BASE HOSPITAL AIRWAY PROTOCOL INDEX Base Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Non-Invasive Ventilation Made Ridiculously Simple
NON-INVASIVE VENTILATION MADE RIDICULOUSLY SIMPLE Jennifer Newitt, MD 3rd year Pulmonary/Critical Care Fellow Mentor: Patrick Strollo Jr, MD Myth or Fact ?!? Myth or Fact ?!? Treatment for Obstructive Sleep Apnea ■ Lifestyle Modifications – Weight loss, increased fitness – Avoid alcohol, sleep deprivation, sedatives – Lateral position, head of bed elevation ■ Surgical – Upper airway reconstruction (UPP) or tracheostomy – Upper airway stimulation ■ Positive Airway Pressure via mask ■ Oral appliance therapy Treatment for Obstructive Sleep Apnea ■ Lifestyle Modifications – Weight loss, increased fitness – Avoid alcohol, sleep deprivation, sedatives – Lateral position, head of bed elevation ■ Surgical – Upper airway reconstruction (UPP) or trach – Upper airway stimulation ■Positive Positive Airway Pressure Airway via mask Pressure via mask ■ Oral appliance therapy 3 decades later…! Continuous Positive Airway Pressure (CPAP) ■ Continuous level of positive pressure provided to overcome airway obstruction ■ Patient must inhale and exhale over continuous pressure ■ Patient initiates all breaths ■ No additional pressure above level of CPAP is provided Continuous Positive Airway Pressure (CPAP) ■ Fixed CPAP – Fixed level of pressure between 4-20 cm H20 (ex: 10 cm H20) ■ Auto-CPAP – Variable pressure according to patient needs as detected by machine – If apnea, hypopnea, flow limitation, or snoring are detected, pressure is increased until events are eliminated – If no events are detected over set time period, pressure is decreased – Set pressure -

Sleep-Apnea-Protocol.Pdf
Evidence-based Practice Center Systematic Review Protocol Project Title: Continuous Positive Airway Pressure Treatment for Obstructive Sleep Apnea in Medicare Eligible Patients I. Background Sleep apnea is a common disorder that affects people of all ages. It is characterized by periods of airflow cessation (apnea) or reduced airflow (hypopnea) during sleep. Sleep apnea may be caused by mechanical obstruction of the airways resulting in disturbed airflow patterns, by a central loss of respiratory drive, or a combination of the two (mixed). Obstructive sleep apnea- hypopnea syndrome, more commonly called obstructive sleep apnea (OSA), is the most common type of sleep apnea.1 Definition and severity of obstructive sleep apnea Sleep apnea is primarily diagnosed with sleep tests that measure sleep time (and often other sleep measures) and respiratory events. OSA is distinguished from central sleep apnea by the presence of respiratory effort during episodes of apnea and hypopnea (in contrast with central sleep apnea where respiratory effort is lacking). The severity of OSA is typically quantified by the sum of the number of apneas and hypopneas per hour of sleep, a quantity that has been termed the apnea-hypopnea index (AHI). AHI is often used as part of both diagnosis (and, thus, study inclusion criteria) and as a surrogate measure for health outcomes (also called an intermediate outcome) in studies. The American Academy of Sleep Medicine (AASM) publishes scoring manuals for AHI and other physiological events to characterize OSA. In the United States, AASM is the predominant accrediting institution for sleep laboratories. AASM first published its scoring manual in 1999 (known as the “Chicago” Criteria).2 They have amended their definitions of breathing events, sleep time, and how these are measured multiple times since their first set of criteria, with major revisions in 2007,3 and in 2012.4 Minor revisions have been made almost annually since (the current version is v2.6,5 released in 2020). -

Role of the Allergist-Immunologist and Upper Airway Allergy in Sleep-Disordered Breathing
AAAAI Work Group Report Role of the Allergist-Immunologist and Upper Airway Allergy in Sleep-Disordered Breathing Dennis Shusterman, MD, MPHa, Fuad M. Baroody, MDb, Timothy Craig, DOc, Samuel Friedlander, MDd, Talal Nsouli, MDe, and Bernard Silverman, MD, MPHf; on behalf of the American Academy of Allergy, Asthma & Immunology’s Rhinitis, Rhinosinusitis and Ocular Allergy Committee Work Group on Rhinitis and Sleep-disordered Breathing San Francisco, Calif; Chicago, Ill; Hershey, Pa; Solon, Ohio; Washington, DC; and Brooklyn, NY BACKGROUND: Sleep-disordered breathing in general and RESULTS: Survey results were returned by 339 of 4881 active obstructive sleep apnea in particular are commonly encountered members (7%). More than two-third of respondents routinely conditions in allergy practice. Physiologically, nasal (or asked about sleep problems, believed that sleep-disordered nasopharyngeal) obstruction from rhinitis, nasal polyposis, or breathing was a problem for at least a “substantial minority” adenotonsillar hypertrophy are credible contributors to snoring (10%-30%) of their adult patients, and believed that medical and nocturnal respiratory obstructive events. Nevertheless, therapy for upper airway inflammatory conditions could existing practice parameters largely relegate the role of the potentially help ameliorate sleep-related complaints. Literature allergist to adjunctive treatment in cases of continuous positive review supported the connection between high-grade nasal airway pressure intolerance. congestion/adenotonsillar hypertrophy and obstructive sleep OBJECTIVES: To survey active American Academy of Allergy, apnea, and at least in the case of pediatric patients, supported the Asthma & Immunology members regarding their perceptions use of anti-inflammatory medication in the initial management and practices concerning sleep-disordered breathing in adult and of obstructive sleep apnea of mild-to-moderate severity. -

Policies & Procedures Title: CPAP/Bipap-Non Invasive Ventilation
Policies & Procedures Title: CPAP/BiPAP-Non Invasive Ventilation (NIV) - Care and Monitoring of the Patient • Post-operative care • Acute respiratory failure Number: 1114 Authorization: Source: Nursing Date Effective: January 2016 [X] SHR Nursing Practice Committee Scope: SHR Acute Urban Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. Overview The following policy applies only to the use of NIV for adult patients with acute respiratory failure (see appendix A, post-operative patients and dyspnea in palliative care patients. It does not apply to the treatment of sleep disordered breathing, chronic, stable respiratory failure or pediatric patients. Definitions: Non-Invasive Ventilation is the provision of ventilatory support through the patient’s upper airway using a mask or similar device. For the purposes of this policy, both continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP) will be generically referred to as non- invasive ventilation (NIV). Note: See SHR policy 7311-60-024 https://www.saskatoonhealthregion.ca/about/RWPolicies/7311-60- 024.pdf for the application of non-invasive ventilation for acute respiratory failure. Continuous Positive Airway Pressure (CPAP) is a continuous positive airway pressure that is used to provide a patent airway during periods of sleep apnea. -
Paramedic Airway Management Course
Pierce County EMS Paramedic Airway Course 2nd Edition September 2012 Pierce County EMS Paramedic Airway Management Course Table of Contents: Acknowledgements ............................................................................................ 3 Course Purpose and Description ..................................................................... 4 Background ........................................................................................................ 5 Assessing the Need for Emergency Airway Management ............................. 6 Effective Use of the Bag-Valve Mask ............................................................... 7 Endotracheal Intubation—Preparing for First Pass Success ........................ 8 RSI & Endotracheal Intubation ....................................................................... 11 Confirming, Securing and Monitoring Airway Placement ............................ 15 Use of Alternative “Rescue Airways” ............................................................ 16 Surgical Airways .............................................................................................. 17 Emergency Airway Management in Special Populations: ........................... 18 Pediatric Patients Geriatric Patients Trauma Patients Bariatric Patients Pregnant Patients Ten Tips for Best Practices in Emergency Airway Management ................ 21 Airway Performance Documentation and CQI Analysis ............................... 22 Conclusion ...................................................................................................... -

Effect of Continuous Positive Airway Pressure Versus Supplemental Oxygen on Sleep
1 Effect of Continuous Positive Airway Pressure versus Supplemental Oxygen on Sleep 2 Quality in Obstructive Sleep Apnea: A placebo-CPAP controlled study 3 4 5 José S. Loredo, MD,a Sonia Ancoli-Israel PhD,b Eui-Joong Kim, MD,c,b 6 Weon Jeong Lim, MD,d,b And Joel E. Dimsdale MDb 7 8 9 From the Department of Medicine,a and the Department of Psychiatry,b University of California, 10 San Diego, the Department of Psychiatry, Eulji University, Daejeon, Korea,c Department of 11 Psychiatry, Ewha Womans University, Seoul, Korea d 12 13 This work was performed at the University of California San Diego 14 15 This work was supported in part by NIH grants HL44915, AG08415, M01 RR00827, HL36005 16 and K23 HL04056 17 18 The authors did not receive any financial support from or were involved with organization(s) 19 with financial interest in the subject matter 20 21 Address correspondence and requests for reprints to Dr. José S. Loredo, UCSD Medical Center 22 Dept. of Medicine, 200 West Arbor Drive, San Diego, CA 92103-0804. 23 Phone: (619) 543-5593. Fax: (619) 543-7519. E-mail: [email protected] 1 24 ABSTRACT 25 Study Objectives: We investigated the short term effectiveness of CPAP and O2 in improving 26 sleep quality in patients with OSA. 27 Design: Randomized, double blinded, placebo-CPAP controlled, parallel study. 28 Setting: General Clinical Research Center at a University Hospital 29 Patients: Seventy-six untreated OSA patients 30 Interventions: Patients were randomized to one of three treatments (CPAP, placebo-CPAP, 31 nocturnal O2 at 3 L/min) for 2-weeks. -

The Effect of Continuous Positive Airway Pressures on Lung Volumes
Paraplegia (1996) 34, 54- 58 © 1996 International Medical Society of Paraplegia All rights reserved 0031-1758/96 $12.00 The effect of continuous positive airway pressures on lung volumes in tetraplegic patients 2 LA Harveyl and ER Ellis 2 1 Physiotherapy Department, The Prince Henry Hospital, Sydney; School of Physiotherapy, Faculty of Health Sciences, The University of Sydney, Sydney, Australia Continuous positive airway pressure (CPAP) is widely advocated for the treatment of respiratory complications. However the effects of CPAP on the respiratory function of tetraplegic patients have not yet been investigated. The purpose of this study was to examine the effects of breathing with different levels of CPAP on the relationship between closing volume (CV) and functional residual capacity (FRC) in ten recently injured, but otherwise healthy tetraplegic patients with lesions between the fourth and eighth cervical segments. Lung volumes were measured before, during and after 32 min of zero end-expiratory pressure and 5 and 10 cm H20 of CPAP. FRC was measured by the open-circuit nitrogen washout method and CV was measured by the single breath nitrogen washout method. FRC was unaffected by zero end-expiratory pressure, but both 5 cm H20 and 10 cm H20 of CPAP caused significant increases in FRC. FRC returned to pre-CPAP values by the first minute after removal of 5 and 10 cm H20 of CPAP. We were unable to measure CVs in any subjects. It was concluded that 5 and 10 cm H20 of CPAP increase FRC in healthy tetraplegic individuals, but that these increases are rapidly lost with the subsequent removal of CPAP. -

Practice Parameters for the Use of Continuous and Bilevel Positive
PRACTICE PARAMETER Practice Parameters for the Use of Continuous and Bilevel Positive Airway Pressure Devices to Treat Adult Patients With Sleep-Related Breathing Disorders An American Academy of Sleep Medicine Report Clete A. Kushida, MD, PhD1; Michael R. Littner, MD2; Max Hirshkowitz, PhD3; Timothy I. Morgenthaler, MD4; Cathy A. Alessi, MD5; Dennis Bailey, DDS6; Brian Boehlecke, MD, MSPH7; Terry M. Brown, DO8; Jack Coleman, Jr., MD9; Leah Friedman, PhD10; Sheldon Kapen, MD11; Vishesh K. Kapur, MD, MPH12; Milton Kramer, MD13; Teofilo Lee-Chiong, MD14; Judith Owens, MD15; Jeffrey P. Pancer, DDS16; Todd J. Swick, MD17; Merrill S. Wise, MD18 1Stanford University Center of Excellence for Sleep Disorders, Stanford, CA; 2VA Greater Los Angeles Healthcare System and David Geffen School of Medicine at UCLA, Sepulveda, CA; 3Baylor College of Medicine and VA Medical Center, Houston, TX; 4Mayo Sleep Disorders Center, Mayo Clinic, Rochester, MN; 5UCLA/Greater Los Angeles Healthcare System, Sepulveda, CA; 6Englewood, Colorado; 7University of North Carolina, Chapel Hill, NC; 8St. Joseph Memorial Hospital, Murphysboro, IL; 9Middle Tennessee ENT, Murfreesboro, TN; 10Stanford University School of Medicine, Stan- ford, CA; 11VA Medical Center and Wayne State University, Detroit, MI; 12University of Washington Sleep Disorder Center, Seattle, WA; 13Maimoides Medical Center, Psychiatry Department, Brooklyn, NY and New York University School of Medicine, New York, NY; 14National Jewish Medical and Research Center, Sleep Clinic, Denver, CO; 15Department of Pediatrics, Rhode Island Hospital, Providence, RI; 16Toronto, Ontario, CN; 17Houston, TX; 18Houston, TX Summary: Positive airway pressure (PAP) devices are used to treat pa- studies are usually adequate. 4) CPAP usage should be monitored objec- tients with sleep related breathing disorders (SRBD) including obstructive tively to help assure utilization. -

1. Ventilator Management
1. Ventilator Management Indications for Mechanical Ventilation Apnea Ventilatory insufficiency Increase in PaCo2 and decrease in ph Refractory hypoxemia Complications Associated with Mechanical Ventilation Hypotension Increased intrathoracic pressure decreases venous return to the heart Increased risk of ventilator associated pneumonia (VAP) Keep HOB at > 30 Maintain frequent, good oral care Problems with endotracheal tube Mucous plugging Tube my become dislodged Kinking or biting of tube Cuff rupture Pneumothorax Initial Ventilator Settings—parameters to be clarified Type of ventilation Mode of ventilation Tidal volume or peak inspiratory setting Respiratory rate FiO2 PEEP (Positive End Expiratory Pressure) Types of Ventilation Volume Cycled Ventilation(VCV) A pre-selected tidal volume is delivered at the pressure required. Tidal volume guaranteed. Peak inspiratory pressure will vary depending on airway resistance and lung compliance. Pressure Control Time-Cycled Ventilation (PCV) Operator selects inspiratory pressure and inspiratory time Breath is terminated when inspiratory time is reached Inspiratory pressure is guaranteed; tidal volume is dependant on airway resistance and lung compliance Pressure Support (PSV) Requires intact respiratory drive Operator selects inspiratory pressure Patient initiates breath, pressure quickly rises to set pressure and is maintained throughout the inspiratory phase Tidal volume determined by lung compliance and inspiratory effort Modes of Ventilation Assist/Control -

Removal of the Endotracheal Tube (2007)
AARC GUIDELINE: REMOVAL OF THE ENDOTRACHEAL TUBE AARC Clinical Practice Guideline Removal of the Endotracheal Tube—2007 Revision & Update RET 1.0 PROCEDURE RET 3.0 ENVIRONMENT Elective removal of the endotracheal tube from The endotracheal tube should be removed in an en- adult, pediatric, and neonatal patients. vironment in which the patient can be physiologi- cally monitored and in which emergency equipment RET 2.0 DESCRIPTION/DEFINITION and appropriately trained health care providers with The decision to discontinue mechanical ventilation airway management skills are immediately avail- involves weighing the risks of prolonged mechani- able (see RET 10.0 and 11.0). cal ventilation against the possibility of extubation failure.1,2 This guideline will focus on the predictors RET 4.0 INDICATIONS/OBJECTIVES that aid the decision to extubate, the procedure re- When the airway control afforded by the endotra- ferred to as extubation, and the immediate postextu- cheal tube is deemed to be no longer necessary for bation interventions that may avoid potential rein- the continued care of the patient, the tube should be tubation. This review will not address weaning removed. Subjective or objective determination of from mechanical ventilation, accidental extubation, improvement of the underlying condition impairing nor terminal extubation. pulmonary function and/or gas exchange capacity is made prior to extubation.2 To maximize the like- 2.1 The risks of prolonged translaryngeal intu- lihood for successful extubation, the patient should bation include but are not limited to: be capable of maintaining a patent airway and gen- 2.1.1 Sinusitis3,4 erating adequate spontaneous ventilation. -

Mechanical Ventilation
Fundamentals of MMeecchhaanniiccaall VVeennttiillaattiioonn A short course on the theory and application of mechanical ventilators Robert L. Chatburn, BS, RRT-NPS, FAARC Director Respiratory Care Department University Hospitals of Cleveland Associate Professor Department of Pediatrics Case Western Reserve University Cleveland, Ohio Mandu Press Ltd. Cleveland Heights, Ohio Published by: Mandu Press Ltd. PO Box 18284 Cleveland Heights, OH 44118-0284 All rights reserved. This book, or any parts thereof, may not be used or reproduced by any means, electronic or mechanical, including photocopying, recording or by any information storage and retrieval system, without written permission from the publisher, except for the inclusion of brief quotations in a review. First Edition Copyright 2003 by Robert L. Chatburn Library of Congress Control Number: 2003103281 ISBN, printed edition: 0-9729438-2-X ISBN, PDF edition: 0-9729438-3-8 First printing: 2003 Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the author and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, express or implied, with respect to the contents of the publication. Table of Contents 1. INTRODUCTION TO VENTILATION..............................1 Self Assessment Questions.......................................................... 4 Definitions................................................................................ -
EMS Patient Care Procedure Documents for NC EMS Systems
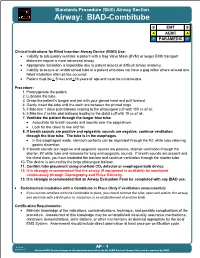
Standards Procedure (Skill) Airway Section Airway: BIAD-Combitube B EMT B A AEMT A P PARAMEDIC P Clinical Indications for Blind Insertion Airway Device (BIAD) Use: Inability to adequately ventilate a patient with a Bag Valve Mask (BVM) or longer EMS transport distances require a more advanced airway. Appropriate intubation is impossible due to patient access or difficult airway anatomy. Inability to secure an endotracheal tube in a patient who does not have a gag reflex where at least one failed intubation attempt has occurred. Patient must be > 5 feet and >16 years of age and must be unconscious. Procedure: 1. Preoxygenate the patient. 2. Lubricate the tube. 3. Grasp the patient s tongue and jaw with your gloved hand and pull forward. 4. Gently insert the tube until the teeth are between the printed rings. 5. Inflate line 1 (blue pilot balloon) leading to the pharyngeal cuff with 100 cc of air. 6. Inflate line 2 (white pilot balloon) leading to the distal cuff with 15 cc of air. 7. Ventilate the patient through the longer blue tube. Auscultate for breath sounds and sounds over the epigastrium. Look for the chest to rise and fall. 8. If breath sounds are positive and epigastric sounds are negative, continue ventilation through the blue tube. The tube is in the esophagus. In the esophageal mode, stomach contents can be aspirated through the #2, white tube relieving gastric distention. 9. If breath sounds are negative and epigastric sounds are positive, attempt ventilation through the shorter, #2 white tube and reassess for lung and epigastric sounds.