Substance Use Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Treatment of Stimulant Use Disorders
UW PACC Psychiatry and Addictions Case Conference UW Medicine | Psychiatry and Behavioral Sciences TREATMENT OF STIMULANT USE DISORDERS Matt Iles-Shih, MD Addiction Psychiatry Fellow University Of Washington & VA Puget Sound Health Care System UW PACC ©2017 University of Washington GENERAL DISCLOSURES The University of Washington School of Medicine also gratefully acknowledges receipt of educational grant support for this activity from the Washington State Legislature through the Safety-Net Hospital Assessment, working to expand access to psychiatric services throughout Washington State. UW PACC ©2017 University of Washington SPEAKER DISCLOSURES No conflicts of interest/disclosures UW PACC ©2017 University of Washington OBJECTIVES 1. Brief overview of stimulant-related physiology & epidemiology 2. Recognizing & treating stimulant use disorders: . Diagnosis & management of acute effects (brief) . Psychotherapies (brief) . Pharmacotherapies 3. Special populations – ADHD in stimulant-abusing pts: to Rx, and how? UW PACC ©2017 University of Washington STIMULANTS: What Substances Are We Talking About? Cocaine Amphetamines: – Prescription Meds – Methamphetamine – Multiple other modified amphetamines MDMA (3,4-methylenedioxy-methamphetamine) [Note: mixed stimulant-psychodelic properties, w/↑serotonin > dopamine and abuse >> addiction.] Others: – Cathinones: Khat & Synthetics (e.g., “Bath Salts”) – Piperazine-like substances (various) – Phenylaklylpyrrolidines (various) UW PACC ©2017 University of Washington COMMONALITIES (WHAT MAKES A STIMULANT -

Management of Status Epilepticus
Published online: 2019-11-21 THIEME Review Article 267 Management of Status Epilepticus Ritesh Lamsal1 Navindra R. Bista1 1Department of Anaesthesiology, Tribhuvan University Teaching Address for correspondence Ritesh Lamsal, MD, DM, Department Hospital, Institute of Medicine, Tribhuvan University, Nepal of Anaesthesiology, Tribhuvan University Teaching Hospital, Institute of Medicine, Tribhuvan University,Kathmandu, Nepal (e-mail: [email protected]). J Neuroanaesthesiol Crit Care 2019;6:267–274 Abstract Status epilepticus (SE) is a life-threatening neurologic condition that requires imme- diate assessment and intervention. Over the past few decades, the duration of seizure Keywords required to define status epilepticus has shortened, reflecting the need to start thera- ► convulsive status py without the slightest delay. The focus of this review is on the management of con- epilepticus vulsive and nonconvulsive status epilepticus in critically ill patients. Initial treatment ► neurocritical care of both forms of status epilepticus includes immediate assessment and stabilization, ► nonconvulsive status and administration of rapidly acting benzodiazepine therapy followed by nonbenzodi- epilepticus azepine antiepileptic drug. Refractory and super-refractory status epilepticus (RSE and ► refractory status SRSE) pose a lot of therapeutic problems, necessitating the administration of contin- epilepticus uous infusion of high doses of anesthetic agents, and carry a high risk of debilitating ► status epilepticus morbidity as well as mortality. ► super-refractory sta- tus epilepticus Introduction occur after 30 minutes of seizure activity. However, this working definition did not indicate the need to immediately Status epilepticus (SE) is a medical and neurologic emergency commence treatment and that permanent neuronal injury that requires immediate evaluation and treatment. It is associat- could occur by the time a clinical diagnosis of SE was made. -

Insomnia Across the Lifespan: Treating This Common Condition
2/20/2019 Insomnia Across the Lifespan: Treating This Common Condition Wendy L. Wright MS, ANP-BC, FNP-BC, FAANP, FAAN, FNAP Adult / Family Nurse Practitioner Owner – Wright & Associates Family Healthcare @ Amherst and @ Concord, NH Owner – Partners in Healthcare Education © Wright, 2019 1 1 Disclosures • Speaker Bureau: Pfizer, Merck, Sanofi Pasteur • Consultant: Pfizer, Merck, Sanofi Pasteur © Wright, 2019 2 2 Objectives • Upon completion of this session, the participant will be able to: • Discuss the incidence and prevalence of insomnia across the lifespan • Identify the appropriate work-up of the individual with insomnia • Discuss nonpharmacologic and pharmacologic treatment options for the patient with insomnia © Wright, 2019 3 3 Wright, 2019 1 2/20/2019 What Is Insomnia? • Insomnia: • Difficulty initiating or maintaining sleep; sleep that is nonrestorative despite having an adequate opportunity and no abnormal environmental circumstances; and accompanied by daytime somnolence (Sateia, M.J. et. al, 2017) © Wright, 2019 4 4 What Is Insomnia? • DSM-V definition: • Difficulty initiating and / or • Difficulty maintaining and / or • Waking earlier than desired AND • Occurring at least 3 nights per week for at least 3 months AND • Dissatisfaction with sleep http://www.psychiatrictimes.com/special-reports/review-changes-dsm-5-sleep-wake-disorders accessed 08- 08-2018 © Wright, 2019 5 5 DSM-5 Diagnostic Criteria https://practicingclinicians.com/CE-CME/sleep/enhancing-the-management-of-insomnia-in-older-patients/MPCE90716 © Wright, 2019 6 -

Drugs That Act in the Cns
DRUGS THAT ACT IN THE CNS Anxiolytic and Hypnotic Drugs Dr Karamallah S. Mahmood PhD Clinical Pharmacology 1 OTHER ANXIOLYTIC AGENTS/ A. Antidepressants Many antidepressants are effective in the treatment of chronic anxiety disorders and should be considered as first-line agents, especially in patients with concerns for addiction or dependence. Selective serotonin reuptake inhibitors (SSRIs) or serotonin/norepinephrine reuptake inhibitors (SNRIs) may be used alone or prescribed in combination with a benzodiazepine. SSRIs and SNRIs have a lower potential for physical dependence than the benzodiazepines and have become first-line treatment for GAD. 2 OTHER ANXIOLYTIC AGENTS/ B. Buspirone Buspirone is useful for the chronic treatment of GAD and has an efficacy comparable to that of the benzodiazepines. It has a slow onset of action and is not effective for short-term or “as-needed” treatment of acute anxiety states. The actions of buspirone appear to be mediated by serotonin (5-HT1A) receptors, although it also displays some affinity for D2 dopamine receptors and 5-HT2A serotonin receptors. Buspirone lacks the anticonvulsant and muscle-relaxant properties of the benzodiazepines. 3 OTHER ANXIOLYTIC AGENTS B. Buspirone The frequency of adverse effects is low, with the most common effects being headaches, dizziness, nervousness, nausea, and light-headedness. Sedation and psychomotor and cognitive dysfunction are minimal, and dependence is unlikely. Buspirone does not potentiate the CNS depression of alcohol. 4 V. BARBITURATES The barbiturates were formerly the mainstay of treatment to sedate patients or to induce and maintain sleep. Today, they have been largely replaced by the benzodiazepines, primarily because barbiturates induce tolerance and physical dependence and are associated with very severe withdrawal symptoms. -

Cocaine Use Disorder
COCAINE USE DISORDER ABSTRACT Cocaine addiction is a serious public health problem. Millions of Americans regularly use cocaine, and some develop a substance use disorder. Cocaine is generally not ingested, but toxicity and death from gastrointestinal absorption has been known to occur. Medications that have been used as substitution therapy for the treatment of a cocaine use disorder include amphetamine, bupropion, methylphenidate, and modafinil. While pharmacological interventions can be effective, a recent review of pharmacological therapy for cocaine use indicates that psycho-social efforts are more consistent over medication as a treatment option. Introduction Cocaine is an illicit, addictive drug that is widely used. Cocaine addiction is a serious public health problem that burdens the healthcare system and that can be destructive to individual lives. It is impossible to know with certainty the extent of use but data from public health surveys, morbidity and mortality reports, and healthcare facilities show that there are millions of Americans who regularly take cocaine. Cocaine intoxication is a common cause for emergency room visits, and it is one drug that is most often involved in fatal overdoses. Some cocaine users take the drug occasionally and sporadically but as with every illicit drug there is a percentage of people who develop a substance use disorder. Treatment of a cocaine use disorder involves psycho-social interventions, pharmacotherapy, or a combination of the two. 1 ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com Pharmacology of Cocaine Cocaine is an alkaloid derived from the Erthroxylum coca plant, a plant that is indigenous to South America and several other parts of the world, and is cultivated elsewhere. -

Behandling Av Ångestsyndrom
Behandling av ångestsyndrom En systematisk litteraturöversikt Volym 2 September 2005 SBU • Statens beredning för medicinsk utvärdering The Swedish Council on Technology Assessment in Health Care SBU utvärderar sjukvårdens metoder SBU (Statens beredning för medicinsk utvärdering) är en statlig myn- Behandling av ångestsyndrom dighet som utvärderar sjukvårdens metoder. SBU analyserar nytta och kostnader för olika medicinska metoder och jämför vetenskapens stånd- punkt med svensk vårdpraxis. Målet är ett bättre beslutsunderlag för En systematisk litteraturöversikt alla som avgör vilken sjukvård som ska bedrivas. Välkommen att besöka SBU:s hemsida, www.sbu.se Volym 2 SBU ger ut tre serier av rapporter. I den första serien presenteras utvär- deringar som utförts av SBU:s projektgrupper. Dessa utvärderingar Projektgrupp åtföljs alltid av en sammanfattning och slutsatser fastställda av SBU:s Lars von Knorring Ingrid Håkanson styrelse och råd. Denna rapportserie ges ut med gula omslag. I den andra (ordförande) (projektassistent) serien, med vita omslag, presenteras aktuella kunskaper inom något Viveka Alton Lundberg Agneta Pettersson område av sjukvården där behov av utvärdering kan föreligga. Den tredje Vanna Beckman (projektledare under serien, Alert-rapporterna, avser tidiga bedömningar av nya metoder inom (deltog 1995–2002) perioden 2004–2005) hälso- och sjukvården. Susanne Bejerot Per-Anders Rydelius Roland Berg Sten Thelander (deltog 1995–2002) (projektledare under Cecilia Björkelund perioden 1995–2004) Per Carlsson Helene Törnqvist (deltog 1995–1999) (deltog 1999–2005) Elias Eriksson Kristian Wahlbeck (deltog 1995–2001) (deltog 2002–2005) Tom Fahlén Hans Ågren Mats Fredrikson Rapporten ”Behandling av ångestsyndrom” består av två volymer (nr 171/1+2) och kan beställas från: Externa granskare SBU, Box 5650, 114 86 Stockholm Fredrik Almqvist Per Høglend Besöksadress: Tyrgatan 7 Alv A. -
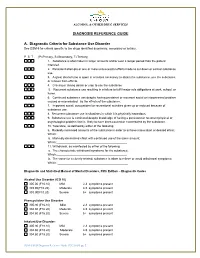
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -

DSM-5 Diagnoses and New ICD-10-CM Codes
DSM-5 DiAgnoses And New ICD-10-CM Codes As Ordered in the DSM-5 Classification DSM-5 Recommended DSM-5 Recommended Disorder ICD-10-CM Code for use ICD-10-CM Code for use through September 30, 2017 beginning October 1, 2017 Avoidant/Restrictive Food Intake Disorder F50.89 F50.82 Alcohol Use Disorder, Mild F10.10 F10.10 Alcohol Use Disorder, Mild, In early or sustained remission F10.10 F10.11 Alcohol Use Disorder, Moderate F10.20 F10.20 Alcohol Use Disorder, Moderate, In early or sustained F10.20 F10.21 remission Alcohol Use Disorder, Severe F10.20 F10.20 Alcohol Use Disorder, Severe, In early or sustained F10.20 F10.21 remission Cannabis Use Disorder, Mild F12.10 F12.10 Cannabis Use Disorder, Mild, In early or sustained F12.10 F12.11 remission Cannabis Use Disorder, Moderate F12.20 F12.20 Cannabis Use Disorder, Moderate, In early or sustained F12.20 F12.21 remission Cannabis Use Disorder, Severe F12.20 F12.20 Cannabis Use Disorder, Severe, In early or sustained F12.20 F12.21 remission Phencyclidine Use Disorder, Mild F16.10 F16.10 Phencyclidine Use Disorder, Mild, In early or sustained F16.10 F16.11 remission Phencyclidine Use Disorder, Moderate F16.20 F16.20 Phencyclidine Use Disorder, Moderate, In early or F16.20 F16.21 sustained remission Phencyclidine Use Disorder, Severe F16.20 F16.20 Phencyclidine Use Disorder, Severe, In early or sustained F16.20 F16.21 remission Other Hallucinogen Use Disorder, Mild F16.10 F16.10 Other Hallucinogen Use Disorder, Mild, In early or F16.10 F16.11 sustained remission Other Hallucinogen Use Disorder, -

Stimulant Use Disorder
Public Meeting on Patient-Focused Drug Development for Stimulant Use Disorder Tuesday, October 6, 2020 FDA will be streaming a live webcast of the meeting with the presentation slides, which is open to the public at: http://fda.yorkcast.com/webcast/Play/89f7acb8d56e4de8827d1ade8efa42661d. The webcast recording and presentation slides, along with a meeting transcript and summary report, will also be made publicly available after the meeting. #PFDD Welcome Robyn Bent, RN, MS | CAPT, U.S. Public Health Service Director, Patient-Focused Drug Development Program Office of Center Director Center for Drug Evaluation and Research U.S. Food and Drug Administration Agenda • Opening Remarks • Setting the Context • Overview of FDA’s Patient-Focused Drug Development Initiative • Overview of Stimulant Use Disorder • Overview of Discussion Format • Discussion Topic 1: Health Effects and Daily Impacts • Break • Discussion Topic 2: Current Approaches to Management • Discussion Topic 3: Impact of COVID-19 Pandemic on Stimulant Use Disorder • Closing Remarks www.fda.gov 3 Opening Remarks Admiral Brett P. Giroir, MD Assistant Secretary for Health United States Department of Health and Human Services Overview of FDA’s Patient-Focused Drug Development Initiative Theresa Mullin, PhD Associate Director for Strategic Initiatives Center for Drug Evaluation and Research U.S. Food and Drug Administration FDA’s role in medical product development and evaluation Review divisions at FDA (e.g., Division of Neurology, Division While FDA plays a critical of Psychiatry, etc.) provide FDA’s mission is to protect and oversight role in drug regulatory oversight during promote public health by development, it is just one part drug development, make evaluating the safety and of the process. -

Prevalence of Substance Use Disorders by Time Since First
Letters RESEARCH LETTER der and nicotine dependence did not differ between the 2 groups within 12 months of initiation but was higher for young Prevalence of Substance Use Disorders adults in subsequent periods. by Time Since First Substance Use Among young adults, prevalence of lifetime cocaine, meth- Among Young People in the US amphetamine, and heroin use in 2018 was 11.4% (95% CI, 10.7- Earlier age at drug initiation has been shown to be associated 12.1), 2.5% (95% CI, 2.2-2.8), and 1.3% (95% CI, 1.1-1.5), respec- with faster transition to substance use disorder (SUD).1 How- tively. Within 12 months of initiation, adjusted prevalence was ever, prevalence of specific SUDs as a function of time since higher for methamphetamine use disorder (24.8% [95% CI, first substance use among young people has not, to our knowl- 16.8-34.9]) and heroin use disorder (30.9% [95% CI, 20.6- edge, been investigated. We examined the prevalence of spe- 43.4]) than for cocaine use disorder (5.6% [95% CI, 4.2-7.4]). cific SUDs since first drug use (including tobacco, alcohol, can- Estimates for adolescents were not reported owing to limited nabis, cocaine, methamphetamine, and heroin) or prescription samples. misuse (including opioids, stimulants, and tranquilizers) in Prevalence of lifetime misuse of prescription drugs in adolescents aged 12 to 17 years and young adults aged 18 2014 was 9.2% (95% CI, 8.7-9.7) among adolescents and to 25 years. 26.3% (95% CI, 25.4-27.2) among young adults. -

Poster Session Imonday, December 7, 2015
Neuropsychopharmacology (2015) 40, S106–S271 & 2015 American College of Neuropsychopharmacology. All rights reserved 0893-133X/15 www.neuropsychopharmacology.org Poster Session I from the Forest Research Institute/ Actavis; NIH/ NCCIH; Monday, December 7, 2015 NIMH M2. Mental Healthcare Access and the Underserved: Are M1. Changes in the Functional Brain Connectivity and Our State-of-the-Art Treatments Getting to those who Verbal Memory Performance Following Yoga or Need It Most? Memory Training in Older Adults with Subjective Memory Complaints Daniel Jimenez*, Benjamin Cook, Margarita Alegria, Stephen Bartels, Charles Reynolds, Philip Harvey Helen Lavretsky*, Hongyu Yang, Harris Eyre, Amber Leaver, Katherine Narr, Dharma Khalsa University of Miami Miller School of Medicine, Miami, Florida, United States University of California Los Angeles Semel Institute for Neuroscience & Human Behavior, Los Angeles, Background: Disparities in mental health service use by racial/ California, United States ethnic minority older adults are well-documented. Attention is now turning to the question of whether racial/ethnic Background: Mind-body interventions, such as yoga, are disparities in mental healthcare are increasing or diminishing. used to reduce stress in the community samples. However, The net effect of changes in healthcare organization and clinical efficacy of such interventions for cognition remains immigration, along with any explicit policies designed to unclear. To-date, no studies have explored the effect of yoga reduce disparities, is not clear. The purpose of this study is to on cognition and resting state functional Magnetic Reso- examine national trends in the use of mental health services by nance Imaging (rs-fMRI). The present study was to explore older racial/ethnic minority adults. -

Outpatient Treatment for Withdrawal from Alcohol and Benzodiazepines
Considerations for Crisis Centers and Clinicians in Managing the Treatment of Alcohol or Benzodiazepine Withdrawal during the COVID-19 Epidemic: March 19, 2020 Overview: The COVID-19 Epidemic has created countless primary and secondary challenges for those delivering care to our most vulnerable populations. An additional concern has arisen for those with alcohol use disorder, benzodiazepine use disorder, or other conditions that increase the risk of seizures. While we recognize that there is high variability in the capacity for crisis centers and practitioners to receive and treat these individuals, we offer precautionary guidance to those that are prepared and capable. Alcohol use disorder, depending on the severity can be managed at various treatment settings. Those determined to be at high risk for withdrawal complications should receive treatment at higher levels of care, but crisis centers may be faced with a surge of patients seeking relief. Some of these patients can be safely managed at crisis centers. These patients would benefit from receiving medications to ameliorate some withdrawal symptoms and prevent withdrawal complications. Benzodiazepines are frequently utilized in a tapering fashion for medical withdrawal from alcohol or benzodiazepine dependence. It is likely that individuals will have difficulty being admitted to a facility that could safely administer these medications and there will be need for outpatient management of these conditions in the current medical emergency presented by the COVID-19 epidemic. SAMHSA urges providers to consider utilizing benzodiazepines in situations in which they believe that the individual would not benefit from administration of anticonvulsant medications that have been effective in treatment of alcohol withdrawal.