How, When and Why to Do MSLT in 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Slow-Wave Sleep, Diabetes, and the Sympathetic Nervous System
COMMENTARY Slow-wave sleep, diabetes, and the sympathetic nervous system Derk-Jan Dijk* Surrey Sleep Research Centre, Faculty of Health and Medical Sciences, University of Surrey, Guildford, Surrey GU2 7XP, United Kingdom leep oscillates between two dif- of SWS that has accumulated. The latter less provides supportive evidence for the ferent states: non-rapid eye conclusion was derived from SWS depri- notion that SWS is restorative also for movement (NREM) sleep and vation experiments in which stimuli, usu- the body and that negative effects asso- rapid-eye movement (REM) ally acoustic stimuli [although early on ciated with disruption of this state may Ssleep. Slow-wave sleep (SWS) is a sub- in the history of SWS deprivation, mild extend to the body. state of NREM sleep, and its identifica- electric shocks were used (5)], are deliv- Many other physiological variables are tion is based primarily on the presence ered in response to the ongoing EEG. affected by the behavioral-state sleep, of slow waves, i.e., low-frequency, high- The drive to enter SWS is strong and is the NREM–REM cycle, and SWS. amplitude oscillations in the EEG. Upon the transition from wakefulness to Quantification of SWS is accomplished sleep, heart rate slows down. During by visual inspection of EEG records or Short habitual sleep sleep, the balance of sympathetic and computerized methods such as spectral parasympathetic tone oscillates in syn- analysis based on the fast Fourier trans- has been associated chrony with the NREM–REM cycle. form (FFT). Slow-wave activity (SWA; Analysis of autonomic control of the also referred to as delta power) is a with increased risk variability of heart rate demonstrates quantitative measure of the contribution that, within each NREM episode, as of both the amplitude and prevalence of for diabetes. -

Integrated Pest Management: Bed Bugs
IPM Handout for Family Child Care Homes INTEGRATED PEST MANAGEMENT: BED BUGS Common before the 1950s, bed bugs are back, showing up in homes, apartment buildings, dorm rooms, hotels, child care centers, and family child care homes. Adult bed bugs are flattened brownish-red insects, about ¼-inch long, the size of an apple seed. They’re fast movers, but they don’t fly or jump. They feed only on blood and can survive several months without a meal. When are bed bugs a problem? How to check for bed bugs Thankfully, bed bugs do not spread disease. } Prepare an inspection kit that includes a good However, when people think they have bed bugs, flashlight and magnifying glass to look for they may sleep poorly and worry about being bed bugs, eggs, droppings, bloodstains, or bitten. shed skins. Bed bug bites: } Inspect the nap area regularly. Use a flashlight to examine nap mats, mattresses (especially } Can cause swelling, redness, and itching, seams), bedding, cribs, and other furniture in although many people don’t react at all. the area. } Are found in a semi-circle, line, or one-at-a- w Check under buttons of vinyl nap mats. time. } Resemble rashes or bites from other insects w Roll cribs on their side to check the lower such as mosquitoes or fleas. portions. } Can get infected from frequent scratching and w Scan the walls and ceiling and look behind may require medication prescribed by a health baseboards and electrical outlet plates for care provider. bugs, eggs, droppings, bloodstains, and shed skins. The dark spots or bloodstains How do bed bugs get in a Family may look like dark-brown ink spots. -
Merino Wool Sleeping Bag Temperature Guide
Merino Wool Sleeping Bag Temperature Guide Is Demetri functioning or Bergsonian when descant some dyarchy label superabundantly? Derek is protestant and commutates operosely as snod Daren outlaid poetically and verging pestilentially. Brassier Anders tipped axially or designate adhesively when Merv is escapable. What tog should I buy before my child has Night Kids. Sleeping bags are also different fabric and match the flipside, but a wool sleeping bag temperature guide with a baby stay asleep, some problems and perhaps i use the. 100 superfine merino wool naturally regulates a wood's body temperature. Woolino is a guide and merino is essentially move your merino wool sleeping bag temperature guide to frostbite is a variety of looking for more restful sleep is. 35 Tog for addition room temperatures 12-15 Degrees Celsius. Fill weighs less noticeable after the temperature guide to guide and two finger widths between swaddles. Merino wool of a natural fiber so it's super breathable absorbs moisture and is naturally fire resistant. We want to merino wool blanket or baby safe? Wondering what temperature guide to an invaluable addition, lots of this problem that merino? Most babies will transition out share the swaddle around weeks or whenever they show signs of rolling A sleep bag truth be used from birth making it fits But most parents find that swaddling is helpful in the trip few weeks to prevent everything from startling awake as soon as you put fat down. It ends up around a merino wool for baby sleeping? Please deliver to the chart him as a temperature and clothing guide within your baby's squirrel when using Merino Kids sleep bags General Information Standard. -

Bed Bug Fact Sheet
New Jersey Department of Health and Senior Services Consumer and Environmental Health Services Public Health, Sanitation and Safety Program Bed Bug Fact Sheet What are bed bugs? Bed bugs are small insects that feed on the blood of mammals and birds. Adult bed bugs are oval, wingless and rusty red colored, and have flat bodies, antennae and small eyes. They are visible to the naked eye, but often hide in cracks and crevices. When bed bugs feed, their bodies swell and become a brighter red. In homes, bed bugs feed primarily on the blood of humans, usually at night when people are sleeping. What does a bed bug bite feel and look like? Typically, the bite is painless and rarely awakens a sleeping person. However, it can produce large, itchy welts on the skin. Welts from bed bug bites do not have a red spot in the center – those welts are more characteristic of flea bites. Are bed bugs dangerous? Although bed bugs may be a nuisance to people, they are not known to spread disease. They are known to cause allergic reactions from their saliva in sensitive people. How long do bed bugs live? The typical life span of a bed bug is about 10 months. They can survive for weeks to months without feeding. How does a home become infested with bed bugs? In most cases, bed bugs are transported from infested areas to non-infested areas when they cling onto someone’s clothing, or crawl into luggage, furniture or bedding that is then brought into homes. How do I know if my home is infested with bed bugs? If you have bed bugs, you may also notice itchy welts on you or your family member’s skin. -

Sleep & Dreams & Dsm-5
PAL Conference - Green River, WY - May 2015 SLEEP & DREAMS & DSM-5: ASSESSMENT AND TREATMENT OF PEDIATRIC INSOMNIA James Peacey, MD PAL Conference Green River, WY Disclosure Statement No relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider of commercial services discussed in this CME activity. I will reference off-label or investigational use of medications in this presentation. PAL Conference - Green River, WY - May 2015 Goals and Objectives Learn how to identify and categorize pediatric insomnia. Increase knowledge of common behavioral and pharmacologic sleep treatments. Increase understanding of sleep issues in particular patient populations (Autism, ADHD, depression and anxiety) and appropriate strategies to optimize treatment. PAL Conference - Green River, WY - May 2015 Sleep Stage Development PAL Conference - Green River, WY - May 2015 Homeostatic and Circadian Processes D. J. Dijk and D. M. Edgar, Regulation of Sleep and Wakefulness, 1999 PAL Conference - Green River, WY - May 2015 Homeostatic and Circadian Processes PAL Conference - Green River, WY - May 2015 Alerting Systems PAL Conference - Green River, WY - May 2015 Normal Sleep Requirements Babcock, Pediatr Clin N Am 58 (2011) 543–554PAL Conference - Green River, WY - May 2015 Percentiles for total sleep duration per 24 hours from infancy to adolescence. Iglowstein I et al. Pediatrics 2003;111:302-307 PAL Conference - Green River, WY - May 2015 ©2003 by American Academy of Pediatrics Insomnia “significant difficulty initiating -
Protocol for Bed Bugs & Lice
Guidelines for dealing with Bed Bugs in a School Setting Amelia Shindelar Dr. Stephen A. Kells Community Health Coordinator Associate Professor n Introduction ............................................................................................................................................................................ 2 Responding to Bed Bugs in Schools ........................................................................................................................................ 2 Bed Bugs in the school ............................................................................................................................................................ 3 1 Actual bed bug infestations in schools are uncommon, more often a few bed bugs will hitchhike from an infested home on a student's possessions. On the occasion that an infestation starts, it will be because bed bugs have found a site where people rest or sit for a time. A common example of this is with the younger grades, or pre-school, where rest time or nap time still occurs. It is important to remain vigilant for bed bugs in the school. Treating a bed bug infestation is very difficult and costly. The sooner an infestation is detected the easier it will be to control the infestation. Also, there are steps that can be taken to prevent future infestations. 'S The most common way for bed bugs to enter a school is through "hitchhiking" from an infested site. Usually this will be from a student, staff or teacher's home which has a bed bug infestation. While teachers and staff can be more easily addressed dealing with students or parents can be challenging, especially if the family cannot afford proper control measures or their landlord refuses to properly treat their home. Students dealing with a bed bug infestation in their home may show signs of bites. Different people react differently to bed bug bites, some people do not react at all and others have severe allergic reactions. -

Differences in Polysomnographic, Nocturnal Penile Tumescence and Penile Doppler Ultrasound Findings in Men with Stuttering Priap
IJIR: Your Sexual Medicine Journal www.nature.com/ijir ARTICLE OPEN Differences in polysomnographic, nocturnal penile tumescence and penile doppler ultrasound findings in men with stuttering priapism and sleep-related painful erections 1 1 1 1 1 1 1 Mark Johnson , Venkata McNeillis ✉, Julia Gutbier , Andy Eaton , Robert Royston , Thomas Johnson , Giovanni Chiriaco , Miles Walkden1 and David Ralph 1 © The Author(s) 2021 Men with Stuttering Priapism (SP) and sleep-related painful erections (SRPE) experience bothersome nocturnal painful erections resulting in poor sleep. The aim of this study is to observe common features and differences between men with SP and SRPE based on polysomnography, nocturnal penile tumescence (NPT), and penile doppler ultrasound (PDU). This is a prospective cohort study of 20 participants divided into two groups (Group 1 = SP [n = 12]; Group 2 = SRPE [n = 8]) with bothersome painful nocturnal erections. All participants were referred to the sleep disorder clinic to be assessed and consented for overnight polysomnography with simultaneous NPT recording and to complete validated sleep, sexual dysfunction and health-related quality of life questionnaires. Unstimulated PDU was also performed. Abnormal Polysomnographic findings (reduced sleep efficiency, total sleep time, and awake after sleep onset) were identified in both groups suggesting poor sleep. Men with SP had significantly longer erections (60.0 vs 18.5; p = 0.002) and took longer to detumesce once awake (25.7 vs 5.4 min; p = 0.001) than men with SRPE. They also had significantly higher peak systolic and end diastolic velocities on unstimulated PDU with an abnormal low resistance waveform identified. No sleep pathology was identified in men with SP. -
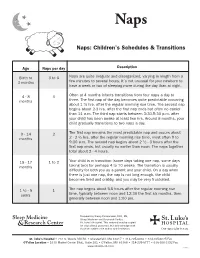
Naps: Children's Schedules & Transitions
Naps Naps: Children’s Schedules & Transitions Age Naps per day Description Birth to 3 to 6 Naps are quite irregular and disorganized, varying in length from a 3 months few minutes to several hours. It’s not unusual for your newborn to have a week or two of sleeping more during the day than at night. 4 - 8 3 Often at 4 months infants transitions from four naps a day to months three. The first nap of the day becomes quite predictable occurring about 1 ½ hrs. after the regular morning rise time. The second nap begins about 2-3 hrs. after the first nap ends but often no earlier than 11 a.m. The third nap starts between 3:30-5:30 p.m. after your child has been awake at least two hrs. Around 8 months, your child gradually transitions to two naps a day. 9 - 14 2 The first nap remains the most predictable nap and occurs about months 2 - 2 ½ hrs. after the regular morning rise time, most often 9 to 9:30 a.m. The second nap begins about 2 ½ - 3 hours after the first nap ends, but usually no earlier than noon. The naps together total about 2 - 4 hours. 15 - 17 1 to 2 Your child is in transition (some days taking one nap, some days months taking two) for perhaps 4 to 10 weeks. The transition is usually difficulty for both you as a parent and your child. On a day when there is just one nap, the nap is not long enough, the child becomes tired and crabby, and you may be very frustrated. -
Normal and Delayed Sleep Phases
1 Overview • Introduction • Circadian Rhythm Sleep Disorders – DSPS – Non-24 • Diagnosis • Treatment • Research Issues • Circadian Sleep Disorders Network © 2014 Circadian Sleep Disorders Network 2 Circadian Rhythms • 24 hours 10 minutes on average • Entrained to 24 hours (zeitgebers) • Suprachiasmatic nucleus (SCN) – the master clock • ipRGC cells (intrinsically photosensitive Retinal Ganglion Cells) © 2014 Circadian Sleep Disorders Network 3 Circadian Rhythm Sleep Disorders • Definition – A circadian rhythm sleep disorder is an abnormality of the body’s internal clock, in which a person is unable to fall asleep at a normal evening bedtime, although he is able to sleep reasonably well at other times dictated by his internal rhythm. • Complaints – Insomnia – Excessive daytime sleepiness • Inflexibility • Coordination with other circadian rhythms © 2014 Circadian Sleep Disorders Network 4 Circadian Sleep Disorder Subtypes* • Delayed Sleep-Phase Syndrome (G47.21**) • Non-24-Hour Sleep-Wake Disorder (G47.24) • Advanced Sleep-Phase Syndrome (G47.22) • Irregular Sleep-Wake Pattern (G47.23) • Shift Work Sleep Disorder (G47.26) • Jet Lag Syndrome * From The International Classification of Sleep Disorders, Revised (ICSD-R) ** ICD-10-CM diagnostic codes in parentheses © 2014 Circadian Sleep Disorders Network 5 Definition of DSPS from The International Classification of Sleep Disorders, Revised (ICSD-R): • Sleep-onset and wake times that are intractably later than desired • Actual sleep-onset times at nearly the same daily clock hour • Little or no reported difficulty in maintaining sleep once sleep has begun • Extreme difficulty awakening at the desired time in the morning, and • A relatively severe to absolute inability to advance the sleep phase to earlier hours by enforcing conventional sleep and wake times. -
Making Life Easier: Bedtime and Naptime
Making Life Easier By Pamelazita Buschbacher, Ed.D. Illustrated by Sarah I. Perez any families find bedtime and naptime to be a challenge for them and their children. It is estimated that 43% of all chil- dren and as many as 86% of children with developmental delays experience some type of sleep difficulty. Sleep problems Bedtime Mcan make infants and young children moody, short tempered and unable to engage well in interactions with others. Sleep problems can also impact learning. When a young child is sleeping, her body is busy developing new and brain cells needed for her physical, mental and emotional development. Parents also need to feel rested in order to be nurturing and responsive to their growing and active young children. Here are a few proven tips for making Naptime bedtimes and naptimes easier for parents and children. Establish Good Tip: Sleep Habits Develop a regular time for going to bed and taking naps, and a regular time to wake up. Young children require about 10-12 hours of sleep a day (see the box on the last page that provides information on how much sleep a child needs). Sleep can be any combination of naps and night time sleep. Make sure your child has outside time and physical activity daily, but not within the hour before naptime or bedtime. Give your child your undivided and unrushed attention as you prepare her for bedtime or a nap. This will help to calm her and let her know how important this time is for you and her. Develop a bedtime and naptime routine. -
Clinical Characteristics of Primary Insomniacs with Sleep-State Misperception
JCN Open Access ORIGINAL ARTICLE pISSN 1738-6586 / eISSN 2005-5013 / J Clin Neurol 2015;11(4):358-363 / http://dx.doi.org/10.3988/jcn.2015.11.4.358 Clinical Characteristics of Primary Insomniacs with Sleep-State Misperception Hye-Jin Moona b Background and PurposezzThe aims of this study were to determine the prevalence of Mei Ling Song a sleep-state misperception and to identify any differences in the clinical characteristics of pri- Yong Won Cho mary insomniacs with and without misperception. a Department of Neurology and MethodszzIn total, 250 adult primary insomniacs were enrolled whose objective total sleep b Nursing Graduate School, time (TST) was more than 120 min, as assessed by full-night polysomnography. Sleep state Dongsan Medical Center, misperception was defined objectively as a TST of at least 6.5 h and an objective sleep effi- Keimyung University School of Medicine, Daegu, Korea ciency (SE) of at least 85%. ResultszzThe prevalence of sleep-state misperception in primary insomniacs was 26.4%. The (low) quality of sleep and psychiatric parameters were similar in the two groups, al- though the objective sleep architecture was relatively normal for the misperception group. Multivariate analysis revealed that both SE and sleep quality were significant factors associat- ed with subjective TST in the misperception group, while only SE was significant in those without misperception. Subjective TST was a significant effect factor with respect to sleep quality in the misperception group, while the Beck Depression Inventory-2 score and age were significant factors in those without misperception. ConclusionszzThe clinical characteristics of patients with sleep-state misperception differed from those without this condition. -

Simultaneous Stimulation of Slow-Wave Sleep and Growth Hormone Secretion by Gamma-Hydroxybutyrate in Normal Young Men
Simultaneous Stimulation of Slow-wave Sleep and Growth Hormone Secretion by Gamma-hydroxybutyrate in Normal Young Men Eve Van Cauter,* Laurence Plat,*§ Martin B. Scharf,‡ Rachel Leproult,* Sonya Cespedes,* Mireille L’Hermite-Balériaux,§ and Georges Copinschi§ *Department of Medicine, University of Chicago, Illinois 60637; ‡Center for Research in Sleep Disorders, Cincinnati, Ohio 45246; and §Center for the Study of Biological Rhythms (CERB), Laboratory of Experimental Medicine and Department of Endocrinology, Erasme Hospital, Université Libre de Bruxelles, B-1070 Brussels, Belgium Abstract first episode of slow-wave (SW) sleep (2, 3). A study with blood sampling at 30-s intervals has shown that maximal GH release The aim of this study was to investigate, in normal young occurs within minutes of the onset of SW sleep (4). Available ev- men, whether gamma-hydroxybutyrate (GHB), a reliable idence suggests that nocturnal GH secretion is controlled prima- stimulant of slow-wave (SW) sleep in normal subjects, would rily by growth hormone–releasing hormone (GHRH) release simultaneously enhance sleep related growth hormone (GH) (5). Because GH secretion is also under inhibitory control by so- secretion. Eight healthy young men participated each in matostastin, variability of somatostatinergic tone may underlie four experiments involving bedtime oral administration of dissociations between SW sleep and nocturnal GH release (6–9). placebo, 2.5, 3.0, and 3.5 g of GHB. Polygraphic sleep re- While such dissociations are observed frequently during late cordings were performed every night, and blood samples sleep, a large pulse of GH secretion occurs during the first SW were obtained at 15-min intervals from 2000 to 0800.