Chapter-1 District Reporting System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Achham, Banke, Chitwan, and Pachthar Districts
Technical Assistance Consultant’s Report Project Number: 44168-012 Capacity Development Technical Assistance (CDTA) October 2013 Nepal: Mainstreaming Climate Change Risk Management in Development (Financed by the Strategic Climate Fund) District Baseline Reports: Department of Roads (DOR) Achham, Banke, Chitwan, and Pachthar Districts Prepared by ICEM – International Centre for Environmental Management This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. (For project preparatory technical assistance: All the views expressed herein may not be incorporated into the proposed project’s design. MOSTE | Mainstreaming climate change risk management in development | DoR District Baseline TA – 7984 NEP October, 2013 Mainstreaming Climate Change Risk Management in Development 1 Main Consultancy Package (44768-012) ACHHAM DISTRICT BASELINE: DEPARTMENT OF ROADS (DOR) Prepared by ICEM – International Centre for Environmental Management METCON Consultants APTEC Consulting Prepared for Ministry of Science, Technology and Environment, Government of Nepal Environment Natural Resources and Agriculture Department, South Asia Department, Asian Development Bank Version B i MOSTE | Mainstreaming climate change risk management in development | DoR District Baseline TABLE OF CONTENTS 1 ACHHAM DISTRICT ........................................................................................................... 1 1.1 District Sector Master Plan ............................................................................................ -

Achhame, Banke, Chitwan, Kathmandu, and Panchthar Districts
Technical Assistance Consultant’s Report Project Number: 44168-012 Capacity Development Technical Assistance (CDTA) October 2013 Nepal: Mainstreaming Climate Change Risk Management in Development (Financed by the Strategic Climate Fund) District Baseline Reports: Department of Local Infrastructure Development and Agricultural Roads (DOLIDAR) Achhame, Banke, Chitwan, Kathmandu, and Panchthar Districts Prepared by ICEM – International Centre for Environmental Management This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. (For project preparatory technical assistance: All the views expressed herein may not be incorporated into the proposed project’s design. MOSTE | Mainstreaming climate change risk management in development | DoLIDAR District Baseline TA – 7984 NEP October, 2013 Mainstreaming Climate Change Risk Management in Development 1 Main Consultancy Package (44768-012) ACHHAM DISTRICT BASELINE: DEPARTMENT OF LOCAL INFRASTRUCTURE DEVELOPMENT & AGRICULTURAL ROADS (DOLIDAR) Prepared by ICEM – International Centre for Environmental Management METCON Consultants APTEC Consulting Prepared for Ministry of Science, Technology and Environment, Government of Nepal Environment Natural Resources and Agriculture Department, South Asia Department, Asian Development Bank Version B 1 MOSTE | Mainstreaming climate change risk management in development | DoLIDAR District Baseline TABLE OF CONTENTS 1 ACHHAM DISTRICT .......................................................................................................... -

Study Report on "Comminity Based Organizations(Cbos): Landscape
Community Based Organizations (CBOs): Landscape, Capacity Assessment and Strengthening Strategy Study Report Prepared for PLAN Nepal Lalitpur, Nepal July, 2005 Democratizing civil society at grassroots SAGUN P.O. Box 7802, Kathmandu, Nepal Phone: 977 4247920, Fax: 9771 4229544 Email: [email protected] Community Based Organizations (CBOs): Landscape, Capacity Assessment and Strengthening Strategy Mukta S. Lama Suresh Dhakal Lagan Rai Study Report Prepared for PLAN Nepal Lalitpur, Nepal July, 2005 SAGUN P.O. Box 7802, Kathmandu, Nepal Phone: 977 4247920, Fax: 9771 4229544 Email: [email protected] ii Acknowledgements This report is a result of contribution of many people in multiple ways. Foremost, we extend our deepest and heartfelt gratitude to members of Community Based Organizations across the districts for sharing us with their time, insight and experiences. The study benefited greatly from support and cooperation of the Plan field staff and partner agencies in Sunsari, Morang, Makwanpur, Rautahat, Bara, and Banke districts and the Regional Operational Support Unit teams. We would like to thank Ms. Chhing Lamu Sherpa, Mr. Kalbhan Rai, Dr. Chandra K. Sen, Mr. R. P. Gupta and Krishna Ghimire for their valuable inputs on the study. Dr. Chandi Chapagai, Plan Nepal Country Training Coordinator deserves special thanks for coordinating the whole exercise. We would like to express our deep appreciation to Shobhakar Vaidhya for his keen interest, insightful comments and his enthusiasm for incorporating the learning into the institutional policies and procedures. Thanks are also due to the Ms. Minty Pande, Country Director for her encouragement and comments. Similarly we very much appreciate the support of Mr. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -
Nepal's 9 Minimum Characteristics of a Disaster Resilient Community
Flagship 4 Handbook Nepal’s 9 Minimum Characteristics of a Disaster Resilient Community Published July 2013 Flagship 4: Integrated Community Based Disaster Risk Reduction/Management Flagship 4 is led by Government of Nepal’s Ministry of Federal Affairs and Local Development in partnership with the International Federation of Red Cross and Red Crescent Societies Flagship 4 is part of the Nepal Risk Reduction Consortium. An electronic version of this handbook can be downloaded from www.flagship4.nrrc.org.np The handbook is available in both English and Nepali Copies of the handbook and other documents can be obtained from IFRC’s Flagship 4 coordinator i Nepal’s 9 Minimum Characteristics Nepal’s 9 Minimum Characteristics of a Disaster Resilient Community of a Disaster Resilient Community About This Handbook Glossary of Terms Community Based Disaster Risk Reduction / Management Since the inception of the 9 minimum Handbook contents CBDRR/M characteristics of a disaster resilient community CDMC Community Disaster Management Committee in Nepal, there have been many questions Case studies by Government, implementing agencies, One attempt to provide guidance on DDC District Development Committee researchers, and community members on how operationalising the characteristics has DDMC District Disaster Management Committee to operationalise these characteristics. These been to collect a number of case studies questions have led to the formation of this from implementing agencies in Nepal. DDRC District Disaster Response Committee handbook which contains more information Each case study corresponds to a specific DEECC District Energy, Environment and Climate Change Division about each characteristic and examples of how characteristic and outlines how the they can be applied in interventions. -

Ltzt Ul/Alsf Uxgtf -K|Ltzt Affs Nifd0fk'/, G/}Gfk'/, S7s'oof, Sfnfkmf6f
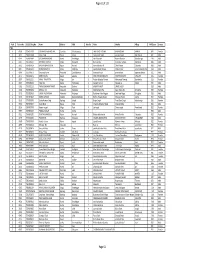
1 2 lhNnfx?sf] ul/aLsf] b/, ul/aLsf] ljifdtf / ul/aLsf] uxgtf @)^* lhNnf uf=lj=;=sf gfd ul/aLsf b/ ul/aLsf ljifdtf ul/aLsf uxgtf -k|ltzt_ -k|ltzt_ -k|ltzt_ afFs nIfd0fk'/, g/}gfk'/, s7s'Oof, sfnfkmf6f 56.46(10.17) 16.88(4.71) 6.8(2.36) afFs kmQ]k'/, lagf}gf 39.35(10.08) 9.88(3.57) 3.53(1.55) afFs d6]lxof, u+ufk'/ 57.98(9.77) 17.65(4.76) 7.2(2.47) afFs a}hfk'/, vf;s'Zdf 33.01(9.93) 7.52(3.07) 2.49(1.22) afFs sGrgk'/ 25.26(8.58) 5.33(2.37) 1.67(0.88) afFs dxfb]jk'/L 18.17(7.47) 3.62(1.9) 1.1(0.67) afFs sf]xnk'/ 12.48(4.8) 2.59(1.25) 0.81(0.45) afFs /em]gf 10.56(4.91) 2.02(1.17) 0.59(0.4) afFs zD;]/u~h 28.96(8.92) 6.92(2.92) 2.4(1.23) afFs u+ufk'/ 41.53(10.17) 10.8(3.7) 3.96(1.64) afFs sDbL 37.03(9.74) 9.65(3.48) 3.57(1.54) afFs dlgsfk'/ 21.98(6.69) 5.21(2.09) 1.8(0.86) afFs ags66L 47.84(9.58) 13.46(4.05) 5.2(1.94) afFs a]txgL 58.1(10.14) 17.37(4.79) 6.98(2.42) afFs xf]lnof 66.99(9.02) 22.33(5.27) 9.66(2.96) afFs k'/}gL, pbok'/ k'/}gf 40.52(9.93) 10.57(3.7) 3.88(1.66) afFs a;'b]jk'/ 23.52(7.13) 5.36(2.11) 1.79(0.83) afFs vf;sf/sf+bf] 9.42(3.62) 1.97(0.96) 0.62(0.35) afFs lkk/xjf, ejfgLk'/ 34.43(9.16) 8.42(3.11) 2.96(1.32) afFs lxl/ldlgof 42.28(10.72) 10.85(3.92) 3.93(1.73) afFs ags6jf 19.47(7.35) 4.12(2.01) 1.31(0.76) afFs lr;fkfgL 18.44(6.32) 3.93(1.72) 1.26(0.65) afFs gf}j:tf 22.23(7.75) 4.8(2.18) 1.55(0.83) afFs l6l6lx/Lof 23.97(8.41) 5.15(2.4) 1.65(0.92) afFs /lgofk'/ 36.22(9.38) 9.01(3.39) 3.2(1.49) afFs l;tfk'/ 11.86(5.22) 2.34(1.28) 0.71(0.45) afFs ;f]gk'/ 36.36(9.79) 8.96(3.35) 3.16(1.43) afFs p9/fk'/ 37.83(10.01) 9.42(3.46) 3.35(1.48) afFs a]nef/, ;fOufpF 45.89(9.99) 12.47(4.01) 4.71(1.87) afFs k/;k'/ 27.7(8.75) 6.62(2.82) 2.3(1.18) afFs /fwfk'/ 5.57(3.21) 0.95(0.63) 0.26(0.2) afFs afu]Zj/L 8.67(3.98) 1.62(0.9) 0.47(0.3) afFs sh'/fv'b{, OGb|k'/, a]nx/L 34.1(8.42) 8.57(2.95) 3.08(1.28) afFs g]kfnu+h gu/kflnsf 9.65(3.35) 2.17(0.93) 0.73(0.36) gf]6 M sf]i7s -_ leq /x]sf] c+sn] ;DalGwt ;"rssf] e|dfz+ -k|ltzt_ nfO{ hgfpF5 . -

Strengthening the Role of Civil Society and Women in Democracy And
HARIYO BAN PROGRAM Monitoring and Evaluation Plan 25 November 2011 – 25 August 2016 (Cooperative Agreement No: AID-367-A-11-00003) Submitted to: UNITED STATES AGENCY FOR INTERNATIONAL DEVELOPMENT NEPAL MISSION Maharajgunj, Kathmandu, Nepal Submitted by: WWF in partnership with CARE, FECOFUN and NTNC P.O. Box 7660, Baluwatar, Kathmandu, Nepal First approved on April 18, 2013 Updated and approved on January 5, 2015 Updated and approved on July 31, 2015 Updated and approved on August 31, 2015 Updated and approved on January 19, 2016 January 19, 2016 Ms. Judy Oglethorpe Chief of Party, Hariyo Ban Program WWF Nepal Baluwatar, Kathmandu Subject: Approval for revised M&E Plan for the Hariyo Ban Program Reference: Cooperative Agreement # 367-A-11-00003 Dear Judy, This letter is in response to the updated Monitoring and Evaluation Plan (M&E Plan) for the Hariyo Program that you submitted to me on January 14, 2016. I would like to thank WWF and all consortium partners (CARE, NTNC, and FECOFUN) for submitting the updated M&E Plan. The revised M&E Plan is consistent with the approved Annual Work Plan and the Program Description of the Cooperative Agreement (CA). This updated M&E has added/revised/updated targets to systematically align additional earthquake recovery funding added into the award through 8th modification of Hariyo Ban award to WWF to address very unexpected and burning issues, primarily in four Hariyo Ban program districts (Gorkha, Dhading, Rasuwa and Nuwakot) and partly in other districts, due to recent earthquake and associated climatic/environmental challenges. This updated M&E Plan, including its added/revised/updated indicators and targets, will have very good programmatic meaning for the program’s overall performance monitoring process in the future. -

The Nepal Smallholder Irrigation Market Initiative (SIMI) WINROCK/IDE/CEAPRED/SAPPROS
Increasing Rural Income through Micro Irrigation & Market Integration The Nepal Smallholder Irrigation Market Initiative (SIMI) WINROCK/IDE/CEAPRED/SAPPROS USAID Cooperative Agreement No. 367-A-00-03-00116-00 Nepal SIMI Annual (Fourth Quarter) Performance Report 2005 July 1, 2004 – June 30, 2005 (F.Y. 2004/5) Nepal SIMI Performance Report No. 8 Mailing Address GPO 8975, EPC 2560, Bakhundol, Lalitpur Tel: (977-1) 5535565 Fax: 5520846 E-mail: [email protected] Table of Contents 1.0 Background…………………………………………………………………………..1 1.1 SIMI goals………………………………………………………………………...2 1.2 Partners…………………………………………………………………………...2 2.0 Expected Results (Output or Indicators)……...……………………………………3 3.0 SIMI Indicator Target Performance………..……………………………….……..3 3.1 Activities………………………………………………………………………..5 3.1.1 Program Mobilization…………………………………………………5 3.1.2 Supply Chain Development……………………………………………5 3.1.3 Social Marketing……………………………………………………….7 3.1.4 Market Development…………………………………………………..7 3.1.5 Collaborative Partnerships and Linkages with Government……….8 3.1.6 Water Source Development…………………………………………...8 3.1.7 Gender Program……………………………………………………….8 3.1.8 Monitoring and Evaluation……………………………………………9 3.1.9 Success Stories………………………………………………………...10 3.1.10 Component wise Highlighted Program……………………………...18 3.2 Activities Planned for the Next Three Months……………………………...30 4.0 Statement of Work………………………………………………………………….31 5.0 Administrative Information………………………………………………………..31 6.0 Financial Information………………………………………………………………33 Annex A Nepal SIMI Project Areas…………………………………………………...34 -
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -
Annual Report Submitted to USAID So the Details of Those Activities Are Not Reported Here
From Combatants to Peacemakers Program Project Final Report October, 2015 to March 31, 2017 Award No: AID-367-F-15-00002 Under USAID/DCHA/CMM APS-OAA-14-000003 Submitted to: United States Agency for International Development (USAID) Democracy and Governance Office Maharajgunj, Kathmandu, Nepal Tel: +977-01-42340000 Submitted by: Forum for Protection of Public Interest (Pro Public) Gautambuddha Marg, Anamnagar P.O.Box: 14307 Telephone: +977-01-4268681, 4265023 Fax: +977-01-4268022 1 Disclaimer: All these activities were made possible by the generous support of the American people through the United States Agency for International Development (USAID). The contents are the responsibility of Pro Public and do not necessarily reflect the views of USAID or the United States Government. 2 Abbreviations BC Brahmin Chhetri CBO Community Based Organization CDO Chief District Officer CPN Communist Party of Nepal CSO Civil Society Organization DDC District Development Committee DF Dialogue facilitation ECs Ex-Combatants FGD Focus Group Discussion GESI Gender and Social Inclusion GIZ Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) GmbH KII Key Informant Interview LPC Local Peace Committee NC Nepali Congress NPTF Nepal Peace Trust Fund OCA Organizational Capacity Assessment OPI Organizational Performance Index PLA People Liberation Army Pro Public Forum for the Protection of Public Interest SDG Social Dialogue Group STPP Strengthening the Peace Process UCPN United Communist Party of Nepal UML United Marxist Leninist UNDP United Nations Development Program USAID United States Agency for International Development VDC Village Development Committee WCF Ward Citizen Forum 3 Acknowledgement This project completion report covers the overall implementation of the USAID-funded Combatants to Peacemakers (C2P) project (October 2015 to March 2017). -
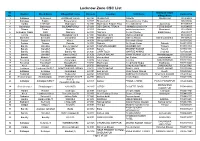
Lucknow Zone CSC List.Xlsx
Lucknow Zone CSC List Sl. Grampanchayat District Block Name Village/CSC name Pincode Location VLE Name Contact No No. Village Name 1 Sultanpur Sultanpur4 JAISINGHPUR(R) 228125 ISHAQPUR DINESH ISHAQPUR 730906408 2 Sultanpur Baldirai Bhawanighar 227815 Bhawanighar Sarvesh Kumar Yadav 896097886 3 Hardoi HARDOI1 Madhoganj 241301 Madhoganj Bilgram Road Devendra Singh Jujuvamau 912559307 4 Balrampur Balrampur BALRAMPUR(U) 271201 DEVI DAYAL TIRAHA HIMANSHU MISHRA TERHI BAZAR 912594555 5 Sitapur Sitapur Hargaon 261121 Hargaon ashok kumar singh Mumtazpur 919283496 6 Ambedkar Nagar Bhiti Naghara 224141 Naghara Gunjan Pandey Balal Paikauli 979214477 7 Gonda Nawabganj Nawabganj gird 271303 Nawabganj gird Mahmood ahmad 983850691 8 Shravasti Shravasti Jamunaha 271803 MaharooMurtiha Nafees Ahmad MaharooMurtiha 991941625 9 Badaun Budaun2 Kisrua 243601 Village KISRUA Shailendra Singh 5835005612 10 Badaun Gunnor Babrala 243751 Babrala Ajit Singh Yadav Babrala 5836237097 11 Bareilly Bareilly2 Bareilly Npp(U) 243201 TALPURA BAHERI JASVEER GIR Talpura 7037003700 12 Bareilly Bareilly3 Kyara(R) 243001 Kareilly BRIJESH KUMAR Kareilly 7037081113 13 Bareilly Bareilly5 Bareilly Nn 243003 CHIPI TOLA MAHFUZ AHMAD Chipi tola 7037260356 14 Bareilly Bareilly1 Bareilly Nn(U) 243006 DURGA NAGAR VINAY KUMAR GUPTA Nawada jogiyan 7037769541 15 Badaun Budaun1 shahavajpur 243638 shahavajpur Jay Kishan shahavajpur 7037970292 16 Faizabad Faizabad5 Askaranpur 224204 Askaranpur Kanchan ASKARANPUR 7052115061 17 Faizabad Faizabad2 Mosodha(R) 224201 Madhavpur Deepchand Gupta Madhavpur -

POPULATION STATUS and HABITAT SUITABILITY of SARUS CRANE (Antigone Antigone, Linnaeus, 1758) in BANKE DISTRICT, NEPAL
POPULATION STATUS AND HABITAT SUITABILITY OF SARUS CRANE (Antigone antigone, Linnaeus, 1758) IN BANKE DISTRICT, NEPAL SHRADDHA TIWARI T.U. Registration No. 5-1-33-471-2005 T.U. Examination Roll No: 050 Batch: 2070/2071 A thesis submitted in partial fulfillment of the requirements for the award of the degree of Master of Science in Zoology with special paper Ecology and Environment. Submitted to Central Department of Zoology Institute of Science and Technology Tribhuvan University Kirtipur, Kathmandu Nepal December, 2016 DECLARATION I hereby declare that the work presented in this thesis has been done by myself, and has not been submitted elsewhere for the award of any degree. All sources of information have been specifically acknowledged by references to the author(s) or institution(s). ……………………… Date: ................................. Ms. Shraddha Tiwari i TRIBHUVAN UNIVERSITY CENTRAL DEPARTMENT OF ZOOLOGY Kirtipur, Kathmandu, Nepal RECOMMENDATION This is to recommend that the thesis entitled “POPULATION STATUS AND HABITAT SUITABILITY OF SARUS CRANE (Antigone antigone, Linnaeus 1758) IN BANKE DISTRICT, NEPAL” has been carried out by Ms. Shraddha Tiwari for the partial fulfillment of Master’s Degree of Science in Zoology with special paper Ecology and Environment. This is her original work and has been carried out under my supervision. To the best of our knowledge, this thesis work has not been submitted for any other degree in any institutions. Date:-………………………………. ………………………………….. Supervisor Nanda Bahadur Singh, PhD Professor Central Department of Zoology Tribhuvan University ii TRIBHUVAN UNIVERSITY CENTRAL DEPARTMENT OF ZOOLOGY Kirtipur, Kathmandu, Nepal RECOMMENDATION This is to recommend that the thesis entitled “POPULATION STATUS AND HABITAT SUITABILITY OF SARUS CRANE (Antigone antigone, Linnaeus 1758) IN BANKE DISTRICT, NEPAL” has been carried out by Ms.