Giant Sialocele Following Facial Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diseases of Salivary Glands: Review
ISSN: 1812–1217 Diseases of Salivary Glands: Review Alhan D Al-Moula Department of Dental Basic Science BDS, MSc (Assist Lect) College of Dentistry, University of Mosul اخلﻻضة امخجوًف امفموي تُئة رطبة، حتخوي ػىل طبلة ركِلة من امسائل ثدغى انوؼاب ثغطي امسطوح ادلاخوَة و متﻷ امفراغات تني ااطَة امفموًة و اﻷس نان. انوؼاب سائل مؼلد، ًنذج من امغدد انوؼاتَة، اذلي ًوؼة دورا" ىاما" يف اﶈافظة ػىل سﻻمة امفم. املرىض اذلٍن ؼًاهون من هلص يف اﻷفراز انوؼايب حكون دلهيم مشبلك يف اﻷلك، امخحدث، و امبوع و ًطبحون غرضة مﻷههتاابت يف اﻷغش َة ااطَة و امنخر املندرش يف اﻷس نان. ًوخد ثﻻثة أزواج من امغدد انوؼاتَة ام ئرُسة – امغدة امنكفِة، امغدة حتت امفكِة، و حتت انوساهَة، موضؼيا ٍكون خارج امخجوًف امفموي، يف حمفظة و ميخد هظاهما املنَوي مَفرغ افرازاهتا. وًوخد أًضا" امؼدًد من امغدد انوؼاتَة امطغرية ، انوساهَة، اتحنكِة، ادلىوزيًة، انوساهَة احلنكِة وما كبل امرخوًة، ٍكون موضؼيا مﻷسفل و مضن امغشاء ااطي، غري حماطة مبحفظة مع هجاز كنَوي كطري. افرازات امغدد انوؼاتَة ام ئرُسة مُست مدشاهبة. امغدة امفكِة ثفرز مؼاب مطيل غين ابﻷمِﻻز، وامغدة حتت امفكِة ثنذج مؼاب غين اباط، أما امغدة حتت انوساهَة ثنذج مؼااب" مزخا". ثبؼا" ميذه اﻷخذﻻفات، انوؼاب املوحود يق امفم ٌشار امَو مكزجي. ح كرَة املزجي انوؼايب مُس ثس َطا" واملادة اﻷضافِة اموػة من لك املفرزات انوؼاتَة، اكمؼدًد من امربوثُنات ثنذلل ثرسػة وثوخطق هبدروكس َل اﻷتُذاًت مﻷس نان و سطوح ااطَة امفموًة. ثبدأ أمراض امغدد انوؼاتَة ػادة تخغريات اندرة يف املفرزات و ام كرتَة، وىذه امخغريات ثؤثر اثهواي" من خﻻل جشلك انووحية اجلرثومِة و املوح، اميت تدورىا ثؤدي اىل خنور مذفش َة وأمراض وس َج دامعة. ىذه اﻷمراض ميكن أن ثطبح شدًدة تؼد املؼاجلة امشؼاغَة ﻷن امؼدًد من احلاﻻت اجليازًة )مثل امسكري، امخوَف اهكُيس( ثؤثر يف اجلراين انوؼايب، و ٌش خيك املرض من حفاف يف امفم. -

ISSN: 2320-5407 Int. J. Adv. Res. 7(10), 979-1021
ISSN: 2320-5407 Int. J. Adv. Res. 7(10), 979-1021 Journal Homepage: - www.journalijar.com Article DOI: 10.21474/IJAR01/9916 DOI URL: http://dx.doi.org/10.21474/IJAR01/9916 RESEARCH ARTICLE MINOR ORAL SURGICAL PROCEDURES. Harsha S K., Rani Somani and Shipra Jaidka. 1. Postgraduate Student, Department of Pediatric and Preventive Dentistry, Divya Jyoti college of Dental Sciences & Research, Modinagar, UP, India. 2. Professor and Head of the Department, Department of Pediatric and Preventive Dentistry, Divya Jyoti College of Dental Sciences & Research, Modinagar, UP, India. 3. Professor, Department of Pediatric and Preventive Dentistry, Divya Jyoti College of Dental Sciences & Research, Modinagar, UP, India. ……………………………………………………………………………………………………………………….... Manuscript Info Abstract ……………………. ……………………………………………………………… Manuscript History Minor oral surgery includes removal of retained or burried roots, Received: 16 August 2019 broken teeth, wisdom teeth and cysts of the upper and lower jaw. It also Final Accepted: 18 September 2019 includes apical surgery and removal of small soft tissue lesions like Published: October 2019 mucocele, ranula, high labial or lingual frenum etc in the mouth. These procedures are carried out under local anesthesia with or without iv Key words:- Gamba grass, accessions, yield, crude sedation and have relatively short recovery period. protein, mineral contents, Benin. Copy Right, IJAR, 2019,. All rights reserved. …………………………………………………………………………………………………….... Introduction:- Children are life‟s greatest gifts. The joy, curiosity and energy all wrapped up in tiny humans. This curiosity and lesser motor coordination usually leads to increased incidence of falls in children which leads to traumatic dental injuries. Trauma to the oral region may damage teeth, lips, cheeks, tongue, and temporomandibular joints. These traumatic injuries are the second most important issue in dentistry, after the tooth decay. -
Parotid and Mandibular Salivary Glands Segmentation of the One Humped Dromedary Camel (Camelus Dromedarius)
Int. J. Adv. Res. Biol. Sci. (2017). 4(11): 32-41 International Journal of Advanced Research in Biological Sciences ISSN: 2348-8069 www.ijarbs.com DOI: 10.22192/ijarbs Coden: IJARQG(USA) Volume 4, Issue 11 - 2017 Research Article DOI: http://dx.doi.org/10.22192/ijarbs.2017.04.11.005 Parotid and Mandibular Salivary Glands Segmentation Of The One Humped Dromedary Camel (Camelus dromedarius) Hamdy M. Rezk and Nora A. Shaker* Department of Anatomy and Embryology, Faculty of Veterinary Medicine, Cairo University, Egypt *Corresponding author: [email protected] Abstract The present study provides detailed anatomical description of the parotid and mandibular salivary glands of the one humped camel with their segmentation based on arterial blood supply and salivary ducts; to facilitate partial removal of the pathologic gland. The shape, position, relations and blood supply of both salivary glands with their ducts were studied on six cadaveric heads. The mandibular and parotid ducts were injected with Urographin® as contrast medium; through inserting the catheter into their openings in the oral cavity; then applying lateral radiography immediately after the injection. The common carotid arteries were injected with red Latex Neoprene and dissected. The parotid gland was irregular rectangular and had five processes while the mandibular gland was irregular triangular with rounded proximal and pointed distal extremity. The parotid duct enters the oral cavity on the cheek opposite the upper 4th molar tooth. The mandibular duct opens in the oral cavity at the sublingual caruncles on the sublingual floor, just about 2cm cranial to frenulum linguae. Both The parotid and the mandibular salivary glands could be divided into four segments. -
Variations of Parotidectomy – Indications and Technique
Variations of Parotidectomy – Indications and Technique Kerry D. Olsen, M.D. Professor and Chair Head and Neck Surgery Mayo Clinic Parotidectomy Personal experience > 32 years • 60 – 100 cases per year • Variety of neoplasms and anatomic variations • Minimal morbidity overall • Recurrent neoplasms – challenging cases 1 Parotid Surgery - Challenges Patient expectations Variety of tumors encountered Relationship and size of the tumor to the nerve Extend the operation as needed Role of pathology Parotidectomy Surgical options: • Superficial parotidectomy • Partial parotidectomy • Deep lobe parotidectomy • Total parotidectomy • Extended parotidectomy 4 2 Surgical Technique Superficial parotidectomy Deep lobe parotidectomy Surgeons will spend their entire career trying to learn when it is safe or necessary to do more or less than a superficial parotidectomy 5 Superficial Parotidectomy Indications • Neoplasm • Risk of metastasis • Recurrent infection/abscess • Surgical exposure – deep lobe/ parapharynx/ infratemporal fossa • Cosmesis 6 3 Pre-operative Discussion Individualized • Goals – rational – risks Goals – safe and complete removal with surrounding margin of normal tissue and preservation of facial nerve function 7 8 4 9 10 5 11 12 6 13 14 7 Facial Nerve Identification Helpful: • Cartilaginous pointer • Posterior belly of the digastric muscle • Mastoid tip Retrograde dissection Mastoid dissection 15 16 8 17 18 9 19 20 10 Superficial Parotidectomy Surgical goals • Avoid facial nerve injury • Remove tumor with surrounding -

Outpatient Versus Inpatient Superficial Parotidectomy: Clinical and Pathological Characteristics Daniel J
Lee et al. Journal of Otolaryngology - Head and Neck Surgery (2021) 50:10 https://doi.org/10.1186/s40463-020-00484-9 ORIGINAL RESEARCH ARTICLE Open Access Outpatient versus inpatient superficial parotidectomy: clinical and pathological characteristics Daniel J. Lee1†, David Forner1,2†, Christopher End3, Christopher M. K. L. Yao1, Shireen Samargandy1, Eric Monteiro1,4, Ian J. Witterick1,4 and Jeremy L. Freeman1,4* Abstract Background: Superficial parotidectomy has a potential to be performed as an outpatient procedure. The objective of the study is to evaluate the safety and selection profile of outpatient superficial parotidectomy compared to inpatient parotidectomy. Methods: A retrospective review of individuals who underwent superficial parotidectomy between 2006 and 2016 at a tertiary care center was conducted. Primary outcomes included surgical complications, including transient/ permanent facial nerve palsy, wound infection, hematoma, seroma, and fistula formation, as well as medical complications in the postoperative period. Secondary outcome measures included unplanned emergency room visits and readmissions within 30 days of operation due to postoperative complications. Results: There were 238 patients included (124 in outpatient and 114 in inpatient group). There was no significant difference between the groups in terms of gender, co-morbidities, tumor pathology or tumor size. There was a trend towards longer distance to the hospital from home address (111 Km in inpatient vs. 27 in outpatient, mean difference 83 km [95% CI,- 1 to 162 km], p = 0.053). The overall complication rates were comparable between the groups (24.2% in outpatient group vs. 21.1% in inpatient, p = 0.56). There was no difference in the rate of return to the emergency department (3.5% vs 5.6%, p = 0.433) or readmission within 30 days (0.9% vs 0.8%, p = 0.952). -

Surgical Treatment of Chronic Parotitis
Published online: 2018-10-24 THIEME Original Research 83 Surgical Treatment of Chronic Parotitis Rik Johannes Leonardus van der Lans1 Peter J.F.M. Lohuis1 Joost M.H.H. van Gorp2 Jasper J. Quak1 1 Department of ENT & Head and Neck Surgery, Diakonessenhuis, Address for correspondence Rik Johannes Leonardus van der Lans, Utrecht, Netherlands MD, Department of ENT- & Head and Neck Surgery, Diakonessenhuis, 2 Department of Pathology, Diakonessenhuis, Utrecht, Netherlands location Utrecht, Bosboomstraat 1, 3582 KE, Utrecht, Netherlands (e-mail: [email protected]). Int Arch Otorhinolaryngol 2019;23:83–87. Abstract Introduction chronic parotitis (CP) is a hindering, recurring inflammatory ailment that eventually leads to the destruction of the parotid gland. When conservative measures and sialendoscopy fail, parotidectomy can be indicated. Objective to evaluate the efficacy and safety of parotidectomy as a treatment for CP unresponsive to conservative therapy, and to compare superficial and near-total parotidectomy (SP and NTP). Methods retrospective consecutive case series of patients who underwent paroti- dectomy for CP between January 1999 and May 2012. The primary outcome variables were recurrence, patient contentment, transient and permanent facial nerve palsy and Frey syndrome. The categorical variables were analyzed using the two-sided Fisher exact test. Alongside, an elaborate review of the current literature was conducted. Results a total of 46 parotidectomies were performed on 37 patients with CP. Near- total parotidectomy was performed in 41 and SP in 5 cases. Eighty-four percent of patients was available for the telephone questionnaire (31 patients, 40 parotidec- tomies) with a mean follow-up period of 6,2 years. Treatment was successful in 40/46 parotidectomies (87%) and 95% of the patients were content with the result. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Phenobarbital-Responsive Bilateral Zygomatic Sialadenitis Following an Enterotomy in a Cavalier King Charles Spaniel
Research Journal for Veterinary Practitioners Case Report Phenobarbital-Responsive Bilateral Zygomatic Sialadenitis following an Enterotomy in a Cavalier King Charles Spaniel PAOUL S MARTINEZ, RENEE CARTER, LORRIE GASCHEN, KIRK RYAN Department of Veterinary Clinical Sciences, School of Veterinary Medicine Louisiana State University, Baton Rouge, LA 70803, USA. Abstract | A 6 year old male castrated Cavalier King Charles Spaniel presented to the Louisiana State University Veterinary Teaching Hospital for a three day history of bilateral acute trismus, exophthalmos, and blindness. These signs developed after an exploratory laparotomy and gastrointestinal foreign body removal was performed. On pre- sentation, the ophthalmic examination revealed bilateral decreased retropulsion, absent bilateral direct and consensual pupillary light responses, bilateral blindness, and a superficial ulcer in right eye. Ocular ultrasound and computed to- mography of the skull were performed and identified a bilateral retrobulbar mass effect originating from the zygomatic salivary glands. Ultrasound guided fine needle aspirate cytology revealed neutrophilic inflammation. Fungal testing and bacterial cultures were performed which were negative for identification of an infectious organism. The patient was placed on a 5-day course of antibiotic therapy and the response was poor. Phenobarbital was added to the treatment regimen. Two days following phenobarbital administration, the exophthalmos and trismus began to resolve. Following phenobarbital therapy, ocular position normalized, trismus completely resolved, and patient returned to normal behav- ior although blindness remained in both eyes. No other neurologic condition occurred. This paper highlights the early use of phenobarbital for the rapid resolution of zygomatic sialadenitis. Keywords | Ultrasound, Sialadenitis, Bilateral exophthalmos, Biomicroscopy, Neutrophilic inflammation Editor | Muhammad Abubakar, National Veterinary Laboratories, Islamabad, Pakistan. -

Salivary Glands
GASTROINTESTINAL SYSTEM [Anatomy and functions of salivary gland] 1 INTRODUCTION Digestive system is made up of gastrointestinal tract (GI tract) or alimentary canal and accessory organs, which help in the process of digestion and absorption. GI tract is a tubular structure extending from the mouth up to anus, with a length of about 30 feet. GI tract is formed by two types of organs: • Primary digestive organs. • Accessory digestive organs 2 Primary Digestive Organs: Primary digestive organs are the organs where actual digestion takes place. Primary digestive organs are: Mouth Pharynx Esophagus Stomach 3 Anatomy and functions of mouth: FUNCTIONAL ANATOMY OF MOUTH: Mouth is otherwise known as oral cavity or buccal cavity. It is formed by cheeks, lips and palate. It encloses the teeth, tongue and salivary glands. Mouth opens anteriorly to the exterior through lips and posteriorly through fauces into the pharynx. Digestive juice present in the mouth is saliva, which is secreted by the salivary glands. 4 ANATOMY OF MOUTH 5 FUNCTIONS OF MOUTH: Primary function of mouth is eating and it has few other important functions also. Functions of mouth include: Ingestion of food materials. Chewing the food and mixing it with saliva. Appreciation of taste of the food. Transfer of food (bolus) to the esophagus by swallowing . Role in speech . Social functions such as smiling and other expressions. 6 SALIVARY GLANDS: The saliva is secreted by three pairs of major (larger) salivary glands and some minor (small) salivary glands. Major glands are: 1. Parotid glands 2. Submaxillary or submandibular glands 3. Sublingual glands. 7 Parotid Glands: Parotid glands are the largest of all salivary glands, situated at the side of the face just below and in front of the ear. -

Three-Dimensional Reconstruction of the Facial Nerve Course in Parotid Gland Tumor Using Double Echo Steady State with Water-Excitation Magnetic Resonance Images
Precision and Future Medicine 2020;4(2):75-80 CASE https://doi.org/10.23838/pfm.2020.00086 REPORT pISSN: 2508-7940 · eISSN: 2508-7959 Three-dimensional reconstruction of the facial nerve course in parotid gland tumor using double echo steady state with water-excitation magnetic resonance images 1 2 2 1 Yong Gi Jung , Yi-Kyung Kim , Hyung-Jin Kim , Han-Sin Jeong 1 DepartmentofOtorhinolaryngologyHeadandNeckSurgery,SamsungMedicalCenter,SungkyunkwanUniversitySchoolof Medicine,Seoul,Korea 2 DepartmentofRadiology,SamsungMedicalCenter,SungkyunkwanUniversitySchoolofMedicine,Seoul,Korea Received: May 7, 2020 Revised: May 28, 2020 Accepted: May 29, 2020 ABSTRACT Functionalpreservationofthefacialnerve(FN)isessentialinparotidtumorsurgery. Corresponding author: Han-Sin Jeong Recently,directvisualizationoftheFNintheparotidgland(double-echosteady-state Department of sequencewithwaterexcitationmagneticresonanceimaging[DESS-WE-MRI])hasbeen Otorhinolaryngology Head attemptedwithpromisingdiagnosticaccuracy.Inthisreport,wepresentthree-dimen- and Neck Surgery, Samsung sional(3D)reconstructionoftheFNcourseintwoparotidglandtumorcasesusing Medical Center, Sungkyunkwan DESS-WE-MRIimagesforthefirsttime.Onepatienthadarecurrentbenignparotid University School of Medicine, glandtumor,whiletheotherpatienthadamalignantparotidglandtumor.Re- 81 Irwon-ro, Gangnam-gu, gions-of-interestincludingtheFNandthetumorsweremanuallyselectedineachsec- Seoul 06351, Korea tionoftheDESS-WE-MRIimages.The3DrenderingswerethencreatedwithanIn-Vesal- Tel: +82-2-3410-3579 iussoftware.TheFNswerewell-demarcatedtothetemporofacialandcervicofacial -
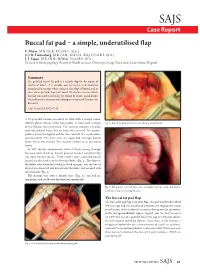
Buccal Fat Pad – a Simple, Underutilised Flap E
SAJS Case Report Buccal fat pad – a simple, underutilised flap E. Meyer, M.B. Ch.B., F.C.O.R.L. (S.A.) S. J. R. Liebenberg, M.B. Ch.B., M.R.C.S. (Ed.), F.C.O.R.L. (S.A.) J. J. Fagan, M.B. Ch.B., M.Med., F.C.O.R.L. (S.A.) Division of Otolaryngology, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital Summary The pedicled buccal fat pad is a reliable flap for the repair of small oral defects. It is durable, easy to harvest, and should be considered in settings where access to free flaps is limited and in cases where previous flaps have failed. We discuss a case in which this flap was used successfully for closure of an oro-antral fistula. The indications, anatomy and techniques of successful harvest are discussed. S Afr J Surg 2012;50(2):47-49. A 57-year-old woman presented in 1998 with a benign minor salivary gland tumour of the hard palate. A wide local excision Fig. 2. Buccal fat pad sutured to cover the oro-antral fistula. of the tumour was performed. The excision margins extended onto the palatal bone, but no bone was excised. The greater palatine artery was ligated and the bone was left to re-epithelialise spontaneously. Two years later, she again had a benign palatal lesion which was excised. The surgery resulted in an oro-antral fistula. In 2007 she was symptomatic, with all fluids coming through her nose when drinking. A local gingival mucosal rotational flap was done without success. -

Distribution and Roles of Substance P in Human Parotid Duct
IJAE Vol. 121, n. 3: 219-225, 2016 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research article - Histology and cell biology Distribution and roles of substance P in human parotid duct Kaori Amano1,*, Osamu Amano2, George Matsumura3, Kazuyuki Shimada4 1,3Department of Anatomy, Kyorin University School of Medicine; 2Department of Anatomy, Meikai University School of Dentistry; 4Kagoshima University Abstract Sialadenitis occurs with greatest frequency in the parotid glands because infection and inflam- mation arise easily from the oral cavity. Since patients often experience severe swelling and pain during inflammation, the distribution of sensory nerves in these ducts may have clini- cal significance. We used antibodies to the known neuropeptide substance P and to tyrosine hydroxylase - a marker of adrenergic fibres - to observe their distribution and gain insight on their functional role in adult human parotid duct. After excising the parotid duct along with the gland, specimens were divided into three regions: the tract adjacent to the parotid gland, the route along the anterior surface of the masseter, and the area where the duct penetrates the buc- cinator muscle and opens into the oral cavity. Specimens were prepared and examined under a fluorescence microscope following immunostaining. Substance P positivity was observed in all three regions of the duct, whereas tyrosine hydroxylase was distributed mainly in the vas- cular walls and surrounding areas. The distribution of substance P candidates this molecule to assist in tissue defense in conjunction with the blood and lymph vessels of this area. Tyrosine hydroxylase in the blood vessel wall likely contributes to regulation of blood flow in concert with substance P positive nerves surrounding the blood vessels.