peoples (53.6%) aged from 0 to 24 years. In contrast, under a third (31.1%) of the European ethnic group fell into this age range. Similarly, less than five percent of the Māori, Pacific, MELAA, and Asian ethnic groups were aged 65 years and over. Substantially higher proportions of the European and Other ethnic groups fell into this age group (17.2% and 9.5% aged 65 years and over, respectively). The younger age structure of the Māori and Pacific ethnic groups reflects both higher birth rates and lower life expectancy [3]. Data Sources Source: Statistics New Zealand. Survey/data set: Census of Population and Dwellings. Access publicly available data from the Statistics New Zealand website www.nzdotstat.stats.govt.nz/wbos/Index.aspx?DataSetCode=TABLECODE Source data frequency: Census conducted every 5 years. -
Asian Auckland: the Multiple Meanings of Diversity
Asian Auckland: The multiple meanings of diversity Author Wardlow Friesen February 2015 ISBN 978-0-9876637-8-8 (online PDF) © Asia New Zealand Foundation R Disclaimer: Comments made in this research report do not necessarily represent the views of the Asia New Zealand Foundation. Report Research Contents 3 About the author 5 Introduction 8 Asian migration and settlement: the national context 17 Asian migration and settlement in Auckland 28 The evolving Asian ‘ethnoscapes’ of Auckland 39 Characteristics of Asian populations of Auckland 53 Conclusion 57 Appendix Asian Auckland: The multiple meanings of diversity 2 About the author 1 About the author Dr. Friesen is currently Senior Lecturer in Geography in the School of Environment at The University of Auckland. His research focus for a number of years has been in the areas of migration and ethnic change, and research and publication have focused on various groups including Pacific, Chinese and Indian migrants. Other areas of research have included population change, international education, development in the Pacific, and urban change, with regional focuses including New Zealand, the Pacific islands and Asia; areas in which he has travelled widely. He is a regular commentator in the media on these and related issues. Between 2005 and 2007 he served as President of the Population Association of New Zealand (PANZ) and he remains active in this association. At the University of Auckland, he currently serves on the Centre for Pacific Studies Board of Graduate Studies and the Development Studies Advisory Committee. He also has considerable experience in consultancy on demographic issues and their planning implications at the national, regional and local levels. -
Māori Heterogeneity in Regional Aotearoa New Zealand: an Exploratory Study
CADDANZ Brief No. 7 December 2019 MĀORI HETEROGENEITY IN REGIONAL AOTEAROA NEW ZEALAND: AN EXPLORATORY STUDY Dr John Ryks, University of Waikato Inside this issue: Overview Overview 1 Context 1 This brief discusses work undertaken to map the heterogeneity of the Ma ori population across regional Aotearoa New Zealand. It reflects on the impacts of the Conceptualising 2 regional Māori rural-urban migration on Ma ori over time and through the use of iwi census data and spatial analysis, maps the distribution of mana whenua and ma ta waka Approach 3 populations at a regional level. The results of the research inform a discussion about the rights and interests of Ma ori in regional development at a time when Summary of 4 findings many regional settlements are either being enveloped by urban growth or are isolated and unsupported. Understanding the heterogeneity of Ma ori in regional Regional maps 7 Aotearoa New Zealand is both an under-researched topic and an often-ignored issue in policy making and local government planning, where a homogenous Ma ori Implications of the 8 research population is typically assumed. Future work 8 Context The migration of Ma ori (the indigenous peoples of Aotearoa Zealand) from rural to For further enquiries urban areas has been recognised as one of the most rapid migrations by a popula- contact; tion globally (Kukutai 2011, 2014). At the start of the 20th century, 85% of the AUTHOR Ma ori population lived in rural areas and 15% in urban areas. At the start of the 21st century this ratio had reversed with 85% living in urban areas (Statistics New Email: Zealand 2006; Kukutai 2014). -
Asian Auckland: the Multiple Meanings of Diversity
Asian Auckland: The multiple meanings of diversity Author Wardlow Friesen February 2015 ISBN 978-0-9876637-8-8 (online PDF) © Asia New Zealand Foundation R Disclaimer: Comments made in this research report do not necessarily represent the views of the Asia New Zealand Foundation. Report Research Contents 3 About the author 5 Introduction 8 Asian migration and settlement: the national context 17 Asian migration and settlement in Auckland 28 The evolving Asian ‘ethnoscapes’ of Auckland 39 Characteristics of Asian populations of Auckland 53 Conclusion 57 Appendix Asian Auckland: The multiple meanings of diversity!2 About the author 1 About the author Dr. Friesen is currently Senior Lecturer in Geography in the School of Environment at The University of Auckland. His research focus for a number of years has been in the areas of migration and ethnic change, and research and publication have focused on various groups including Pacific, Chinese and Indian migrants. Other areas of research have included population change, international education, development in the Pacific, and urban change, with regional focuses including New Zealand, the Pacific islands and Asia; areas in which he has travelled widely. He is a regular commentator in the media on these and related issues. Between 2005 and 2007 he served as President of the Population Association of New Zealand (PANZ) and he remains active in this association. At the University of Auckland, he currently serves on the Centre for Pacific Studies Board of Graduate Studies and the Development Studies Advisory Committee. He also has considerable experience in consultancy on demographic issues and their planning implications at the national, regional and local levels.