Alternative and Complimentary Methods in the Treatment of Sleep Disorders And/Or Insomnia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of Pharmacology and Experimental Therapeutics
Journal of Pharmacology and Experimental Therapeutics Molecular Determinants of Ligand Selectivity for the Human Multidrug And Toxin Extrusion Proteins, MATE1 and MATE-2K Bethzaida Astorga, Sean Ekins, Mark Morales and Stephen H Wright Department of Physiology, University of Arizona, Tucson, AZ 85724, USA (B.A., M.M., and S.H.W.) Collaborations in Chemistry, 5616 Hilltop Needmore Road, Fuquay-Varina NC 27526, USA (S.E.) Supplemental Table 1. Compounds selected by the common features pharmacophore after searching a database of 2690 FDA approved compounds (www.collaborativedrug.com). FitValue Common Name Indication 3.93897 PYRIMETHAMINE Antimalarial 3.3167 naloxone Antidote Naloxone Hydrochloride 3.27622 DEXMEDETOMIDINE Anxiolytic 3.2407 Chlordantoin Antifungal 3.1776 NALORPHINE Antidote Nalorphine Hydrochloride 3.15108 Perfosfamide Antineoplastic 3.11759 Cinchonidine Sulfate Antimalarial Cinchonidine 3.10352 Cinchonine Sulfate Antimalarial Cinchonine 3.07469 METHOHEXITAL Anesthetic 3.06799 PROGUANIL Antimalarial PROGUANIL HYDROCHLORIDE 100MG 3.05018 TOPIRAMATE Anticonvulsant 3.04366 MIDODRINE Antihypotensive Midodrine Hydrochloride 2.98558 Chlorbetamide Antiamebic 2.98463 TRIMETHOPRIM Antibiotic Antibacterial 2.98457 ZILEUTON Antiinflammatory 2.94205 AMINOMETRADINE Diuretic 2.89284 SCOPOLAMINE Antispasmodic ScopolamineHydrobromide 2.88791 ARTICAINE Anesthetic 2.84534 RITODRINE Tocolytic 2.82357 MITOBRONITOL Antineoplastic Mitolactol 2.81033 LORAZEPAM Anxiolytic 2.74943 ETHOHEXADIOL Insecticide 2.64902 METHOXAMINE Antihypotensive Methoxamine -

Management of Status Epilepticus
Published online: 2019-11-21 THIEME Review Article 267 Management of Status Epilepticus Ritesh Lamsal1 Navindra R. Bista1 1Department of Anaesthesiology, Tribhuvan University Teaching Address for correspondence Ritesh Lamsal, MD, DM, Department Hospital, Institute of Medicine, Tribhuvan University, Nepal of Anaesthesiology, Tribhuvan University Teaching Hospital, Institute of Medicine, Tribhuvan University,Kathmandu, Nepal (e-mail: [email protected]). J Neuroanaesthesiol Crit Care 2019;6:267–274 Abstract Status epilepticus (SE) is a life-threatening neurologic condition that requires imme- diate assessment and intervention. Over the past few decades, the duration of seizure Keywords required to define status epilepticus has shortened, reflecting the need to start thera- ► convulsive status py without the slightest delay. The focus of this review is on the management of con- epilepticus vulsive and nonconvulsive status epilepticus in critically ill patients. Initial treatment ► neurocritical care of both forms of status epilepticus includes immediate assessment and stabilization, ► nonconvulsive status and administration of rapidly acting benzodiazepine therapy followed by nonbenzodi- epilepticus azepine antiepileptic drug. Refractory and super-refractory status epilepticus (RSE and ► refractory status SRSE) pose a lot of therapeutic problems, necessitating the administration of contin- epilepticus uous infusion of high doses of anesthetic agents, and carry a high risk of debilitating ► status epilepticus morbidity as well as mortality. ► super-refractory sta- tus epilepticus Introduction occur after 30 minutes of seizure activity. However, this working definition did not indicate the need to immediately Status epilepticus (SE) is a medical and neurologic emergency commence treatment and that permanent neuronal injury that requires immediate evaluation and treatment. It is associat- could occur by the time a clinical diagnosis of SE was made. -

Insomnia Across the Lifespan: Treating This Common Condition
2/20/2019 Insomnia Across the Lifespan: Treating This Common Condition Wendy L. Wright MS, ANP-BC, FNP-BC, FAANP, FAAN, FNAP Adult / Family Nurse Practitioner Owner – Wright & Associates Family Healthcare @ Amherst and @ Concord, NH Owner – Partners in Healthcare Education © Wright, 2019 1 1 Disclosures • Speaker Bureau: Pfizer, Merck, Sanofi Pasteur • Consultant: Pfizer, Merck, Sanofi Pasteur © Wright, 2019 2 2 Objectives • Upon completion of this session, the participant will be able to: • Discuss the incidence and prevalence of insomnia across the lifespan • Identify the appropriate work-up of the individual with insomnia • Discuss nonpharmacologic and pharmacologic treatment options for the patient with insomnia © Wright, 2019 3 3 Wright, 2019 1 2/20/2019 What Is Insomnia? • Insomnia: • Difficulty initiating or maintaining sleep; sleep that is nonrestorative despite having an adequate opportunity and no abnormal environmental circumstances; and accompanied by daytime somnolence (Sateia, M.J. et. al, 2017) © Wright, 2019 4 4 What Is Insomnia? • DSM-V definition: • Difficulty initiating and / or • Difficulty maintaining and / or • Waking earlier than desired AND • Occurring at least 3 nights per week for at least 3 months AND • Dissatisfaction with sleep http://www.psychiatrictimes.com/special-reports/review-changes-dsm-5-sleep-wake-disorders accessed 08- 08-2018 © Wright, 2019 5 5 DSM-5 Diagnostic Criteria https://practicingclinicians.com/CE-CME/sleep/enhancing-the-management-of-insomnia-in-older-patients/MPCE90716 © Wright, 2019 6 -

Drugs That Act in the Cns
DRUGS THAT ACT IN THE CNS Anxiolytic and Hypnotic Drugs Dr Karamallah S. Mahmood PhD Clinical Pharmacology 1 OTHER ANXIOLYTIC AGENTS/ A. Antidepressants Many antidepressants are effective in the treatment of chronic anxiety disorders and should be considered as first-line agents, especially in patients with concerns for addiction or dependence. Selective serotonin reuptake inhibitors (SSRIs) or serotonin/norepinephrine reuptake inhibitors (SNRIs) may be used alone or prescribed in combination with a benzodiazepine. SSRIs and SNRIs have a lower potential for physical dependence than the benzodiazepines and have become first-line treatment for GAD. 2 OTHER ANXIOLYTIC AGENTS/ B. Buspirone Buspirone is useful for the chronic treatment of GAD and has an efficacy comparable to that of the benzodiazepines. It has a slow onset of action and is not effective for short-term or “as-needed” treatment of acute anxiety states. The actions of buspirone appear to be mediated by serotonin (5-HT1A) receptors, although it also displays some affinity for D2 dopamine receptors and 5-HT2A serotonin receptors. Buspirone lacks the anticonvulsant and muscle-relaxant properties of the benzodiazepines. 3 OTHER ANXIOLYTIC AGENTS B. Buspirone The frequency of adverse effects is low, with the most common effects being headaches, dizziness, nervousness, nausea, and light-headedness. Sedation and psychomotor and cognitive dysfunction are minimal, and dependence is unlikely. Buspirone does not potentiate the CNS depression of alcohol. 4 V. BARBITURATES The barbiturates were formerly the mainstay of treatment to sedate patients or to induce and maintain sleep. Today, they have been largely replaced by the benzodiazepines, primarily because barbiturates induce tolerance and physical dependence and are associated with very severe withdrawal symptoms. -

Behandling Av Ångestsyndrom
Behandling av ångestsyndrom En systematisk litteraturöversikt Volym 2 September 2005 SBU • Statens beredning för medicinsk utvärdering The Swedish Council on Technology Assessment in Health Care SBU utvärderar sjukvårdens metoder SBU (Statens beredning för medicinsk utvärdering) är en statlig myn- Behandling av ångestsyndrom dighet som utvärderar sjukvårdens metoder. SBU analyserar nytta och kostnader för olika medicinska metoder och jämför vetenskapens stånd- punkt med svensk vårdpraxis. Målet är ett bättre beslutsunderlag för En systematisk litteraturöversikt alla som avgör vilken sjukvård som ska bedrivas. Välkommen att besöka SBU:s hemsida, www.sbu.se Volym 2 SBU ger ut tre serier av rapporter. I den första serien presenteras utvär- deringar som utförts av SBU:s projektgrupper. Dessa utvärderingar Projektgrupp åtföljs alltid av en sammanfattning och slutsatser fastställda av SBU:s Lars von Knorring Ingrid Håkanson styrelse och råd. Denna rapportserie ges ut med gula omslag. I den andra (ordförande) (projektassistent) serien, med vita omslag, presenteras aktuella kunskaper inom något Viveka Alton Lundberg Agneta Pettersson område av sjukvården där behov av utvärdering kan föreligga. Den tredje Vanna Beckman (projektledare under serien, Alert-rapporterna, avser tidiga bedömningar av nya metoder inom (deltog 1995–2002) perioden 2004–2005) hälso- och sjukvården. Susanne Bejerot Per-Anders Rydelius Roland Berg Sten Thelander (deltog 1995–2002) (projektledare under Cecilia Björkelund perioden 1995–2004) Per Carlsson Helene Törnqvist (deltog 1995–1999) (deltog 1999–2005) Elias Eriksson Kristian Wahlbeck (deltog 1995–2001) (deltog 2002–2005) Tom Fahlén Hans Ågren Mats Fredrikson Rapporten ”Behandling av ångestsyndrom” består av två volymer (nr 171/1+2) och kan beställas från: Externa granskare SBU, Box 5650, 114 86 Stockholm Fredrik Almqvist Per Høglend Besöksadress: Tyrgatan 7 Alv A. -

Comparison of Short-And Long-Acting Benzodiazepine-Receptor Agonists
J Pharmacol Sci 107, 277 – 284 (2008)3 Journal of Pharmacological Sciences ©2008 The Japanese Pharmacological Society Full Paper Comparison of Short- and Long-Acting Benzodiazepine-Receptor Agonists With Different Receptor Selectivity on Motor Coordination and Muscle Relaxation Following Thiopental-Induced Anesthesia in Mice Mamoru Tanaka1, Katsuya Suemaru1,2,*, Shinichi Watanabe1, Ranji Cui2, Bingjin Li2, and Hiroaki Araki1,2 1Division of Pharmacy, Ehime University Hospital, Shitsukawa, Toon, Ehime 791-0295, Japan 2Department of Clinical Pharmacology and Pharmacy, Neuroscience, Ehime University Graduate School of Medicine, Shitsukawa, Toon, Ehime 791-0295, Japan Received November 7, 2007; Accepted May 15, 2008 Abstract. In this study, we compared the effects of Type I benzodiazepine receptor–selective agonists (zolpidem, quazepam) and Type I/II non-selective agonists (zopiclone, triazolam, nitrazepam) with either an ultra-short action (zolpidem, zopiclone, triazolam) or long action (quazepam, nitrazepam) on motor coordination (rota-rod test) and muscle relaxation (traction test) following the recovery from thiopental-induced anesthesia (20 mg/kg) in ddY mice. Zolpidem (3 mg/kg), zopiclone (6 mg/kg), and triazolam (0.3 mg/kg) similarly caused an approximately 2-fold prolongation of the thiopental-induced anesthesia. Nitrazepam (1 mg/kg) and quazepam (3 mg/kg) showed a 6- or 10-fold prolongation of the anesthesia, respectively. Zolpidem and zopiclone had no effect on the rota-rod and traction test. Moreover, zolpidem did not affect motor coordination and caused no muscle relaxation following the recovery from the thiopental-induced anesthesia. However, zopiclone significantly impaired the motor coordination at the beginning of the recovery. Triazolam significantly impaired the motor coordination and muscle relaxant activity by itself, and these impairments were markedly exacerbated after the recovery from anesthesia. -

Herbal Remedies and Their Possible Effect on the Gabaergic System and Sleep
nutrients Review Herbal Remedies and Their Possible Effect on the GABAergic System and Sleep Oliviero Bruni 1,* , Luigi Ferini-Strambi 2,3, Elena Giacomoni 4 and Paolo Pellegrino 4 1 Department of Developmental and Social Psychology, Sapienza University, 00185 Rome, Italy 2 Department of Neurology, Ospedale San Raffaele Turro, 20127 Milan, Italy; [email protected] 3 Sleep Disorders Center, Vita-Salute San Raffaele University, 20132 Milan, Italy 4 Department of Medical Affairs, Sanofi Consumer HealthCare, 20158 Milan, Italy; Elena.Giacomoni@sanofi.com (E.G.); Paolo.Pellegrino@sanofi.com (P.P.) * Correspondence: [email protected]; Tel.: +39-33-5607-8964; Fax: +39-06-3377-5941 Abstract: Sleep is an essential component of physical and emotional well-being, and lack, or dis- ruption, of sleep due to insomnia is a highly prevalent problem. The interest in complementary and alternative medicines for treating or preventing insomnia has increased recently. Centuries-old herbal treatments, popular for their safety and effectiveness, include valerian, passionflower, lemon balm, lavender, and Californian poppy. These herbal medicines have been shown to reduce sleep latency and increase subjective and objective measures of sleep quality. Research into their molecular components revealed that their sedative and sleep-promoting properties rely on interactions with various neurotransmitter systems in the brain. Gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter that plays a major role in controlling different vigilance states. GABA receptors are the targets of many pharmacological treatments for insomnia, such as benzodiazepines. Here, we perform a systematic analysis of studies assessing the mechanisms of action of various herbal medicines on different subtypes of GABA receptors in the context of sleep control. -

Paper Clip—High Risk Medications
You belong. PAPER CLIP—HIGH RISK MEDICATIONS Description: Some medications may be risky for people over 65 years of age and there may be safer drug choices to treat some conditions. It is recommended that medications are reviewed regularly with your providers/prescriber to ensure patient safety. Condition Treated Current Medication(s)-High Risk Safer Alternatives to Consider Urinary Tract Infections (UTIs), Nitrofurantoin Bactrim (sulfamethoxazole/trimethoprim) or recurrent UTIs, or Prophylaxis (Macrobid, or Macrodantin) Trimpex/Proloprim/Primsol (trimethoprim) Allergies Hydroxyzine (Vistaril, Atarax) Xyzal (Levocetirizine) Anxiety Hydroxyzine (Vistaril, Atarax) Buspar (Buspirone), Paxil (Paroxetine), Effexor (Venlafaxine) Parkinson’s Hydroxyzine (Vistaril, Atarax) Symmetrel (Amantadine), Sinemet (Carbidopa/levodopa), Selegiline (Eldepryl) Motion Sickness Hydroxyzine (Vistaril, Atarax) Antivert (Meclizine) Nausea & Vomiting Hydroxyzine (Vistaril, Atarax) Zofran (Ondansetron) Insomnia Hydroxyzine (Vistaril, Atarax) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Eszopiclone (Lunesta) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Zolpidem (Ambien) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Zaleplon (Sonata) Ramelteon (Rozerem), Doxepin (Silenor) Muscle Relaxants Cyclobenazprine (Flexeril, Amrix) NSAIDs (Ibuprofen, naproxen) or Hydrocodone Codeine Tramadol (Ultram) Baclofen (Lioresal) Tizanidine (Zanaflex) Migraine Prophylaxis Elavil (Amitriptyline) Propranolol (Inderal), Timolol (Blocadren), Topiramate (Topamax), -
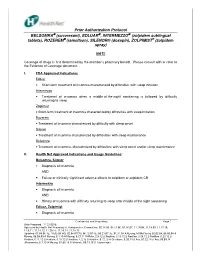
Prior Authorization Protocol BELSOMRA® (Suvorexant)
Prior Authorization Protocol BELSOMRA (suvorexant), EDLUAR , INTERMEZZO (zolpidem sublingual tablets), ROZEREM (ramelteon), SILENOR® (doxepin), ZOLPIMIST ® (zolpidem spray) NATL Coverage of drugs is first determined by the member’s pharmacy benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: Edluar • Short-term treatment of insomnia characterized by difficulties with sleep initiation Intermezzo • Treatment of insomnia when a middle-of-the-night awakening is followed by difficulty returning to sleep Zolpimist • Short-term treatment of insomnia characterized by difficulties with sleep initiation. Rozerem • Treatment of insomnia characterized by difficulty with sleep onset Silenor • Treatment of insomnia characterized by difficulties with sleep maintenance Belsomra • Treatment of insomnia, characterized by difficulties with sleep onset and/or sleep maintenance II. Health Net Approved Indications and Usage Guidelines: Belsomra, Silenor • Diagnosis of insomnia AND • Failure or clinically significant adverse effects to zolpidem or zolpidem CR Intermezzo • Diagnosis of insomnia AND • History of insomnia with difficulty returning to sleep after middle of the night awakening Edluar, Zolpimist • Diagnosis of insomnia Confidential and Proprietary Page 1 Date Prepared: 11.23.05JE Approved by Health Net Pharmacy & Therapeutic s Committee: 02.14.06, 04.11.06, 05.16.07, 11.19.08, 11.18.09, 11.17.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 05.09.06 JE, 10.03.06 RG, 02.08.07CM, -

Insomnia in Adults
New Guideline February 2017 The AASM has published a new clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults. These new recommendations are based on a systematic review of the literature on individual drugs commonly used to treat insomnia, and were developed using the GRADE methodology. The recommendations in this guideline define principles of practice that should meet the needs of most adult patients, when pharmacologic treatment of chronic insomnia is indicated. The clinical practice guideline is an essential update to the clinical guideline document: Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–349. SPECIAL ARTICLE Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults Sharon Schutte-Rodin, M.D.1; Lauren Broch, Ph.D.2; Daniel Buysse, M.D.3; Cynthia Dorsey, Ph.D.4; Michael Sateia, M.D.5 1Penn Sleep Centers, Philadelphia, PA; 2Good Samaritan Hospital, Suffern, NY; 3UPMC Sleep Medicine Center, Pittsburgh, PA; 4SleepHealth Centers, Bedford, MA; 5Dartmouth-Hitchcock Medical Center, Lebanon, NH Insomnia is the most prevalent sleep disorder in the general popula- and disease management of chronic adult insomnia, using existing tion, and is commonly encountered in medical practices. Insomnia is evidence-based insomnia practice parameters where available, and defined as the subjective perception of difficulty with sleep initiation, consensus-based recommendations to bridge areas where such pa- duration, consolidation, or quality that occurs despite adequate oppor- rameters do not exist. -
Zopiclone 7.5Mg Tablets PIL V5P1
PATIENT INFORMATION LEAFLET Patients with liver or kidney problems Very Rare (may affect up to 1 in 10,000 The usual starting dose is 3.75mg (½ a tablet). people) ZOPICLONE 7.5mg TABLETS • Change in blood tests (increase of liver Patients with Respiratory Insufficiency enzymes in the blood) Read this leaflet carefully BEFORE you start taking Zopiclone Tablets because it A reduced dosage is recommended (frequency cannot be estimated contains important information for you. Not known Pharmacode location from the available data) • Keep this leaflet. You may need to read it again. Use in Children and adolescents • Restlessness • If you have further questions, please ask your doctor or your pharmacist. Zopiclone Tablets are NOT recommended for • Delusion • This medicine has been prescribed for you only. Do not pass it on to others. It may harm children. • Anger them, even if their signs of illness are the same as yours. • Muscular weakness • If you get any of the side effects talk to your doctor or pharmacist. This includes any Your treatment will usually be for less than 4 • Loss of co-ordination possible side effects not listed in this leaflet. See section 4 weeks, and the doctor may reduce your dose near the end of your course. If you take • Loss of memory WHAT IS IN THIS LEAFLET Zopiclone longer than this, the medicine may • Double vision 1. What Zopiclone Tablets are and what they are used for not work as well, you may become dependent • Unusual skin sensations such as numbness, 2. What you need to know before you take Zopiclone Tablets and you may have withdrawal symptoms when burning, tingling or prickling (paraesthesia) 3. -

Nonbenzodiazepine Sedatives
24. Haller C, Thai D, Jacob P, Dyer JE: GHB urine concentrations after single-dose adminis- CHAPTER Nonbenzodiazepine tration in humans. J Anal Toxicol 30: 360, 2006. [PMID: 16872565] 25. Wong CG, Gibson KM, Snead O: From the street to the brain: neurobiology of the rec- Sedatives reational drug gamma-hydroxybutyric acid. Trends Pharmacol Sci 25: 29, 2004. [PMID: 184 14723976] Frank LoVecchio 26. White CM: Pharmacologic, pharmacokinetic, and clinical assessment of illicitly used γ-hydroxybutyrate. J Clin Pharmacol 57: 33, 2017. [PMID: 27198055] 27. Liakoni E, Walther F, Nickel CH, Liechti ME: Presentations to an urban emergency department in Switzerland due to acute γ-hydroxybutyrate toxicity. Scand J Trauma REFERENCES Resusc Emerg Med 24: 107, 2016. [PMID: 27581664] 28. Thai D, Dyer JE, Benowitz NL, Haller CA: Gamma-hydroxybutyrate and ethanol effects 1. Richey SM, Krystal AD: Pharmacological advances in the treatment of insomnia. Curr and interactions in humans. J Clin Psychopharm 26: 549, 2006. [PMID: 16974199] Pharm Des 17: 1471, 2011. [PMID: 21476952] 29. Miró Ò, Galicia M, Dargan P, et al: Intoxication by gamma hydroxybutyrate and related 2. http://www.digitalcitizensalliance.org/cac/alliance/content.aspx?page=Darknet. (Digital analogues: clinical characteristics and comparison between pure intoxication and that Citizens Alliance: Darknet Marketplace Watch: monitoring sales of illegal drugs on the combined with other substances of abuse. Toxicol Lett 277: 84, 2017. [PMID: 28579487] Darknet.) Accessed December 15, 2014. 30. Dietze P, Horyniak D, Agius P, et al: Effect of Intubation for gamma-hydroxybutyric acid 3. Loane C, Politis M: Buspirone: what is it all about? Brain Res 1461: 111, 2012.