Hot Cereal Cathy Breedon
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
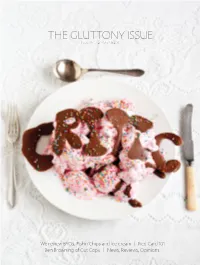
THE GLUTTONY ISSUE Issue 04 – 21St March 2011
THE GLUTTONY ISSUE Issue 04 – 21st March 2011 We review BYOs, Fish‘n’Chips and Ice cream | Red Card 101 Ben Browning of Cut Copy | News, Reviews, Opinions. Critic Issue 04 – 1 Critic Issue 04 – 2 Critic – Te Arohi PO Boc 1436, Dunedin (03) 479 5335 [email protected] www.critic.co.nz contents Editor: 5 – Editorial Julia Hollingsworth Designer: 6 – Letters to the Editor Andrew Jacombs Ad Designer: 7 – Notices Kathryn Gilbertson News Editor: 8 – Snippets Gregor Whyte News Reporters: 10 – News Aimee Gulliver, Lozz Holding 18 – The Inaugural BYO review Feature Writers: BYOs are becoming an integral part of student life. Charlotte Greenfield, We review the best and worst of the bunch. Josh Hercus, Phoebe Harrop, 21 – The Great and Glorious Annual Critic Siobhan Downes Sub Editor: Fush & Chup Review Lisa McGonigle Speaks for itself really. Feature Illustrator: Tom Garden 24 – We all scream for ice cream Music Editor: Critic reviews ice cream. Num num. Sam Valentine Film Editor: 26 – Red Card 101; an introduction to, and critical Sarah Baillie Books Editor: appraisal of, a Dunedin student tradition. Sarah Maessen We talk Red Cards: the themes, the crazy stuff that goes down, Theatre Editor: and what the Proctor thinks of them. Jen Aitken Food Editor: 30 – In Memoriam Niki Lomax Games Editor: 31 – Opinion Toby Hills Fashion Editor: 38 – Profile Mahoney Turnbull Critic interviews Ben Browning of Cut Copy Art Editor: Hana Aoake 40 – Summer Lovin’ And a whole heap of lovely volunteers 41 – Review Music, Film, Art, Fashion, Food, Games, Theatre, Books Planet Media (03) 479 5361 53 – Comics [email protected] www.planetmedia.co.nz 55 – OUSA Page Advertising: Kate Kidson, Tim Couch, Dave Eley, Critic is a member of the Aotearoa Student Press Association (ASPA). -

WO 2U11/154U12 a L
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Χ 15 December 2011 (15.12.2011) WO 2U11/154U12 A l (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/415 (2006.01) A61K 9/20 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (21) International Application Number: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, PCT/DK201 1/050207 DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 10 June 201 1 (10.06.201 1) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (26) Publication Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: PA 2010 00506 10 June 2010 (10.06.2010) DK Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): LIFE- GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, CYCLE PHARMA A S [DK/DK]; Kogle Alle 4, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, DK-2970 H0rsholm (DK). -

Principios Activos Fotosensibles
PRINCIPIOS ACTIVOS FOTOSENSIBLES PROTEGE A TUS PRODUCTOS DE LA FOTODEGRADACIÓN PRINCIPIOS ACTIVOS FOTOSENSIBLES Adenosine Carbamazepine Digitoxin Heptacaine Methaqualone-1-oxide Phenothiazines Sulfisomidine Tinidazole Vitamin D Adrenaline Carbisocaine Digoxin Hexachlorophane Methotrexate Phenylbutazone Sulpyrine Tolmetin Vitamin E Adriamycin Carboplatin Dihydroergotamin Hydralazine Metronidazole Phenylephrine Suprofen Tretinoin Vitamin K1 Amidopyrin Carmustine Dihydropyridines Mifepristone Phenytoin Triamcinolone Vitamin K2 Hydrochlorothiazide Suramin Amidinohydrazones Cefotaxime Diltiazem Hydrocortisone Minoxidil Physostigmine Triamterene Warfarin Amiloride Cefuroxime axetil Diosgenin Mitomycin C Piroxicam Tauromustine (TCNU) Trifluoperazine Hydroxychloroquine Terbutaline 4-Aminobenzoic acid Cephaeline Diphenhydramine Hypochloride Mitonafide Pralidoxime Trimethoprim Aminophenazone Cephalexine Dipyridamole Ibuprofen Mitoxantrone Prednisolone Tetracyclines Ubidecarenone Thiazide Aminophylline Cephradine Dithranol Imipramin Molsidomine Primaquine Vancomycin Thiocolchicoside Aminosalicylic acid Chalcone Dobutamin Indapamide Morphine Proguanil Vinblastine Thioridazine Amiodarone Chloramphenicol Dopamine Indomethacin Nalidixic acid Promazine Vitamin A Thiorphan Amodiaquine Chlordiazepoxide Dothiepin Indoprofen Naproxen Promethazine Vitamin B (see also Thiothixene Amonafide Chloroquine Doxorubicin Isoprenaline Neocarzinostatin Proxibarbital riboflavine) Tiaprofenic acid Amphotericin B Chlorpromazine DTIC Isopropylamino- Nimodipine Psoralen -

Box Sets of the Latest Shows
More Box sets of the latest shows 15th April 2016 Customers with the Family Bundle and existing HD customers can enjoy more Box Sets of the latest shows than any other pay TV or online subscription service in the UK. Now customers can get up to speed with the shows everyone’s talking about from the very beginning. And with new titles added every month, there’s always something new to discover. We have compared our currently available TV Box Sets against other Pay TV and online subscription services in the UK and have more Box Sets* of shows that meet any of the below criteria: - Shows for which the first run of the latest series is currently on TV - Shows which have aired in the last 12 months - Shows for which a new series will be showing in the next 12 months *For a show to be considered a ‘box set’ it must have at least one series that is 60% complete in a given service on the date the audit was undertaken. *Kids content is not classified as TV Box Sets for the purposes of this comparison Monthly comparison of box sets of the latest shows: Last updated 4th April 2016 TalkTalk Amazon Prime Sky TV Netflix Virgin NowTV (inc.YouVie Instant Video w) Box sets of the latest shows 159 92 131 111 44 9 180 160 140 120 100 80 Shows 60 40 20 0 Number of Boxsets of the Latest Latest the of Boxsets of Number Sky TV Netflix Virgin NowTV Amazon Prime TalkTalk Instant Video (inc.YouView) Other Pay TV or Online Substantiation Services Comparison based on box sets of shows available on each service on the following dates: Sky Box Sets Netflix Virgin Now TV Amazon TalkTalk Date of last Audit 04/04/16 04/04/16 07/04/16 04/04/16 04/04/16 04/04/16 Title Sky Netflix Virgin NowTV Amazon TalkTalk 24 Y Y Blacklist, The Y Y Boardwalk Empire Y Y Broadchurch Y Y Californication Y Y Y Criminal Minds Y Y Elementary Y Y Fortitude Y Y Game of Thrones Y Y Girls Y Glee Y Y Gracepoint Y Y Grey's Anatomy Y Y Hannibal Y Y Jinx: The Life And Deaths of Robert Durst, TheY Y Mad Men Y Y Y Marvel's Agents of S.H.I.E.L.D. -

Promotion of Bone Formation by Fermented Soybean (Natto) Intake in Premenopausal Women
J Nutr Sci Vitaminol, 50,114-120, 2004 Promotion of Bone Formation by Fermented Soybean (Natto) Intake in Premenopausal Women Hironobu KATSUYAMA1,Seiji IDEGUCHI2,Masao FUKUNAGA3, Tatsushige FUKUNAGA4, Kiyofumi SAIJOHSand Shigeo SUNAMII Departments of 1Public Health, 2Health Care Medicine arid 3NuclearMedicine , Kawasaki Medical School,Kurashiki 701-0192, Japan 4Departrnent of Forensic Medicine and Sciences , Mie University School of Medicine, Tsu 514-8507, Japan 5Department of Hygiene , Kanazawa University School of Medicine and Graduate School of Medical Sciences, Kanazawa 920-8640, Japan (Received July 24, 2003) Summary A therapeutic agent of vitamin K2 is approved for the treatment of osteoporosis in Japan. However, little is known about the efficacy of dietary intake of vitamin K2for bone health. We compared the effects of various levels of fermented soybeans (Natto) intake , which contains plenty of vitamin K2, on bone stiffness and bone turnover markers in healthy premenopausal women, Seventy-three healthy premenopausal women were ran domly divided into four groups matched for age and parity categories . Natto was supplied as follows: Group 1(no intake), Group 2 (once per month), Group 3 (once per week) and Group 4 (three times per week). Subjects took Natto at a lunch for 1 y, and the stiffness index by quantitative ultrasound and bone turnover markers were assessed at baseline, 6 mo and 1 y There was no statistical difference in the stiffness index during the 1 y observation . How ever, bone specific alkaline phosphatase (BAP) in Group 4 was higher than that in Group 3 at 1 y and undercarboxylated osteocalcin (Glu) in Group 4 was significantly lower than those in Groups 1, 2 and 3 at 6 mo. -

Pharmaceuticals and Medical Devices Safety Information No
Pharmaceuticals and Medical Devices Safety Information No. 215 July 2005 Table of Contents 1. Important Safety Information ································································ 2 .1. Ethionamide ······················································································ 2 .2. Etodolac ···························································································· 5 .3. Gemcitabine Hydrochloride ····························································· 10 .4. Omeprazole, Omeprazole Sodium ·················································· 12 2. Revision of PRECAUTIONS (No.167) Tiaprofenic Acid (and 17 others) ·································································· 16 3. List of products subject to Early Post-marketing Phase Vigilance ·············································· 23 This Pharmaceuticals and Medical Devices Safety Information (PMDSI) is issued based on safety information collected by the Ministry of Health, Labour and Welfare. It is intended to facilitate safer use of pharmaceuticals and medical devices by healthcare providers. PMDSI is available on the Pharmaceuticals and Medical Devices Agency website (http://www.pmda.go.jp/english/index.html) and on the MHLW website (http://www.mhlw.go.jp/, Japanese only). Published by Translated by Pharmaceutical and Food Safety Bureau, Pharmaceuticals and Medical Devices Agency Ministry of Health, Labour and Welfare Pharmaceutical and Food Safety Bureau, Office of Safety, Ministry of Health, Labour and Welfare Pharmaceuticals and Medical -

Application of Marsplines and Descriptors Encoded in SMILES String
Supplementary Materials Predicting value of binding constants of organic ligands to beta-cyclodextrin: application of MARSplines and descriptors encoded in SMILES string Piotr Cysewski1 and Maciej Przybyłek1,* 1 Chair and Department of Physical Chemistry, Faculty of Pharmacy, Collegium Medicum of Bydgoszcz, Nicolaus Copernicus University in Toruń, Kurpińskiego 5, 85-950 Bydgoszcz, Poland; [email protected] Table. S1 Experimental and calculated LnK values. No. Chemical name SMILES lnKexp* lnKest Set (ext. validation) 1 Acetonitrile CC#N -1.474 -1.278 test 2 Methanol CO -1.128 -1.235 training 3 Acetaldehyde CC=O -0.622 -0.225 training 4 1,2-Ethanediol C(CO)O -0.437 0.828 training 5 Ethanol CCO -0.069 0.504 training 6 2-Methoxyethanol COCCO 0.507 0.711 test 7 Acetone CC(=O)C 0.967 0.619 training 8 1-Propanol CCCO 1.312 1.410 training 9 2-Propanol CC(C)O 1.451 1.988 training 10 1,4-Butanediol C(CCO)CO 1.474 2.177 training 11 1,3-Propanediol C(CO)CO 1.543 1.512 test 12 Cyclobutanol C1CC(C1)O 2.717 3.234 training 13 2-Butanol CCC(C)O 2.740 2.849 training 14 1-Butanol CCCCO 2.809 2.739 training 15 1,5-Pentanediol C(CCO)CCO 2.809 2.860 training 1 No. Chemical name SMILES lnKexp* lnKest Set (ext. validation) 16 3-Pentanol CCC(CC)O 3.108 4.305 test 17 Diethylamine CCNCC 3.132 2.355 training 18 Chloroform C(Cl)(Cl)Cl 3.293 3.119 training 19 Tetrahydrofuran C1CCOC1 3.385 2.874 training 20 Griseofulvin C[C@@H]1CC(=O)C=C([C@]12C(=O)C3=C(O2)C(= 3.385 3.929 training C(C=C3OC)OC)Cl)OC 21 2-Pentanol CCCC(C)O 3.431 4.916 training 22 3-Cyanophenylacetate -

Commmon Factors for Parkinson's Disease and Crohn's Disease
© The MITRE Corporation. All rights reserved LITERATURE-RELATED DISCOVERY: COMMON FACTORS FOR PARKINSON’S DISEASE AND CROHN’S DISEASE Dr. Ronald N. Kostoff The MITRE Corporation 7515 Colshire Drive McLean, VA 22102 DISCLAIMER (The views contained in this paper are solely those of the author and do not reflect the views of the MITRE Corporation) ACKNOWLEDGEMENT This project was supported by MITRE internal research funding. KEYWORDS Literature-related discovery; Text mining; Scientometrics; Parkinson‟s disease; Crohn‟s disease; neurodegeneration; autoimmunity; inflammation © The MITRE Corporation. All rights reserved ABSTRACT Literature-related discovery (LRD) is the linking of two or more literature concepts that have heretofore not been linked (i.e., disjoint), in order to produce novel, interesting, and intelligible knowledge (i.e., potential discovery). The mainstream software for assisting LRD is Arrowsmith, and it generates intermediate linking literatures by matching title phrases from two disjoint literatures (literatures that do not share common records). Arrowsmith then prioritizes these linking phrases through a series of text-based filters. The present study examines another route to linking disjoint literatures (shared references) through a process called bibliographic coupling. Two disjoint literatures were selected: Parkinson‟s Disease (PD) (neurodegeneration) and Crohn‟s Disease (CD)(autoimmune). Three cases were examined: matching phrases in records with no shared references; shared references in records with no matching phrases; matching phrases in records with shared references. In addition, the main themes in the body of shared references were examined through grouping techniques to identify the myriad linkages between the two literatures. No concepts were identified in the matching phrases/no shared references records that could not be found in the matching phrases/shared references records. -

Vitamin K Monograph
Vitamin K Natural Standard Bottom Line Monograph, Copyright © 2008 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions. While some complementary and alternative techniques have been studied scientifically, high-quality data regarding safety, effectiveness, and mechanism of action are limited or controversial for most therapies. Whenever possible, it is recommended that practitioners be licensed by a recognized professional organization that adheres to clearly published standards. In addition, before starting a new technique or engaging a practitioner, it is recommended that patients speak with their primary healthcare provider(s). Potential benefits, risks (including financial costs), and alternatives should be carefully considered. The below monograph is designed to provide historical background and an overview of clinically-oriented research, and neither advocates for or against the use of a particular therapy. Related Terms: 2-methyl-1,4-naphthoquinone, AquaMEPHYTON®, Konakion®, menadiol (not available in United States), menadiol diphosphate (vitamin K3), menadione, menaquinones, menatetrenone, Mephyton®, Phylloquinone®, Phytomenadione®, phytonadione. The name "vitamin K" refers to a group of chemically similar fat-soluble compounds called naphthoquinones. Vitamin K1 (phytonadione) is the natural form of vitamin K, which is found in plants and provides the primary source of vitamin K to humans through dietary consumption. Vitamin K2 compounds (menaquinones) are made by bacteria in the human gut and provide a smaller amount of the human vitamin K requirement. Vitamin K1 is commercially manufactured for medicinal use under several brand names (Phylloquinone®, Phytonadione®, AquaMEPHYTON®, Mephyton®, Konakion®). -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Menatetrenone, a Vitamin K2 Analogue, Inhibits Hepatocellular
Cancer Therapy: Preclinical Menatetrenone, a Vitamin K2 Analogue, Inhibits Hepatocellular Carcinoma Cell Growth by Suppressing Cyclin D1 Expression through Inhibition of Nuclear Factor KBActivation Iwata Ozaki,1, 2 Hao Zhang,1, 3 To s hi hi ko Mi z u t a , 1Ya s u s hi Id e ,1Yuichiro Eguchi,1TsutomuYasutake,1 Toshiyuki Sakamaki,4 Richard G. Pestell,4 and KyosukeYamamoto1 Abstract Purpose: Menatetrenone, a vitamin K2 analogue, plays an important role in the production of blood coagulation factors. Menatetrenone has also bee shown to have antineoplastic effects against several cancer cell lines including hepatocellular carcinoma (HCC) cells. However, the mechanisms by which vitamin K2 inhibits HCC cell growth have not bee fully clarified, and we therefore investigated the molecular basis of vitamin K2^ induced growth inhibition of HCC cells. Experimental Design: HCC cells were treated with vitamin K2 and the expression of several growth-related genes including cyclin-dependent kinase inhibitors and cyclin D1 was examined at the mRNA and protein levels. A reporter gene assay of the cyclin D1promoter was done under vitamin K2 treatment.The regulation of nuclear factor nB(NF-nB) activation was investigated by aNF-nB reporter gene assay, an electrophoretic mobility shift assay, aWestern blot for phosphor- ylated InB, and an in vitro kinase assay for InB kinase (IKK).We also examined the effect of vitamin K2 on the growth of HCC cells transfected with p65 or cyclin D1. Results:Vitamin K2 inhibited cyclin D1mRNA and protein expression in a dose-dependent man- ner in the HCC cells. Vitamin K2 also suppressed the NF-nB binding site-dependent cyclin D1 promoter activity and suppressed the basal, 12-O-tetradecanoylphorbol-13-acetate (TPA)^, TNF-a^, and interleukin (IL)-1^ induced activation of NF-nB binding and transactivation. -

(12) Patent Application Publication (10) Pub. No.: US 2011/0064805 A1 Obae Et Al
US 2011 OO64805A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0064805 A1 Obae et al. (43) Pub. Date: Mar. 17, 2011 (54) POROUS CELLULOSE AGGREGATE AND Publication Classification MOLDING COMPOSITION THEREOF (51) Int. Cl. (75) Inventors: Kazuhiro Obae, Tokyo (JP); A69/20 (2006.01) HidekiO O Amakawa, Tokyo (JP); A6IR 9/16 (2006.01) Ichirochiro Ibuki,Ibuki.T Tokyo (JP)JP A6II 3/663/167 (2006.01) (73) Assignee: ASAHIKASE CHEMICALS A63L/92A6II 3/34 308:2006.O1 CORPORATION, Tokyo (JP) CI3K L/02 (2006.01) 21) Appl. No.: 12A926,318 (52) U.S. Cl. ......... 424/464; 424/499; 514/630; 514/622: (21) Appl. No 9 514/474; 514/570; 127/34; 127/37 (22) Filed: Nov. 9, 2010 (57) ABSTRACT Related U.S. Application Data A porous cellulose aggregate characterized by having a sec - - - ondary aggregate structure resulting from aggregation of pri (62) Division of application No. 11/918,979, filed on Oct. mary cellulose particles, having a pore Volume within a par 22, 2007, filed as application No. PCT/JP2006/308414 ticle of 0.265 to 2.625 cm/g, containing I-type crystals and on Apr. 21, 2006. having an average particle size of over 30 to 250 Lim, a specific surface area of 0.1 to less than 20 m/g, a repose angle of 25° (30) Foreign Application Priority Data to less than 44° and a swelling degree of 5% or more, and characterized by having the property of disintegrating in Apr. 22, 2005 (JP) ................................. 2005-124477 Water. Patent Application Publication Mar.