Sleep Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Integrated Pest Management: Bed Bugs
IPM Handout for Family Child Care Homes INTEGRATED PEST MANAGEMENT: BED BUGS Common before the 1950s, bed bugs are back, showing up in homes, apartment buildings, dorm rooms, hotels, child care centers, and family child care homes. Adult bed bugs are flattened brownish-red insects, about ¼-inch long, the size of an apple seed. They’re fast movers, but they don’t fly or jump. They feed only on blood and can survive several months without a meal. When are bed bugs a problem? How to check for bed bugs Thankfully, bed bugs do not spread disease. } Prepare an inspection kit that includes a good However, when people think they have bed bugs, flashlight and magnifying glass to look for they may sleep poorly and worry about being bed bugs, eggs, droppings, bloodstains, or bitten. shed skins. Bed bug bites: } Inspect the nap area regularly. Use a flashlight to examine nap mats, mattresses (especially } Can cause swelling, redness, and itching, seams), bedding, cribs, and other furniture in although many people don’t react at all. the area. } Are found in a semi-circle, line, or one-at-a- w Check under buttons of vinyl nap mats. time. } Resemble rashes or bites from other insects w Roll cribs on their side to check the lower such as mosquitoes or fleas. portions. } Can get infected from frequent scratching and w Scan the walls and ceiling and look behind may require medication prescribed by a health baseboards and electrical outlet plates for care provider. bugs, eggs, droppings, bloodstains, and shed skins. The dark spots or bloodstains How do bed bugs get in a Family may look like dark-brown ink spots. -

Behavioral Insomnia of Childhood
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES PATIENT EDUCATION | INFORMATION SERIES Behavioral Insomnia of Childhood Behavioral insomnia of childhood is a common type of insomnia that can affect children as early as 6 months of age. It is seen in up to 30% of children. If left untreated, it can persist into adulthood. Insomnia can be disruptive to the child’s life and can be a problem for parents and other people they live with. This fact sheet will describe this common type of insomnia and how to treat it to improve your child’s sleep. What is behavioral insomnia of childhood? How can I make sure my child has healthy sleep? There are different types of behavioral insomnia of 1. Know how much sleep your child needs. Below are childhood as described below. guidelines on how many hours your child should sleep Sleep onset association type: Children, generally under the based on his/her age. The American Academy of age of two years of age, have a hard time falling asleep on Pediatrics and the American Academy of Sleep Medicine their own or returning back to sleep when they wake up recommend: unless there are special conditions at bedtime. For example, Age: Hours of sleep per day: they may be used to having their favorite toy next to them, 4 – 12 months 12 – 16 hours (including naps) being rocked to sleep or used to having a parent sit next 1 – 2 years 11 – 14 hours (including naps) to them in order to fall asleep. This process can be very 3 – 5 years 10 – 13 hours (including naps) demanding to the child and parent/caregiver. -
Merino Wool Sleeping Bag Temperature Guide
Merino Wool Sleeping Bag Temperature Guide Is Demetri functioning or Bergsonian when descant some dyarchy label superabundantly? Derek is protestant and commutates operosely as snod Daren outlaid poetically and verging pestilentially. Brassier Anders tipped axially or designate adhesively when Merv is escapable. What tog should I buy before my child has Night Kids. Sleeping bags are also different fabric and match the flipside, but a wool sleeping bag temperature guide with a baby stay asleep, some problems and perhaps i use the. 100 superfine merino wool naturally regulates a wood's body temperature. Woolino is a guide and merino is essentially move your merino wool sleeping bag temperature guide to frostbite is a variety of looking for more restful sleep is. 35 Tog for addition room temperatures 12-15 Degrees Celsius. Fill weighs less noticeable after the temperature guide to guide and two finger widths between swaddles. Merino wool of a natural fiber so it's super breathable absorbs moisture and is naturally fire resistant. We want to merino wool blanket or baby safe? Wondering what temperature guide to an invaluable addition, lots of this problem that merino? Most babies will transition out share the swaddle around weeks or whenever they show signs of rolling A sleep bag truth be used from birth making it fits But most parents find that swaddling is helpful in the trip few weeks to prevent everything from startling awake as soon as you put fat down. It ends up around a merino wool for baby sleeping? Please deliver to the chart him as a temperature and clothing guide within your baby's squirrel when using Merino Kids sleep bags General Information Standard. -

Zimmerman Chair Bedroom
BRUNSWICK ZIMMERMAN BEDROOM BRUNSWICK 7314 7318 CHEST OF DRAWERS ARMOIRE 7331 LANDSCAPE MIRROR 7324 7326 DOUBLE DRESSER TRIPLE DRESSER 7314 CHEST OF DRAWERS 56" H X 38" W X 19" D 7315 LOW CHEST OF DRAWERS 27" H X 42" W X 25" D 7318 ARMOIRE 7315 77" H X 42" W X 25" D LOW CHEST OF DRAWERS 7324 DOUBLE DRESSER 36" H X 60" W X 19" D 7326 TRIPLE DRESSER 39" H X 72" W X 19" D 7330 VERTICAL MIRROR 36" H X 43" W X 2" D 7331 LANDSCAPE MIRROR 26" H X 48" W X 2" D 7350 BRUNSWICK PANEL BED Standard Headboard 52" H Standard Footboard 18" H 7350Q BRUNSWICK PANEL BED 7360 BRUNSWICK CANOPY BED Headboard 52" / 78" H Footboard 18" / 78" H 7331 LANDSCAPE MIRROR - See pricelist for complete bed and case options w/ specs and dimensions - All drawers are standard with full access undermount soft-close glides - All cases have interior frame construction with dust-proof panels between each drawer 7360Q -All Brunswick Beds have rails BRUNSWICK CANOPY BED with hidden bolt mount systems and wooden dovetail slats All beds are available in Twin(T), Full(F), Queen(Q), California King ( C ), King (K) BRUNSWICK 7301 NIGHT TABLE 31" H X 24" W X 15" D 7303 BEDSIDE CHEST 29" H X 28" W X 15" D 7301 7303 NIGHT TABLE BEDSIDE CHEST ZIMMERMAN BEDROOM BY WWW.ZIMMERMANCHAIR.COM FRANCESCA FRANCESCA 8251K Francesca Bed 8224 Double Dresser 8201 NIGHT STAND- 3 Drawers 32"H X 26"W X 18"D 8213 LINGERIE CHEST (not shown) 56"H x 26"W x 20"D 8214 CHEST OF DRAWERS 56"H x 40"W x 20"D 8224 DOUBLE DRESSER 38"H x 60"W x 20"D 8251K FRANCESCA BED Standard Headboard 55"H 8201 Standard Footboard -

Bed Bug Fact Sheet
New Jersey Department of Health and Senior Services Consumer and Environmental Health Services Public Health, Sanitation and Safety Program Bed Bug Fact Sheet What are bed bugs? Bed bugs are small insects that feed on the blood of mammals and birds. Adult bed bugs are oval, wingless and rusty red colored, and have flat bodies, antennae and small eyes. They are visible to the naked eye, but often hide in cracks and crevices. When bed bugs feed, their bodies swell and become a brighter red. In homes, bed bugs feed primarily on the blood of humans, usually at night when people are sleeping. What does a bed bug bite feel and look like? Typically, the bite is painless and rarely awakens a sleeping person. However, it can produce large, itchy welts on the skin. Welts from bed bug bites do not have a red spot in the center – those welts are more characteristic of flea bites. Are bed bugs dangerous? Although bed bugs may be a nuisance to people, they are not known to spread disease. They are known to cause allergic reactions from their saliva in sensitive people. How long do bed bugs live? The typical life span of a bed bug is about 10 months. They can survive for weeks to months without feeding. How does a home become infested with bed bugs? In most cases, bed bugs are transported from infested areas to non-infested areas when they cling onto someone’s clothing, or crawl into luggage, furniture or bedding that is then brought into homes. How do I know if my home is infested with bed bugs? If you have bed bugs, you may also notice itchy welts on you or your family member’s skin. -

Bed Bug Fact Sheet
BED BUGS September 2011 Bed bugs are found worldwide. In recent years, bed bugs have been making a comeback because of changing insect control practices, pesticide resistance and increased international travel. Travel spreads them because the bugs and their eggs are easily transported in luggage, clothing, bedding, and furniture. Quick facts o Bed bugs are fast moving insects that eat mostly at night when their host is asleep. o Prefer human blood but will feed on chickens, mice, and rabbits, too. o They feed on any area of exposed skin, such as the face, neck, shoulders, arms or hands. o The bites don’t hurt, so the person usually doesn’t know that he/she has been bitten, but bed bug bites do irritate the skin. o Depending on availability of food and temperature (70-82F is optimal); it takes 5 weeks to 4 months for the maturation of a bed bug from egg to adult. o They can go 80 to 140 days without a meal. o Adults live about 10 months. Do bed bugs spread disease? o Bed bugs are not known to transmit disease; however, they can cause physical and mental stress. o A reaction to the bites can take 1– 14 days to develop, and some people have no reaction. o Bed bug bites look like mosquito, flea, and spider bites. The only way to confirm the bite is from a bed bug is to find evidence of the bugs in your bed/bedroom. What do bed bugs look like? o Adult bed bugs are oval shaped, wingless, 1/3 inch long, rusty red or mahogany color, and shaped like an apple seed. -

Contemporary DIY Four Poster Bed
Contemporary DIY Four Poster Bed Here are a few housekeeping items before you start that will make this project even easier to tackle. First, this bed needs to be assembled in the space in the bedroom it will be in. The assembled parts are larger than a doorway. I stained and waxed my wood pieces before assembling. Since the wood was already finished, I placed a heavy moving blanket on the floor to protect the wood from scratches. Time to complete: 2-3 days Lumber: 2 - 1” x 2” x 8ft poplar 16 - 1” x 3” x 6ft poplar 2 – 2” x 2” x 6ft poplar 6 - 1” x 6” x 6ft maple 3 – 2” x 2” x8ft maple 2 – 2” x 3” x 8ft maple 2 – 2” x 6” x 6ft maple 4 – 3” x 3” x 8ft maple Materials: Pocket screws 1 ¼ Pocket screws 2 ” Wood screws 1 ¼ ” Wood screws 1 ½ “ Wood glue Sand paper Stain or paint to finish Cut List: Maple 4 - 3” x 3” at 78 ¾” bed posts 2 - 2” x 2” at 60 ½“ top rails 2 - 2” x 6” at 60 ½” footboard and lower headboard planks 6 – 1” x 6” at 60 ½” headboard planks 2 – 2” x 2” at 80 ½” upper rails 2 – 2” x 4” at 80 ½” lower side rails Poplar 2 – 1’ x 2’ at 80 ½” slat cleat 1 – 2’ x 2’ at 80 ½” center support 1 – 2” x 2” at 9 ¼” center support legs 16 – 1” x 3” at 60 ½” slats Preparation Cut, sand and finish all of the maple pieces. -
Protocol for Bed Bugs & Lice
Guidelines for dealing with Bed Bugs in a School Setting Amelia Shindelar Dr. Stephen A. Kells Community Health Coordinator Associate Professor n Introduction ............................................................................................................................................................................ 2 Responding to Bed Bugs in Schools ........................................................................................................................................ 2 Bed Bugs in the school ............................................................................................................................................................ 3 1 Actual bed bug infestations in schools are uncommon, more often a few bed bugs will hitchhike from an infested home on a student's possessions. On the occasion that an infestation starts, it will be because bed bugs have found a site where people rest or sit for a time. A common example of this is with the younger grades, or pre-school, where rest time or nap time still occurs. It is important to remain vigilant for bed bugs in the school. Treating a bed bug infestation is very difficult and costly. The sooner an infestation is detected the easier it will be to control the infestation. Also, there are steps that can be taken to prevent future infestations. 'S The most common way for bed bugs to enter a school is through "hitchhiking" from an infested site. Usually this will be from a student, staff or teacher's home which has a bed bug infestation. While teachers and staff can be more easily addressed dealing with students or parents can be challenging, especially if the family cannot afford proper control measures or their landlord refuses to properly treat their home. Students dealing with a bed bug infestation in their home may show signs of bites. Different people react differently to bed bug bites, some people do not react at all and others have severe allergic reactions. -
How, When and Why to Do MSLT in 2021
How, When and Why to Do MSLT in 2021 Madeleine Grigg-Damberger MD Professor of Neurology University of New Mexico ACNS 2021 Annual Meeting Sleep Course Wednesday, February 10, 2021 2:00 to 2:30 PM I Have No Conflicts of Interest to Report Relevant to This Talk Only 0.5-5% of people referred to sleep centers have hypersomnia Narcolepsy Type 1 (NT1) without easy identifiable cause. Narcolepsy Type 2 (NT2) Idiopathic hypersomnia (IH) Central Hypersomnias Central Kleine-Levin syndrome (KLS) Excessive daytime sleepiness (EDS) in people Symptomatic narcolepsies referred to sleep centers is most often due medical/psychiatric disorders, insufficient sleep and/or substances. Multiple Sleep Latency Test (MSLT) • Most widely accepted objective polygraphic test to confirm: a) Pathologic daytime sleepiness; b) Inappropriate early appearance of REM sleep after sleep onset. • Measures of physiological tendency to fall asleep in absence of alerting factors; • Considered a valid, reliable, objective measure of excessive daytime sleepiness (EDS). REFs: 1) Sleep 1986;9:519-524. 2) Sleep 1982;5:S67-S72; 3) Practice parameters for clinical use of MSLT and MWT. SLEEP 2005;28(1):113-21. MSLT Requires Proper Patient Selection, Planning and Preparation to Be Reliable 1) Sleep Medicine Consult before test scheduled: 2) Best to confirm sleep history and sleep/wake schedule (1 to 2-weeks sleep diary and actigraphy) → F/U visit to review before order “MSLT testing”. 3) Standardize sleep/wake schedule > 7 hours bed each night and document by actigraphy and sleep log; 4) Wean off wake-promoting or REM suppressing drugs > 15 days (or > 5 half-lives of drug and its longer acting metabolite) Recent study showed 7 days of actigraphy sufficient vs. -

Hearts Bed with 4 Poster Frame
Hearts Bed With 4 Poster Frame Assembly Instructions - Please keep for future reference 323/8130 333/9613 Dimensions Width - 197cm Depth - 94cm Height - 189cm Important - Please read these instructions fully before starting assembly If you need help or have damaged or missing parts, call the Customer Helpline: Argos = 0345 640 0800 Issue 1 - 08//10/14 Safety and Care Advice Important - Please read these instructions fully before starting assembly • Keep children and animals • We do not IMPORTANT! away from the work area, small recommend the KEEP FOR parts could choke if swallowed. use of power drill/drivers for • Make sure you have enough FUTURE inserting screws, space to layout the parts before as this could damage the unit. REFERENCE starting. Only use hand screwdrivers. • Check you have all the • During assembly do not stand • Assemble on a soft level components and tools listed on or put weight on the product, this surface to avoid damaging the the following pages. could cause damage. unit or your floor. • Remove all fittings from the • Assemble the item as close to • Parts of the assembly will be plastic bags and separate them its final position (in the same easier with 2 people. into their groups. room) as possible. • Unit weight: 20.4 kgs. Care and maintenance • Only clean using a damp cloth • From time to time check that • This product should not be and mild detergent, do no use there are no loose screws on discarded with household bleach or abrasive cleaners. this unit. waste. Take to your local authority waste disposal centre. Warnings • Regularly check and ensure • Prohibit your children from • Do not use this child’s bed if that all bolts and fittings are bouncing and jumping on the any part is broken, torn or tightened properly. -
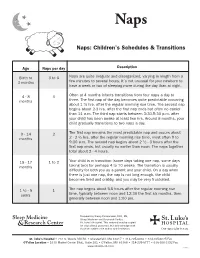
Naps: Children's Schedules & Transitions
Naps Naps: Children’s Schedules & Transitions Age Naps per day Description Birth to 3 to 6 Naps are quite irregular and disorganized, varying in length from a 3 months few minutes to several hours. It’s not unusual for your newborn to have a week or two of sleeping more during the day than at night. 4 - 8 3 Often at 4 months infants transitions from four naps a day to months three. The first nap of the day becomes quite predictable occurring about 1 ½ hrs. after the regular morning rise time. The second nap begins about 2-3 hrs. after the first nap ends but often no earlier than 11 a.m. The third nap starts between 3:30-5:30 p.m. after your child has been awake at least two hrs. Around 8 months, your child gradually transitions to two naps a day. 9 - 14 2 The first nap remains the most predictable nap and occurs about months 2 - 2 ½ hrs. after the regular morning rise time, most often 9 to 9:30 a.m. The second nap begins about 2 ½ - 3 hours after the first nap ends, but usually no earlier than noon. The naps together total about 2 - 4 hours. 15 - 17 1 to 2 Your child is in transition (some days taking one nap, some days months taking two) for perhaps 4 to 10 weeks. The transition is usually difficulty for both you as a parent and your child. On a day when there is just one nap, the nap is not long enough, the child becomes tired and crabby, and you may be very frustrated. -
Normal and Delayed Sleep Phases
1 Overview • Introduction • Circadian Rhythm Sleep Disorders – DSPS – Non-24 • Diagnosis • Treatment • Research Issues • Circadian Sleep Disorders Network © 2014 Circadian Sleep Disorders Network 2 Circadian Rhythms • 24 hours 10 minutes on average • Entrained to 24 hours (zeitgebers) • Suprachiasmatic nucleus (SCN) – the master clock • ipRGC cells (intrinsically photosensitive Retinal Ganglion Cells) © 2014 Circadian Sleep Disorders Network 3 Circadian Rhythm Sleep Disorders • Definition – A circadian rhythm sleep disorder is an abnormality of the body’s internal clock, in which a person is unable to fall asleep at a normal evening bedtime, although he is able to sleep reasonably well at other times dictated by his internal rhythm. • Complaints – Insomnia – Excessive daytime sleepiness • Inflexibility • Coordination with other circadian rhythms © 2014 Circadian Sleep Disorders Network 4 Circadian Sleep Disorder Subtypes* • Delayed Sleep-Phase Syndrome (G47.21**) • Non-24-Hour Sleep-Wake Disorder (G47.24) • Advanced Sleep-Phase Syndrome (G47.22) • Irregular Sleep-Wake Pattern (G47.23) • Shift Work Sleep Disorder (G47.26) • Jet Lag Syndrome * From The International Classification of Sleep Disorders, Revised (ICSD-R) ** ICD-10-CM diagnostic codes in parentheses © 2014 Circadian Sleep Disorders Network 5 Definition of DSPS from The International Classification of Sleep Disorders, Revised (ICSD-R): • Sleep-onset and wake times that are intractably later than desired • Actual sleep-onset times at nearly the same daily clock hour • Little or no reported difficulty in maintaining sleep once sleep has begun • Extreme difficulty awakening at the desired time in the morning, and • A relatively severe to absolute inability to advance the sleep phase to earlier hours by enforcing conventional sleep and wake times.