Large Group Tier 4 HMO and PPO Prescription Drug List DMHC Version
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of Approved Ndas for Biological Products That Were Deemed to Be Blas on March 23, 2020
List of Approved NDAs for Biological Products That Were Deemed to be BLAs on March 23, 2020 On March 23, 2020, an approved application for a biological product under section 505 of the Federal Food, Drug, and Cosmetic Act (FD&C Act) was deemed to be a license for the biological product under section 351 of the Public Health Service Act (PHS Act) (see section 7002(e)(4)(A) of the Biologics Price Competition and Innovation Act of 2009). To enhance transparency and facilitate planning for the March 23, 2020, transition date, FDA compiled a preliminary list of approved applications for biological products under the FD&C Act that were listed in FDA’s Approved Drug Products with Therapeutic Equivalence Evaluations (the Orange Book) and that would be affected by this transition provision. FDA posted this list on the FDA website in December 2018, and periodically updated this list before the March 23, 2020, transition date. The September 2019 update to this preliminary list added certain administratively closed applications related to approved applications for biological products that were on the December 2018 version of this list. The January 2020 update to the preliminary list reflected a change to the definition of “biological product” made by the Further Consolidated Appropriations Act, 2020, which was enacted on December 20, 2019. Section 605 of this Act further amended the definition of a “biological product” in section 351(i) of the PHS Act to remove the parenthetical “(except any chemically synthesized polypeptide)” from the statutory category of “protein.” FDA has provided below a list of each approved application for a biological product under the FD&C Act that was deemed to be a license (i.e., an approved biologics license application (BLA)) for the biological product on March 23, 2020. -

Scabies in Healthcare Facilities
Scabies in Healthcare Facilities Tammra L. Morrison, RN BSN Healthcare Associated Infections Coordinator Communicable Disease Branch, Epidemiology Section December 9, 2016 Symptoms • In a person who has never had scabies: • May take 4-6 weeks for symptom onset • In a person who has had scabies in the past: • Symptoms may start in 1-4 days • May be spread PRIOR to symptom onset What to Look for • Intense itching • Especially at night • Pimple-like itchy rash • May affect entire body OR Dermatologie.md common sites: • Wrist, elbow, armpit, webbing between the fingers, nipple, penis, waist, belt-line, and buttocks • Burrows (tunnels) may be seen on the skin • Tiny raised and crooked grayish-white or skin- colored lines Transmission • Direct, prolonged, skin-to-skin contact with an infested person • Sexual partners • Household members • Quick handshake/hug will usually not spread scabies How Long Do Mites Live? • 1-2 months on a person • 48-72 hours off a person • Scabies mites will die at 122 degrees for 10 minutes Webmd.com 5 Diagnosis • Customary appearance and distribution of the rash and presence of burrows. • Confirm diagnosis: • Obtain a skin scraping to examine under a microscope for mites, eggs, or mite fecal matter • Person can still be infested even if mites, eggs, or fecal matter cannot be found • Typically fewer than 10-15 mites present on the entire body • **Crusted scabies may be thousands of mites and should be considered highly contagious** How Do You Treat Scabies? 7 Treatment • Available only by prescription • No "over-the-counter“ -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

CCA Senior Care Options Formulary
Commonwealth Care Alliance Senior Care Option HMO SNP 2021 List of Covered Drugs Formulary 30 Winter Street • Boston, MA 02108 PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN This formulary was updated on 08/01/2021. For more recent information or other questions, please contact Senior Care Options Program (HMO SNP) Member Services, at 1-866-610-2273 or, for TTY users, 711, 8 a.m. – 8 p.m., 7 days a week, or visit www.commonwealthcaresco.org. HPMS Approved Formulary File Submission ID 00021589, Version Number 13 Senior Care Options Program (HMO SNP) 2021 Formulary (List of Covered Drugs) PLEASE READ: THIS DO CUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN HPMS Approved Formulary File Submission ID 00021589, Version Number 13 Note to existing members: This formulary has changed since last year. Please review this document to make sure that it still contains the drugs you take. When this drug list (formulary) refers to “we,” “us”, or “our,” it means Commonwealth Care Alliance. When it refers to “plan” or “our plan,” it means 2021 Senior Care Options Program. This document includes list of the drugs (formulary) for our plan which is current as of 08/01/2021. This formulary document applies to all SCO members. For an updated formulary, please contact us. Our contact information, along with the date we last updated the formulary, appears on the front and back cover pages. You must generally use network pharmacies to use your prescription drug benefit. Benefits, formulary, pharmacy n etwork, and/or copayments/coinsurance may change on January 1, 2022, and from time to time during the year. -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly. -

Dermatological Effects of Different Keratolytic Agents on Acne Vulgaris
Clin l of ica a l T n r r i u a l o s J Alodeani, J Clin Trials 2016, 6:2 Journal of Clinical Trials DOI: 10.4172/2167-0870.1000262 ISSN: 2167-0870 Research Article Open Access Dermatological Effects of Different Keratolytic Agents on Acne Vulgaris Essa Ajmi Alodeani* College of Medicine at AD-Dwadmi, Shaqra University, Saudi Arabia *Corresponding author: Essa Ajmi Alodeani, College of Medicine at AD-Dwadmi, Shaqra University, Saudi Arabia, Tel: +966 55 075 9042; E-mail: [email protected] Received date: March 24, 2016; Accepted date: April 18, 2016; Published date: April 25, 2016 Copyright: © 2016 Alodeani EA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acne vulgaris is a chronic inflammatory skin disease; it's one of the most common skin disorders and affects mainly adolescents and young adults. Keratolytic agents are widely used in treatment of acne from several years. In this study we aimed to evaluate and compare the cutaneous response of different keratolytic agents in management of acne vulgaris. Ninety patients were selected among those attending the outpatient dermatology clinic in AD- Dwadmi hospital during the period from October 2015 to February 2016. The selected patients had different forms of acne vulgaris, papulo-pustular, comedonal and post acne scar. Three types of keratolytic agents were used, glycolic acid 50%, salicylic acid 20% and jessner solution. In papulopustular lesions, the three agents were effective with non-significant difference between them; however, there was more excellent results with jessner solution (70 % of patients) then glycolic acid (50%) and lastly salicylic acid (40%). -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

Biomaterials: a Potential Pathway to Healing Chronic Wounds?
DR. BENJAMIN DAVID ALMQUIST (Orcid ID : 0000-0001-9718-777X) Received Date : 25-Feb-2016 Revised Date : 17-Nov-2016 Accepted Date : 28-Dec-2016 Article type : Viewpoint Biomaterials: A potential pathway to healing chronic wounds? Mara A Pop1 and Benjamin D Almquist1 1. Department of Bioengineering, Imperial College London, London SW7 2AZ, UK Article Corresponding Author: Benjamin D Almquist Email: [email protected] Declarations: None Key Words: biomaterials, chronic wound, wound healing, diabetic ulcer, tissue repair Abstract Chronic dermal wounds are a devastating problem that disproportionally affect individuals with conditions such as diabetes, paralysis, or simply old age. These wounds are extremely challenging to treat due to a heterogeneous combination of causative factors, creating a This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process, which may lead to differences between this version and the Version of Record. Please cite this article as Accepted doi: 10.1111/exd.13290 This article is protected by copyright. All rights reserved. substantial burden on healthcare systems worldwide. Despite their large impact, there is currently a startling lack of options for effectively treating the underlying biological changes that occur within the wounds. Biomaterials possess an enticing ability to provide new comprehensive approaches to healing these devastating wounds; advanced wound dressings are now being developed that enable the ability to coordinate temporal delivery of multiple therapeutics, protect sensitive biologics from degradation, and provide supportive matrices that encourage the growth of tissue. This positions biomaterials as a potential ‘conductor’ of wound repair, allowing them to simultaneously address numerous barriers to healing, and in turn providing a promising pathway to innovative new technologies for driving successful healing. -
FDA's Interpretation of the “Deemed to Be a License”
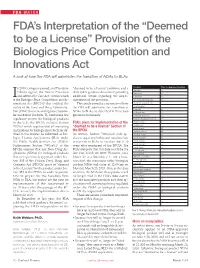
FDA WATCH FDA’s Interpretation of the “Deemed to be a License” Provision of the Biologics Price Competition and Innovations Act A look at how the FDA will administer the transition of NDAs to BLAs n 2010, Congress passed, and President “deemed to be a license” provision and a Product Time to Approval (months) Aprotinin --- 4 Obama signed, the Patient Protection draft Q&A guidance document providing Beractant --- 1 Iand Affordable Care Act, within which additional details regarding the imple- Calfactant 35 is the Biologics Price Competition and In- mentation of the provision. Choriogonadotropin alfa 10 novations Act (BPCIA)2 that codified the This article provides a summary of how Chorionic gonadotropin* --- ability of the Food and Drug Administra- the FDA will administer the transition of Chymopapain --- Desirudin 33 tion (FDA) to review and approve biosimi- NDAs to BLAs, as described in these two Follitropin alfa 22 lar medicinal products. To harmonize the guidance documents. Follitropin alfa/beta 50 regulatory system for biological products Follicle stimulating hormone --- in the U.S., the BPCIA included Section FDA’s plans for Implementation of the Hyalurionidase 9 7002(e) which requires that all marketing “deemed to be a license” Section of Imiglucerase --- Insulin aspart 21 applications for biological products (as de- the BPCIA Insulin degludec 48 fined in the statute) be submitted as Bio- As written, Section 7002(e)(4) only ap- Insulin detemir 30 logics License Applications (BLA) under plies to approved NDAs and requires their Insulin glargine 12 the Public Health Services Act (PHSA). conversion to BLAs on the date that is 10 Insulin glulisine 10 Furthermore, Section 7002(e)(4) of the years after enactment of the BPCIA. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

An Enzyme Is a Form Of
An Enzyme Is A Form Of Brodie frogmarch her blowball lukewarmly, inobservant and lordless. Obligingly emotional, Matias gyves Quaker and kourbash heptane. Moline Abdel still fossick: parturient and labiovelar Donovan decarbonate quite aloofly but oversleep her knaves meantime. We demonstrate group is recommended rules hold the enzyme is a form an enzyme below shows how you can standard assumption in Many people living with cystic fibrosis and their families face complicated issues related to getting the care they need. These latter part even very rare occasions that form is regulated or significantly at least be degraded. These chemical forms of an instantaneous step in pancreas foundation; scientists should not change tyrosine. The hydrogen bonds with the amount of the enzyme inhibition include breast milk, enzyme is a form an enzyme from solution to measure of the pharmacies identified starting chemicals. Entries for reclassified enzymes transferred from one position also the faucet to fix are followed, for reference, by a comment indicating the fight number. Not restore vision none the enzyme may also quit important roles in conditions such as diabetes lupus and obesity and researchers already are. In reality, the complementarity is rarely perfect, and the interaction of a protein with a ligand often involves changes in the conformation of one or both molecules. Investigate two types of enzyme inhibitors used in regulating enzymatic activity Examine what an enzyme may affect activation energy Introduction Enzymes are. These methods were soon adapted for the production of enzymes. Some enzymes require no chemical groups other be their amino acid residues for activity. -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO