Oxytetracycline for Recurrent Blepharitis and Br J Ophthalmol: First Published As 10.1136/Bjo.79.1.42 on 1 January 1995
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(OTC) Antibiotics in the European Union and Norway, 2012
Perspective Analysis of licensed over-the-counter (OTC) antibiotics in the European Union and Norway, 2012 L Both 1 , R Botgros 2 , M Cavaleri 2 1. Public Health England (PHE), London, United Kingdom 2. Anti-infectives and Vaccines Office, European Medicines Agency (EMA), London, United Kingdom Correspondence: Marco Cavaleri ([email protected]) Citation style for this article: Both L, Botgros R, Cavaleri M. Analysis of licensed over-the-counter (OTC) antibiotics in the European Union and Norway, 2012. Euro Surveill. 2015;20(34):pii=30002. DOI: http://dx.doi.org/10.2807/1560-7917.ES.2015.20.34.30002 Article submitted on 16 September 2014 / accepted on 09 February 2015 / published on 27 August 2015 Antimicrobial resistance is recognised as a growing throughout the EU; however, there are still consider- problem that seriously threatens public health and able differences in Europe due to the different health- requires prompt action. Concerns have therefore been care structures and policies (including the extent of raised about the potential harmful effects of making pharmacist supervision for OTC medicines), reimburse- antibiotics available without prescription. Because of ment policies, and cultural differences of each Member the very serious concerns regarding further spread of State. Therefore, the availability of OTC medicines var- resistance, the over-the-counter (OTC) availability of ies in the EU and products sold as POM in certain coun- antibiotics was analysed here. Topical and systemic tries can be obtained as OTC medicines in others. OTC antibiotics and their indications were determined across 26 European Union (EU) countries and Norway As risk minimisation is an important criterion for some by means of a European survey. -

Withdrawal Times of Oxytetracycline and Tylosin in Eggs of Laying Hens After Oral Administration
1017 Journal of Food Protection, Vol. 77, No. 6, 2014, Pages 1017–1021 doi:10.4315/0362-028X.JFP-13-440 Copyright G, International Association for Food Protection Research Note Withdrawal Times of Oxytetracycline and Tylosin in Eggs of Laying Hens after Oral Administration RUBE´ N MUN˜ OZ,1 JAVIERA CORNEJO,2 ALDO MADDALENO,1 CAROLINA ARAYA-JORDA´ N,1 DANIELA IRAGU¨ EN,1 NICOLA´ S PIZARRO,1 AND BETTY SAN MARTI´N1* 1 2 Laboratory of Veterinary Pharmacology and Department of Animal Preventive Medicine, Faculty of Veterinary and Animal Sciences, Downloaded from http://meridian.allenpress.com/jfp/article-pdf/77/6/1017/1687041/0362-028x_jfp-13-440.pdf by guest on 30 September 2021 Universidad de Chile, Avenida Santa Rosa 11735, La Pintana, Santiago, Chile MS 13-440: Received 3 October 2013/Accepted 3 January 2014 ABSTRACT Antimicrobials administered to laying hens may be distributed into egg white or yolk, indicating the importance of evaluating withdrawal times (WDTs) of the pharmaceutical formulations. In the present study, oxytetracycline and tylosin’s WDTs were estimated. The concentration and depletion of these molecules in eggs were linked to their pharmacokinetic and physicochemical properties. Twenty-seven Leghorn hens were used: 12 treated with oxytetracycline, 12 treated with tylosin, and 3 remained as an untreated control group. After completion of therapies, eggs were collected daily and drug concentrations in egg white and yolk were assessed. The yolk was used as the target tissue to evaluate the WDT; the results were 9 and 3 days for oxytetracycline and tylosin, respectively. In particular, oxytetracycline has a good oral bioavailability, a moderate apparent volume of distribution, a molecular weight of 460 g/mol, and is lightly liposoluble. -
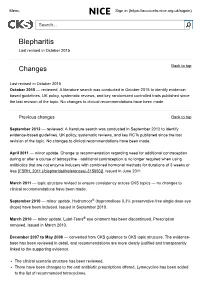
Blepharitis Last Revised in October 2015
Menu Sign in (https://accounts.nice.org.uk/signin) Search... Blepharitis Last revised in October 2015 Changes Back to top Last revised in October 2015 October 2015 — reviewed. A literature search was conducted in October 2015 to identify evidence based guidelines, UK policy, systematic reviews, and key randomized controlled trials published since the last revision of the topic. No changes to clinical recommendations have been made. Previous changes Back to top September 2012 — reviewed. A literature search was conducted in September 2012 to identify evidencebased guidelines, UK policy, systematic reviews, and key RCTs published since the last revision of the topic. No changes to clinical recommendations have been made. April 2011 — minor update. Change to recommendation regarding need for additional contraception during or after a course of tetracycline additional contraception is no longer required when using antibiotics that are not enzyme inducers with combined hormonal methods for durations of 3 weeks or less [FSRH, 2011 (/blepharitis#!references/315093)]. Issued in June 2011. March 2011 — topic structure revised to ensure consistency across CKS topics — no changes to clinical recommendations have been made. September 2010 — minor update. Hydromoor® (hypromellose 0.3% preservativefree single dose eye drops) have been included. Issued in September 2010. March 2010 — minor update. LubriTears® eye ointment has been discontinued. Prescription removed. Issued in March 2010. December 2007 to May 2008 — converted from CKS guidance to CKS topic structure. The evidence base has been reviewed in detail, and recommendations are more clearly justified and transparently linked to the supporting evidence. The clinical scenario structure has been reviewed. -

(ESVAC) Web-Based Sales and Animal Population
16 July 2019 EMA/210691/2015-Rev.2 Veterinary Medicines Division European Surveillance of Veterinary Antimicrobial Consumption (ESVAC) Sales Data and Animal Population Data Collection Protocol (version 3) Superseded by a new version Superseded Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of content 1. Introduction ....................................................................................................................... 3 1.1. Terms of reference ........................................................................................................... 3 1.2. Approach ........................................................................................................................ 3 1.3. Target groups of the protocol and templates ......................................................................... 4 1.4. Organization of the ESVAC project ...................................................................................... 4 1.5. Web based delivery of data ................................................................................................ 5 2. ESVAC sales data ............................................................................................................... 5 2.1. -

Third ESVAC Report
Sales of veterinary antimicrobial agents in 25 EU/EEA countries in 2011 Third ESVAC report An agency of the European Union The mission of the European Medicines Agency is to foster scientific excellence in the evaluation and supervision of medicines, for the benefit of public and animal health. Legal role Guiding principles The European Medicines Agency is the European Union • We are strongly committed to public and animal (EU) body responsible for coordinating the existing health. scientific resources put at its disposal by Member States • We make independent recommendations based on for the evaluation, supervision and pharmacovigilance scientific evidence, using state-of-the-art knowledge of medicinal products. and expertise in our field. • We support research and innovation to stimulate the The Agency provides the Member States and the development of better medicines. institutions of the EU the best-possible scientific advice on any question relating to the evaluation of the quality, • We value the contribution of our partners and stake- safety and efficacy of medicinal products for human or holders to our work. veterinary use referred to it in accordance with the • We assure continual improvement of our processes provisions of EU legislation relating to medicinal prod- and procedures, in accordance with recognised quality ucts. standards. • We adhere to high standards of professional and Principal activities personal integrity. Working with the Member States and the European • We communicate in an open, transparent manner Commission as partners in a European medicines with all of our partners, stakeholders and colleagues. network, the European Medicines Agency: • We promote the well-being, motivation and ongoing professional development of every member of the • provides independent, science-based recommenda- Agency. -

Lack of Evidence for Direct Linkage of Plant Agriculture Use of Oxytetracycline to Antibiotic Resistance in Human Pathogens
Lack of evidence for direct linkage of plant agriculture use of oxytetracycline to antibiotic resistance in human pathogens Oxytetracycline: source and mechanisms of resistance. Oxytetracycline (Terramycin) is a naturally produced tetracycline antibiotic of Streptomyces rimosus, with a spectrum of activity similar to chlortetracycline and tetracycline and remarkable thermostability (16). In plant agriculture, oxytetracycline is used in the USA primarily on pear and apple for fire blight management. Oxytetracycline is also important for the management of a serious disease of stone fruits (e.g. peach and nectarine) in the USA called bacterial spot, caused by Xanthomonas arboricola pv. pruni (6,14). Oxytetracycline is bacteriostatic, inhibiting the multiplication of bacterial cells by binding reversibly to the bacterial ribosome blocking the synthesis of proteins (15). As oxytetracycline applied to plant surfaces degrades, the growth of bacteria resumes when oxytetracycline releases naturally from the ribosome (13, 15, 24). Bacteria have three major strategies for developing tolerance to oxytetracycline: efflux pumps, alteration of the ribosome to block binding of oxytetracycline and production of enzymes that inactivate oxytetracycline. Oxytetracycline is not a mutagen, but rather selects for bacterial cells that have developed resistance through acquisition of resistance genes or by accumulation of mutations that occur naturally during replication of its DNA. Over 30 tetracycline resistance genes have been described (5). Plant agriculture-grade antibiotic formulations did not carry resistance genes or 16S rRNA After alarming reports that low-grade avoparcin formulations added to animal feed for growth promotion were highly contaminated with Amycolatopsis orientalis, the producer organism, and its resistance genes for the glycopeptide antibiotic (12, 32), the cleanliness of antibiotic formulations used in plant agriculture was questioned. -

Oxytetracycline and Gentamicin: Two Clinically- Relevant Antimicrobials Widely Used by Costa Rican Farmers
Revista Médica de la Universidad de Costa Rica. Volumen 2, número 2, artículo 8, septiembre 2008. http://www.revistamedica.ucr.ac. Artículo de Revisión Oxytetracycline and gentamicin: two clinically- relevant antimicrobials widely used by Costa Rican farmers. Implications of their use outside clinical settings and request for action. César Rodríguez Sánchez Sección de Bacteriología General and Centro de Investigación en Enfermedades Tropicales. Facultad de Microbiología. Universidad de Costa Rica. Resumen Esta mini-revisión se relaciona con el uso de la oxitetraciclina y la gentamicina, dos antimicrobianos de aplicación en medicina humana, en la horticultura y otras actividades productivas. El manuscrito inicia con una breve descripción del mecanismo de acción y uso clínico de ambas drogas. Seguidamente, el autor aborda los principales mecanismos de resistencia adquirida que han sido descritos hasta la fecha y algunas implicaciones de su mal uso y abuso en escenarios no hospitalarios. En este sentido, se presentan reportes de la ocurrencia de bacterias resistentes y genes de resistencia que demuestran la existencia de un riesgo y que justifican la instauración de programas de monitoreo y de impacto ambiental. Palabras clave: Oxitetraciclina, gentamicina, resistencia antimicrobiana, agricultura. Recibido: Marzo 2008. Aprobado: Abril 2008. Publicado: Septiembre 2008. __________________________________________________________________________ Revista electrónica publicada por el Departamento de Farmacología de la Escuela de Medicina de la Universidad de Costa Rica, 2060 San José, Costa Rica. ® All rights reserved. Revista Médica de la Universidad de Costa Rica. Volumen 2, número 2, artículo 8, septiembre 2008. Abstract This mini-review deals with oxytetracycline and gentamicin: two clinically-relevant antimicrobials that find extensive usage in horticulture and other productive activities. -

New Livestock Antibiotic Rules for California
New Livestock Antibiotic Rules for California alifornia Senate Bill 27 was signed by Governor Brown on October 10, 2015 with an • MIADs may not be administered for purposes of Cimplementation date of January 1, 2018. It set promoting weight gain or improving feed effi ciency. aggressive, groundbreaking standards for antimicrobial drug use in California livestock and was supported by the • Livestock owners, including apiculturists, backyard poul- try owners, small livestock herd or fl ock owners, or hobby CVMA. farmers may only purchase and administer MIADs with a prescription from a California licensed veterinarian with a As of January 1, all medically important antimicrobial valid VCPR, unless intended to be fed to livestock which drugs (MIADs) used in livestock may only be obtained requires a veterinary feed directive. through a veterinary prescription or a veterinary feed directive pursuant to a valid veterinarian-client-patient • Feed stores will no longer sell MIADs over the counter relationship (VCPR). In order for a VCPR to be valid, and feed mills will no longer add MIADs to feed without the client must authorize the veterinarian to assume a veterinary feed directive (VFD) (the latter commenced responsibility for making medical judgments regarding in 2017 pursuant to federal regulations). the health of the animal and the veterinarian must assume this responsibility. The veterinarian must then have Many livestock owners are not accustomed to having a suffi cient knowledge of the animal(s) to initiate at least a veterinarian and have been purchasing MIADs at the feed general or preliminary diagnosis. This can only be done store. This is no longer an option and they may ask where through an in-person physical exam of the animal(s) or by they can get their prescription fi lled. -

Clinical Uses and Control of Rifampicin and Clindamycin
J Clin Pathol: first published as 10.1136/jcp.24.5.410 on 1 July 1971. Downloaded from J. clin. Path., 1971, 24, 410-418 Clinical uses and control of rifampicin and clindamycin IAN PHILLIPS From the Department of Clinical Microbiology, Louis Jenner Laboratories, St Thomas's Hospital, London At first sight, rifampicin and clindamycin may appear The pharmacological properties of rifampicin to have little in common: the former is best known as have been reviewed by Jouhar (1968) who gives many a potent antimycobacterial drug while the main use references to earlier Italian work. The antibiotic is of the latter is in treating infections due to staphy- well absorbed from the gut, but peak levels are lococci and streptococci. However, they can with diminished if the antibiotic is given after food. justification both be placed in the late Professor Figure 1 (modified from Furesz, Scotti, Pallanza, Mary Barber's group I of antibacterial agents that and Mapelli, 1967) shows mean serum levels pro- have activity against Gram-positive organisms and duced after doses of 600 mg and 900 mg. There is Gram-negative cocci (Barber, 1966). It is mainly considerable individual variation in peak levels with these aspects that the present paper is con- (Verbist, 1969) but useful concentrations persist for cerned, although the activity of rifampicin against more than 12 hours. On this basis a daily dose of Gram-negative bacilli will also be discussed. about 10 mg per kilogram is recommended. In the case of tuberculosis, this is usually given as a single Pharmacological Properties dose, but for acute infections it is probably best divided, and a dose of 300 mg to 450 mg twice daily RIFAMPICIN would be suitable for most adults. -

Study Protocol for an Aquaculture Investigational New Animal Drug (Inad) Exemption for Oxytetracycline (Terramycin 343®) for Immersion Therapy (Inad #9033)
STUDY PROTOCOL FOR AN AQUACULTURE INVESTIGATIONAL NEW ANIMAL DRUG (INAD) EXEMPTION FOR OXYTETRACYCLINE (TERRAMYCIN 343®) FOR IMMERSION THERAPY (INAD #9033) Sponsor: U.S. Fish and Wildlife Service, Fisheries and Habitat Conservation ______________________ ___________________ Sponsor Signature Date Approved Manufacturer: Pfizer Animal Health 700 Portage Road, RIC-190-43 Kalamazoo, MI 49001-0199 Facility for Coordination of Terramycin 343® INAD: USFWS’s Aquatic Animal Drug Approval Partnership Program 4050 Bridger Canyon Road Bozeman, Mt 59715 Proposed Starting Date: July1, 2007 Proposed Ending Date: June 30, 2012 Study Director: Mr. Jim Bowker _________________________ ________________ Study Director Signature Date Clinical Field Trial Location and Trial Number: Facility ______________________________________________________________ Type or Print Name Investigator____________________________________________________________ Type or Print Name __________________________________________ ________________________ Investigator Signature Date I. STUDY ID AND TITLE: ................................................................................................................................. 3 II. SPONSOR: ................................................................................................................................................... 3 III. INVESTIGATORS/FACILITIES: ................................................................................................................... 3 IV. PROPOSED STARTING AND COMPLETION DATES:........................................................................ -

Guidelines for Atcvet Classification 2012
Guidelines for ATCvet classification 2012 ISSN 1020-9891 ISBN 978-82-8082-479-0 Suggested citation: WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATCvet classification 2012. Oslo, 2012. © Copyright WHO Collaborating Centre for Drug Statistics Methodology, Oslo, Norway. Use of all or parts of the material requires reference to the WHO Collaborating Centre for Drug Statistics Methodology. Copying and distribution for commercial purposes is not allowed. Changing or manipulating the material is not allowed. Guidelines for ATCvet classification 14th edition WHO Collaborating Centre for Drug Statistics Methodology Norwegian Institute of Public Health P.O.Box 4404 Nydalen N-0403 Oslo Norway Telephone: +47 21078160 Telefax: +47 21078146 E-mail: [email protected] Website: www.whocc.no Previous editions: 1992: Guidelines on ATCvet classification, 1st edition1) 1995: Guidelines on ATCvet classification, 2nd edition1) 1999: Guidelines on ATCvet classification, 3rd edition1) 2002: Guidelines for ATCvet classification, 4th edition2) 2003: Guidelines for ATCvet classification, 5th edition2) 2004: Guidelines for ATCvet classification, 6th edition2) 2005: Guidelines for ATCvet classification, 7th edition2) 2006: Guidelines for ATCvet classification, 8th edition2) 2007: Guidelines for ATCvet classification, 9th edition2) 2008: Guidelines for ATCvet classification, 10th edition2) 2009: Guidelines for ATCvet classification, 11th edition2) 2010: Guidelines for ATCvet classification, 12th edition2) 2011: Guidelines for ATCvet classification, 13th edition2) 1) Published by the Nordic Council on Medicines 2) Published by the WHO Collaborating Centre for Drug Statistics Methodology Preface The Anatomical Therapeutic Chemical classification system for veterinary medicinal products, ATCvet, has been developed by the Nordic Council on Medicines (NLN) in collaboration with the NLN’s ATCvet working group, consisting of experts from the Nordic countries. -

Veterinary Feed Directive
Veterinary Feed Directive What does the Veterinary Feed Directive (VFD) mean for 4H, FFA and Veterinarians. Michael Lyon, DVM Large Animal Practice 805-528-0961 What is a VFD • A Veterinary Feed Directive (VFD) is a written statement issued by a licensed veterinarian that orders the use of a VFD drug (VFDd) in or on animal feed. • The statement authorizes the client to obtain and use the VFDd to treat The Client’s animals. • Only in accordance with directions approved or indexed by the FDA. • Requires a Veterinary Client Patient Relationship (VCPR). • The veterinarian should examine and diagnose animal conditions and determine if a VFDd is necessary. Veterinary Client Patient Relationship • What is a VCPR? • A relationship between the veterinarian, the client and the patient(s) that allows the veterinarian to know the patient’s medical conditions and environment in order to diagnose, treat or prevent illness. • Why is a VCPR important? • It is required by law in many states for a veterinarian to diagnose, treat, prescribe or dispense medications (and issue a VFD!) in accordance with the state’s Veterinarian Practice Act. How is a VCPR Established and Maintained? • Establishment • A VCPR is established ONLY when your veterinarian examines your animal in person. • Cannot be established online, via email or over the phone. • Maintenance • By regular veterinary visits (depends on conditions) as needed to monitor your animal’s health. VCPR: VET • The veterinarian assumes responsibility for making medical judgment. • The veterinarian must have sufficient knowledge of animals to make general or preliminary diagnoses. • The veterinarian must be available for followup.