Kava Hepatotoxicity: Comparative Study of Two Structured Quantitative Methods for Causality Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Central Valley Toxicology Drug List
Chloroform ~F~ Lithium ~A~ Chlorpheniramine Loratadine Famotidine Acebutolol Chlorpromazine Lorazepam Fenoprofen Acetaminophen Cimetidine Loxapine Fentanyl Acetone Citalopram LSD (Lysergide) Fexofenadine 6-mono- Clomipramine acetylmorphine Flecainide ~M~ Clonazepam a-Hydroxyalprazolam Fluconazole Maprotiline Clonidine a-Hydroxytriazolam Flunitrazepam MDA Clorazepate Albuterol Fluoxetine MDMA Clozapine Alprazolam Fluphenazine Medazepam Cocaethylene Amantadine Flurazepam Meperidine Cocaine 7-Aminoflunitrazepam Fluvoxamine Mephobarbital Codeine Amiodarone Fosinopril Meprobamate Conine Amitriptyline Furosemide Mesoridazine Cotinine Amlodipine Methadone Cyanide ~G~ Amobarbital Methanol Cyclobenzaprine Gabapentin Amoxapine d-Methamphetamine Cyclosporine GHB d-Amphetamine l-Methamphetamine Glutethamide l-Amphetamine ~D~ Methapyrilene Guaifenesin Aprobarbital Demoxepam Methaqualone Atenolol Desalkylfurazepam ~H~ Methocarbamol Atropine Desipramine Halazepam Methylphenidate ~B~ Desmethyldoxepin Haloperidol Methyprylon Dextromethoraphan Heroin Metoclopramide Baclofen Diazepam Hexobarbital Metoprolol Barbital Digoxin Hydrocodone Mexiletine Benzoylecgonine Dihydrocodein Hydromorphone Midazolam Benzphetamine Dihydrokevain Hydroxychloroquine Mirtazapine Benztropine Diltiazem Hydroxyzine Morphine (Total/Free) Brodificoum Dimenhydrinate Bromazepam ~N~ Diphenhydramine ~I~ Bupivacaine Nafcillin Disopyramide Ibuprofen Buprenorphine Naloxone Doxapram Imipramine Bupropion Naltrexone Doxazosin Indomethacin Buspirone NAPA Doxepin Isoniazid Butabarbital Naproxen -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -
Kava - the Unfolding Story: Report on a Work-In-Progress
Article Kava - the unfolding story: Report on a work-in-progress. Denham, Alison, McIntyre, Michael and Whitehouse, Jule Available at http://clok.uclan.ac.uk/9455/ Denham, Alison, McIntyre, Michael and Whitehouse, Jule Kava - the unfolding story: Report on a work-in-progress. Journal of Alternative and Complementary Medicine, 8 (3). pp. 237-263. It is advisable to refer to the publisher’s version if you intend to cite from the work. For more information about UCLan’s research in this area go to http://www.uclan.ac.uk/researchgroups/ and search for <name of research Group>. For information about Research generally at UCLan please go to http://www.uclan.ac.uk/research/ All outputs in CLoK are protected by Intellectual Property Rights law, including Copyright law. Copyright, IPR and Moral Rights for the works on this site are retained by the individual authors and/or other copyright owners. Terms and conditions for use of this material are defined in the policies page. CLoK Central Lancashire online Knowledge www.clok.uclan.ac.uk THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE Volume 8, Number 3, 2002, pp. 237–263 © Mary Ann Liebert, Inc. SPECIAL REPORT Kava—the Unfolding Story: Report on a Work-in-Progress ALISON DENHAM, B.A. (Soc.), M.N.I.M.H., 1 MICHAEL McINTYRE, M.A., F.N.I.M.H., F.R.C.H.M., M.B.Ac.C., 2 and JULIE WHITEHOUSE, Ph.D., M.N.I.M.H. 3 ABSTRACT This paper, originated as a submission (now updated) to the U.K. Medicines Control Agency and Committee of Safety of Medicines (CSM) on January 11, 2002, in response to a report circu- lated by the German Federal Institute for Drugs and Medical Products (German initials are BfArM), a compilation of which is summarized in Appendix 2. -

Letters to the Editor
Letters to the Editor Internet Pharmacy Prescription complete the medication database. Of course, patients can abuse and Phentermine Overdose any medications, so collaboration between pharmacies and physicians is essential to minimize this risk. Sir: The Internet is now widely used by patients for both Dr. Takeshita reports no financial or other relationship relevant to the health information and prescription services. Yet, a MEDLINE subject matter of this letter. search in January 2002 using the phrase “Internet pharmacy” showed a total of 99 articles; nearly all were geared toward REFERENCES health care management or the general public. There are only a few published reports of bad outcome resulting from medical 1 1. Crocco AG, Villasis-Keever M, Jadad AR. Analysis of cases of information obtained from the Internet. The U.S. Food and harm associated with use of health information on the Internet. Drug Administration noted 326 Internet sites selling pharma- JAMA 2002;287:2867–2871 ceutical products.2 The exact numbers are difficult to quantify 2. Henney JE. Cyberpharmacies and the role of the US Food and Drug as Web sites are constantly changing. I report a case of overdose Administration. J Med Internet Res 2001;3:E3 with phentermine that was obtained through an Internet 3. Gardin JM, Schumacher D, Constantine G, et al. Valvular abnormali- pharmacy. ties and cardiovascular status following exposure to dexfenfluramine or phentermine/fenfluramine. JAMA 2000;283:1703–1709 4. Koury E, Stone CK, Stapczynski JS, et al. Sympathetic overactivity Case report. Ms. A, a 20-year-old woman with a prior from fenfluramine-phentermine overdose. -
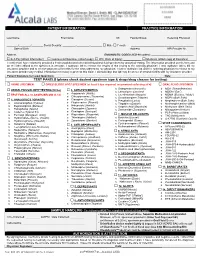
Please Check Desired Specimen Type & Drugs/Drug Classes for Testing
PATIENT INFORMATION PRACTICE INFORMATION ____________________________________ _____________________________________ _______ ________________________ __________________ Last Name First Name MI Facility/Group Referring Physician ________/________/________ Social Security: _________-_________-________ ☐ Male ☐ Female ___________________________________________ Date of Birth Address NPI Provider Nr. __________________________________________________________________ Address DIAGNOSTIC CODES (ICD-10 codes): _____________________________ ☐ Self-Pay (attach Information) ☐ Commercial Insurance (attach copy) ☐ W/C (Date of Injury): ____________ ☐ Medicare (attach copy of Insurance) I certify that I have voluntarily provided a fresh unadulterated urine/dried blood/oral fluid specimen for analytical testing. The information provided on this form and on the label affixed to the specimen is accurate. I authorize lab to release the results of this testing to the ordering physician. I also authorize lab to bill my insurance provider and to receive payment of benefits for the tests ordered by my physician. I further authorize lab and the ordering physician to release to my insurance provider any medical information necessary to process this claim. I acknowledge that lab may be an out-of-network facility with my insurance provider. Patient Signature (or Legal Guardian): ___________________________________________________________________________ Date: _______________ TEST PANELS (please check desired specimen type & drugs/drug classes for testing): ☐ URINE -

Kava Kava Extract Is Available from Ashland Chemical Co., Mini Star International, Inc., and QBI (Quality Botanical Ingredients, Inc.)
SUMMARY OF DATA FOR CHEMICAL SELECTION Kava Kava 9000-38-8; 84696-40-2 November 1998 TABLE OF CONTENTS Basis for Nomination Chemical Identification Production Information Use Pattern Human Exposure Regulatory Status Evidence for Possible Carcinogenic Activity Human Data Animal Data Metabolism Other Biological Effects Structure-Activity Relationships References BASIS OF NOMINATION TO THE CSWG Kava kava is brought to the attention of the CSWG because it is a rapidly growing, highly used dietary supplement introduced into the mainstream U.S. market relatively recently. Through this use, millions of consumers using antianxiety preparations are potentially exposed to kava kava. A traditional beverage of various Pacific Basin countries, kava clearly has psychoactive properties. The effects of its long-term consumption have not been documented adequately; preliminary studies suggest possibly serious organ system effects. The potential carcinogenicity of kava and its principal constituents are unknown. INPUT FROM GOVERNMENT AGENCIES/INDUSTRY The U.S. Pharmacopeia is in the process of reviewing kava kava. No decision on preparation of a monograph has been made. SELECTION STATUS ACTION BY CSWG: 12/14/98 Studies requested: - Toxicological evaluation, to include studies of reproductive toxicity and neurotoxicity - Genotoxicity Priority: High Rationale/Remarks: - Significant human exposure - Leading dietary supplement with rapidly growing use - Concern that kava has been promoted as a substitute for ritilin in children - Test extract standardized to 30 percent kavalactones - NCI is conducting studies in Salmonella typhimurium CHEMICAL IDENTIFICATION CAS Registry Number: 9000-38-8 Kava-kava resin (8CI) Chemical Abstract Service Name: 84696-40-2 CAS Registry Number: Pepper (Piper), P. methysticum, ext. Chemical Abstract Service Name: Extract of kava; kava extract; Piper Synonyms and Trade Names: methisticum extract Description: The tropical shrub Piper methysticum is widely cultivated in the South Pacific. -

Kavain, the Major Constituent of the Anxiolytic Kava
RESEARCH ARTICLE Kavain, the Major Constituent of the Anxiolytic Kava Extract, Potentiates GABAA Receptors: Functional Characteristics and Molecular Mechanism Han Chow Chua1, Emilie T. H. Christensen1,2, Kirsten Hoestgaard-Jensen2, Leonny Y. Hartiadi1, Iqbal Ramzan1, Anders A. Jensen2, Nathan L. Absalom1, Mary Chebib1* 1 Faculty of Pharmacy, The University of Sydney, Sydney, New South Wales, Australia, 2 Department of a11111 Drug Design and Pharmacology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark * [email protected] Abstract OPEN ACCESS Extracts of the pepper plant kava (Piper methysticum) are effective in alleviating anxiety in Citation: Chua HC, Christensen ETH, Hoestgaard- Jensen K, Hartiadi LY, Ramzan I, Jensen AA, et al. clinical trials. Despite the long-standing therapeutic interest in kava, the molecular target(s) (2016) Kavain, the Major Constituent of the Anxiolytic of the pharmacologically active constituents, kavalactones have not been established. γ- Kava Extract, Potentiates GABAA Receptors: Aminobutyric acid type A receptors (GABAARs) are assumed to be the in vivo molecular tar- Functional Characteristics and Molecular Mechanism. PLoS ONE 11(6): e0157700. doi:10.1371/journal. get of kavalactones based on data from binding assays, but evidence in support of a direct pone.0157700 interaction between kavalactones and GABAARs is scarce and equivocal. In this study, we Editor: Steven Barnes, Dalhousie University, characterised the functional properties of the major anxiolytic kavalactone, kavain at human CANADA recombinant α1β2, β2γ2L, αxβ2γ2L (x = 1, 2, 3 and 5), α1βxγ2L (x = 1, 2 and 3) and α4β2δ Received: March 24, 2016 GABAARs expressed in Xenopus oocytes using the two-electrode voltage clamp technique. -

Analytical Studies on the Kavain Metabolism in Human Specimen and Liver Cell Lines
Analytical studies on the kavain metabolism in human specimen and liver cell lines Inaugural-Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakultät der Heinrich-Heine-Universität Düsseldorf Vorgelegt von Fuad Ali Tarbah aus Derna, Libyen Düsseldorf 2003 Gedruckt mit Genehmigung der Mathematisch-Naturwissenschaftlichen Fakultät der Heinrich-Heine-Universität Düsseldorf Referent: Prof. Dr. Th. Daldrup Korreferent: Prof. Dr. G. Willuhn, Prof. Dr. H. Weber Tag der mündlichen Prüfung: 17. 12. 2003 Parts of this Ph.D. Thesis have already been presented and/or published in: Tarbah F. A., Mahler H., Temme O. and Daldrup Th. Mass spectral characterisation of hepatic cell metabolites of D,L-kavain using HPLC and GC/MS systems. Special issue: 37th TIAFT triennial meeting “Problems of Forensic Sciences” XLII: 173-180 (1999) Tarbah F. A., Mahler H., Temme O. and Daldrup Th. Determination of D,L-kavain and its metabolites in blood, serum and urine. Rapid quantitative method using fluid/fluid extraction and gas chromatography/mass spectrometry (GC/MS). Poster in 79. Jahrestagung der Deutschen Gesellschaft für Rechtsmedizin, Medizinische Einrichtungen der Universität / Gesamthochschule Essen (2000) Tarbah F., Mahler H., Kardel B., Weinmann W., Hafner D. and Daldrup Th. Kinetics of kavain and its metabolites after oral application. J. Chromatogr. B 789 (1): 115-130 (2003) Cabalion P., Barguil Y., Duhet D., Mandeau A., Warter S., Russmann S., Tarbah F. and Daldrup Th. Kava in modern therapeutic uses: to a better evaluation -

5Mg/6Mg Tablets for Example Valsartan, Telmisartan, Irbesartan, Etc.), in Particular Ramipril 5Mg If You Have Diabetes-Related Kidney Problems, • Aliskiren
PACKAGE LEAFLET: INFORMATION FOR THE USER • If you are taking any of the following medicines used to treat high blood pressure: • an ’angiotensin II receptor blocker (ARBs) (also known as sartans - 5mg/6mg Tablets for example valsartan, telmisartan, irbesartan, etc.), in particular Ramipril 5mg if you have diabetes-related kidney problems, • aliskiren. Piretanide 6mg Your doctor may check your kidney function, blood pressure, and the amount of electrolytes (e.g. potassium) in your blood at regular intervals. See information under the heading ’Do not take Trialix Tablets’. • You have gout Is this leaflet hard to see or read? • You feel dizzy or dehydrated. This can happen if you have lost a Phone 01 403 5600 for help lot of body salts or fluids (through being sick (vomiting), having Read all of this leaflet carefully before you start using this diarrhoea, sweating more than usual, being on a low salt diet, medicine because it contains important information for you. passing water very often or having had dialysis. It can also happen • Keep this leaflet. You may need to read it again if you are having trouble drinking or eating • If you have any further questions, ask your doctor or pharmacist • If you have been pre-treated with diuretics (drugs to increase • This medicine has been prescribed for you only. Do not pass it the rate of urination) on to others. It may harm them, even if their signs of illness are • You are going to receive an anaesthetic. This may be given for an the same as yours. operation or any dental work. -

Piper Methysticum)
Journal of Student Research (2015) Volume 4, Issue 2: pp. 69-72 Research Article A Closer Look at the Risks vs. Benefits of Kava (Piper methysticum) Anan A. Husseina If you took a trip to Fiji, the locals would probably welcome you with a drink of Kava. For centuries, the indigenous people of the South Pacific Islands have used the roots of a plant known as Kava. Beyond the use of Kava as a psychoactive substance, it has been incorporated as a cultural drink that is used in many ceremonies. In the late 1990’s Kava use spread quickly in Western countries including Europe, North America, and Australia. It was used as a treatment for anxiety. But just as quickly as it spread, the enthusiasm for it faded, because it was banned or restricted in many Western countries following reports of liver toxicity. In the United States, the Food and Drug Administration’s (FDA) concern for safety prompted a request for more research on the substance. The issues of safety and efficacy remain more specifically whether the benefits of using Kava outweigh the risks. History Kava is a beverage made from the roots of the plant included alcohol, cocaine, tobacco, and heroin. The findings Piper methysticum, and has been used historically in the suggest that kava may reduce the craving associated with the South Pacific Islands as a ceremonial drink. Kava was aforementioned substances, which may make kava a great introduced in Europe around the 1700s by Captain James future candidate to help with addiction. 13 Cook and has since spread widely to Australia, Europe, and Although the mechanism of action is not clear, it is the United States. -

Toxic, and Comatose-Fatal Blood-Plasma Concentrations (Mg/L) in Man
Therapeutic (“normal”), toxic, and comatose-fatal blood-plasma concentrations (mg/L) in man Substance Blood-plasma concentration (mg/L) t½ (h) Ref. therapeutic (“normal”) toxic (from) comatose-fatal (from) Abacavir (ABC) 0.9-3.9308 appr. 1.5 [1,2] Acamprosate appr. 0.25-0.7231 1311 13-20232 [3], [4], [5] Acebutolol1 0.2-2 (0.5-1.26)1 15-20 3-11 [6], [7], [8] Acecainide see (N-Acetyl-) Procainamide Acecarbromal(um) 10-20 (sum) 25-30 Acemetacin see Indomet(h)acin Acenocoumarol 0.03-0.1197 0.1-0.15 3-11 [9], [3], [10], [11] Acetaldehyde 0-30 100-125 [10], [11] Acetaminophen see Paracetamol Acetazolamide (4-) 10-20267 25-30 2-6 (-13) [3], [12], [13], [14], [11] Acetohexamide 20-70 500 1.3 [15] Acetone (2-) 5-20 100-400; 20008 550 (6-)8-31 [11], [16], [17] Acetonitrile 0.77 32 [11] Acetyldigoxin 0.0005-0.00083 0.0025-0.003 0.005 40-70 [18], [19], [20], [21], [22], [23], [24], [25], [26], [27] 1 Substance Blood-plasma concentration (mg/L) t½ (h) Ref. therapeutic (“normal”) toxic (from) comatose-fatal (from) Acetylsalicylic acid (ASS, ASA) 20-2002 300-3502 (400-) 5002 3-202; 37 [28], [29], [30], [31], [32], [33], [34] Acitretin appr. 0.01-0.05112 2-46 [35], [36] Acrivastine -0.07 1-2 [8] Acyclovir 0.4-1.5203 2-583 [37], [3], [38], [39], [10] Adalimumab (TNF-antibody) appr. 5-9 146 [40] Adipiodone(-meglumine) 850-1200 0.5 [41] Äthanol see Ethanol -139 Agomelatine 0.007-0.3310 0.6311 1-2 [4] Ajmaline (0.1-) 0.53-2.21 (?) 5.58 1.3-1.6, 5-6 [3], [42] Albendazole 0.5-1.592 8-992 [43], [44], [45], [46] Albuterol see Salbutamol Alcuronium 0.3-3353 3.3±1.3 [47] Aldrin -0.0015 0.0035 50-1676 (as dieldrin) [11], [48] Alendronate (Alendronic acid) < 0.005322 -6 [49], [50], [51] Alfentanil 0.03-0.64 0.6-2.396 [52], [53], [54], [55] Alfuzosine 0.003-0.06 3-9 [8] 2 Substance Blood-plasma concentration (mg/L) t½ (h) Ref. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine