More of a Less Known Pathogen - Moraxella
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Biofilm Formation by Moraxella Catarrhalis
BIOFILM FORMATION BY MORAXELLA CATARRHALIS APPROVED BY SUPERVISORY COMMITTEE Eric J. Hansen, Ph.D. ___________________________ Kevin S. McIver, Ph.D. ___________________________ Michael V. Norgard, Ph.D. ___________________________ Philip J. Thomas, Ph.D. ___________________________ Nicolai S.C. van Oers, Ph.D. ___________________________ BIOFILM FORMATION BY MORAXELLA CATARRHALIS by MELANIE MICHELLE PEARSON DISSERTATION Presented to the Faculty of the Graduate School of Biomedical Sciences The University of Texas Southwestern Medical Center at Dallas In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center at Dallas Dallas, Texas March, 2004 Copyright by Melanie Michelle Pearson 2004 All Rights Reserved Acknowledgements As with any grand endeavor, there was a large supporting cast who guided me through the completion of my Ph.D. First and foremost, I would like to thank my mentor, Dr. Eric Hansen, for granting me the independence to pursue my ideas while helping me shape my work into a coherent story. I have seen that the time involved in supervising a graduate student is tremendous, and I am grateful for his advice and support. The members of my graduate committee (Drs. Michael Norgard, Kevin McIver, Phil Thomas, and Nicolai van Oers) have likewise given me a considerable investment of time and intellect. Many of the faculty, postdocs, students and staff of the Microbiology department have added to my education and made my experience here positive. Many members of the Hansen laboratory contributed to my work. Dr. Eric Lafontaine gave me my first introduction to M. catarrhalis. I hope I have learned from his example of patience, good nature, and hard work. -

Neisseria Acinetobacter, Moraxella ? and Kingella Based on Partial 16S Ribosomal DNA Sequence Analysis4
INTERNATIONALJOURNAL OF SYSTEMATICBACTERIOLOGY, July 1994, p. 387-391 Vol. 44, No. 3 0020-7713/94/$04.00 + 0 Copyright 0 1994, International Union of Microbiological Societies Phylogenetic Relationships between Some Members of the Genera Neisseria Acinetobacter, Moraxella ? and Kingella Based on Partial 16s Ribosomal DNA Sequence Analysis4. M. C. ENRIGHT,” P. E. CARTER, I. A. MACLEAN,AND H. McKENZIE Department of Medical Microbiology, Faculty of Medicine, University of Aberdeen, Foresterhill, Aberdeen, Scotland AB9 220 We obtained 16s ribosomal DNA (rDNA) sequence data for strains belonging to 11 species of Proteobacteria, including the type strains of Kingella kingae, Neisseria lactamica, Neisseria meningitidis, Moraxella lacunata subsp. lacunata, [Neisseria] ovis, Moraxella catarrhalis, Moraxella osloensis, [Moraxella] phenylpyruvica, and Acineto- bacter lwo$i, as well as strains of Neisseria subflava and Acinetobacter calcoaceticus. The data in a distance matrix constructed by comparing the sequences supported the proposal that the genera Acinetobacter and Moraxella and [N.] ovis should be excluded from the family Neisseriaceae. Our results are consistent with hybridization data which suggest that these excluded taxa should be part of a new family, the Moraxellaceae. The strains that we studied can be divided into the following five groups: (i) M. lacunata subsp. lacunata, [N.] ovis, and M. catarrhalis; (ii) M. osloensis; (iii) [M.]phenylpyruvica; (iv) A. calcoaceticus and A. lwofii; and (v) N. meningitidis, N. subflava, N. lactamica, and K. kingae. We agree with the previous proposal that [N.] ovis should be renamed Moraxella ovis, as this organism is closely related to Moraxella species and not to Neisseria species. The generically misnamed taxon [M.] phenylpyruvica belongs to the proposed family Moraxellaceae, but it is sufficiently different to warrant exclusion from the genus Moraxella. -
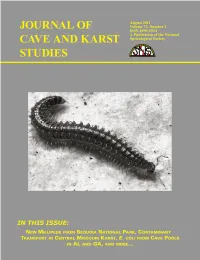
Cave-73-02-Fullr.Pdf
EDITORIAL Production Changes for Future Publication of the Journal of Cave and Karst Studies SCOTT ENGEL Production Editor The Journal of Cave and Karst Studies has experienced December 2011 issue, printed copies of the Journal will be budget shortfalls for the last several years for a multitude automatically distributed to paid subscribers, institutions, of reasons that include, but are not limited to, increased and only those NSS members with active Life and cost of paper, increased costs of shipping through the Sustaining level memberships. The remainder of the NSS United State Postal Service, increased submissions, and membership will be able to view the Journal electronically stagnant funding from the National Speleological Society online but will not automatically receive a printed copy. Full (NSS). The cost to produce the Journal has increased 5 to content of each issue of the Journal will be available for 20 percent per year for the last five years, yet the budget for viewing and downloading in PDF format at no cost from the the Journal has remained unchanged. To offset rising costs, Journal website www.caves.org/pub/journal. the Journal has implemented numerous changes over recent Anyone wishing to receive a printed copy of the Journal years to streamline the production and printing process. will be able to subscribe for an additional cost separate However, the increasing production costs, combined with from normal NSS dues. The cost and subscription process the increasing rate of good-quality submissions, has were still being determined at the time of this printing. resulted in the number of accepted manuscripts by the Once determined, the subscription information will be Journal growing faster than the acquisition of funding to posted on the Journal website. -

Moraxella Species: Infectious Microbes Identified by Use of Time-Of
Japanese Journal of Ophthalmology (2019) 63:328–336 https://doi.org/10.1007/s10384-019-00669-4 CLINICAL INVESTIGATION Moraxella species: infectious microbes identifed by use of time‑of‑fight mass spectrometry Shunsuke Takahashi1 · Kazuhiro Murata1 · Kenji Ozawa1 · Hiroki Yamada2 · Hideaki Kawakami3 · Asami Nakayama4 · Yuko Asano5 · Kiyofumi Mochizuki1 · Hiroshige Mikamo6 Received: 14 August 2018 / Accepted: 2 April 2019 / Published online: 4 July 2019 © Japanese Ophthalmological Society 2019 Abstract Purpose To report the clinical manifestations, identifcation, antimicrobial susceptibilities, and treatment outcomes of ocular infections caused by Moraxella species. Study design Retrospective study. Patients and methods The medical records of all patients treated at the Departments of Ophthalmology of the Ogaki Munici- pal Hospital and the Gifu University Graduate School of Medicine for ocular infections caused by Moraxella species between January 2011 and June 2017 were examined. The stored Moraxella species isolated from ocular samples were identifed by matrix-assisted laser desorption/ionization time-of-fight mass spectrometry (MALDI-TOF MS), molecular identifcation, and the biochemical properties. Results Sixteen eyes of 16 patients were treated for Moraxella ocular infections. The patients’ median age was 72 years. A predisposing systemic or ocular condition was identifed in 15 of the patients. Nine of the patients developed keratitis; four, conjunctivitis; and three, blebitis. M lacunata (6 eyes), M catarrhalis (6), M nonliquefaciens (3), and M osloensis (1) were identifed by MALDI-TOF MS. All isolates were sensitive to levofoxacin, tobramycin, ceftazidime, ceftriaxone, and cefa- zolin. Twelve patients with keratitis or blebitis were treated with various topical antimicrobial combinations, and systemic antibiotics were used in 10 of the 12 patients. -

Moraxella Bacteremia in Cancer Patients
Open Access Case Report DOI: 10.7759/cureus.15316 Moraxella Bacteremia in Cancer Patients Shamra Zaman 1 , John Greene 2 1. Medicine, University of South Florida, Tampa, USA 2. Internal Medicine, Moffitt Cancer Center, Tampa, USA Corresponding author: John Greene, [email protected] Abstract Moraxella is a gram-negative bacterium part of the Moraxellaceae family. It is a pathogen that is commonly found in the upper respiratory tract of humans. It is a rare cause of community-acquired pneumonia and can be found in immunocompromised individuals, especially those with impaired humoral immunity such as hypogammaglobulinemia and those with lung diseases. We present three cases of Moraxella infections at the Moffitt Cancer Center between the years 2011 and 2017. We performed a literature review of Moraxella bacteremia in cancer patients and included three patients, two with a history of multiple myeloma and one undergoing radiation therapy for non-small cell lung carcinoma. None of the patients died as a result of the infection. Moraxella infections can result in a range of severity with increasing resistance to antibiotic therapy. Categories: Infectious Disease, Oncology Keywords: moraxella, myeloma, respiratory tract, pneumonia, immunocompromised patient Introduction Moraxella is a gram-negative bacterium that has a coccobacillus shape [1]. Originally considered normal flora in the human respiratory system, it can cause respiratory tract infections [2]. It primarily affects adults with prior chronic lung disease and the immunosuppressed. The most common immunodeficiency is hypogammaglobulinemia, which is found in patients with multiple myeloma and chronic lymphocytic leukemia (CLL). Invasive infections include meningitis, pneumonia, and endocarditis [3,4]. We present the cases of three cancer patients with Moraxella infections that illustrate the most common risk factors that predispose to this infection. -

Component Causes of Infectious Bovine Keratoconjunctivitis - the Role of Moraxella Species in the Epidemiology of Infectious Bovine Keratoconjunctivitis
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Veterinary and Biomedical Sciences, Papers in Veterinary and Biomedical Science Department of 5-2021 Component Causes of Infectious Bovine Keratoconjunctivitis - The Role of Moraxella Species in the Epidemiology of Infectious Bovine Keratoconjunctivitis John Dustin Loy Matthew Hille Gabriele Maier Michael L. Clawson Follow this and additional works at: https://digitalcommons.unl.edu/vetscipapers Part of the Biochemistry, Biophysics, and Structural Biology Commons, Cell and Developmental Biology Commons, Immunology and Infectious Disease Commons, Medical Sciences Commons, Veterinary Microbiology and Immunobiology Commons, and the Veterinary Pathology and Pathobiology Commons This Article is brought to you for free and open access by the Veterinary and Biomedical Sciences, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Papers in Veterinary and Biomedical Science by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Component Causes of Infectious Bovine Keratoconjunctivitis - The Role of Moraxella Species in the Epidemiology of Infectious Bovine Keratoconjunctivitis a, a John Dustin Loy, DVM, PhD, DACVM *, Matthew Hille, DVM , b c Gabriele Maier, DVM, MPVM, PhD, DACVPM , Michael L. Clawson, PhD KEYWORDS Infectious bovine keratoconjunctivitis Moraxella bovis Moraxella bovoculi Moraxella ovis MALDI-TOF MS Genomics Pathogenesis KEY POINTS Moraxella bovis can cause infectious bovine keratoconjunctivitis (IBK). The role of M bovoculi in IBK is not fully understood. M bovis and M bovoculi appear to undergo genetic recombination with each other or other members of the Moraxellaceae. Recombination complicates their classification and potential role(s) in IBK pathogenesis. MALDI-TOF MS is used to identify M bovis, 2 major strains or genotypes of M bovoculi, M ovis, and other members of the Moraxellaceae. -

Moraxella Nonliquefaciens and M. Osloensis Are Important Moraxella Species That Cause Ocular Infections
microorganisms Article Moraxella nonliquefaciens and M. osloensis Are Important Moraxella Species That Cause Ocular Infections Samantha J. LaCroce 1, Mollie N. Wilson 2, John E. Romanowski 3, Jeffrey D. Newman 4 , Vishal Jhanji 3, Robert M. Q. Shanks 3 and Regis P. Kowalski 3,* 1 Department of Ophthalmology, Wake Forest University School of Medicine, Winston-Salem, NC 27157, USA; [email protected] 2 Clinical Laboratory—Microbiology, University of Pittsburgh Medical Center, Pittsburgh, PA 16148, USA; [email protected] 3 The Charles T. Campbell Ophthalmic Microbiology Laboratory, Department of Ophthalmology, University of Pittsburgh School of Medicine, Pittsburgh, PA 15213, USA; [email protected] (J.E.R.); [email protected] (V.J.); [email protected] (R.M.Q.S.) 4 Department of Biology, Lycoming College, Williamsport, PA 17701, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-(412)-647-7211; Fax: +1-(412)-647-5331 Received: 1 February 2019; Accepted: 31 May 2019; Published: 4 June 2019 Abstract: Moraxella is an ocular bacterial pathogen isolated in cases of keratitis, conjunctivitis, and endophthalmitis. Gram-negative brick-shaped diplobacilli from ocular specimens, and slow growth in culture, are early indications of Moraxella ocular infection; however, identifying Moraxella to species can be complex and inconsistent. In this study, bacteria consistent with Moraxella were identified to species using: (1) DNA sequencing coupled with vancomycin susceptibility, (2) MALDI-TOF mass spectrometry, and (3) the Biolog ID system. Study samples consisted of nine ATCC Moraxella controls, 82 isolates from keratitis, 21 isolates from conjunctivitis, and 4 isolates from endophthalmitis. The ATCC controls were correctly identified. For keratitis, 66 (80.5%) were identified as M. -

Type of the Paper (Article
Supplementary Materials S1 Clinical details recorded, Sampling, DNA Extraction of Microbial DNA, 16S rRNA gene sequencing, Bioinformatic pipeline, Quantitative Polymerase Chain Reaction Clinical details recorded In addition to the microbial specimen, the following clinical features were also recorded for each patient: age, gender, infection type (primary or secondary, meaning initial or revision treatment), pain, tenderness to percussion, sinus tract and size of the periapical radiolucency, to determine the correlation between these features and microbial findings (Table 1). Prevalence of all clinical signs and symptoms (except periapical lesion size) were recorded on a binary scale [0 = absent, 1 = present], while the size of the radiolucency was measured in millimetres by two endodontic specialists on two- dimensional periapical radiographs (Planmeca Romexis, Coventry, UK). Sampling After anaesthesia, the tooth to be treated was isolated with a rubber dam (UnoDent, Essex, UK), and field decontamination was carried out before and after access opening, according to an established protocol, and shown to eliminate contaminating DNA (Data not shown). An access cavity was cut with a sterile bur under sterile saline irrigation (0.9% NaCl, Mölnlycke Health Care, Göteborg, Sweden), with contamination control samples taken. Root canal patency was assessed with a sterile K-file (Dentsply-Sirona, Ballaigues, Switzerland). For non-culture-based analysis, clinical samples were collected by inserting two paper points size 15 (Dentsply Sirona, USA) into the root canal. Each paper point was retained in the canal for 1 min with careful agitation, then was transferred to −80ºC storage immediately before further analysis. Cases of secondary endodontic treatment were sampled using the same protocol, with the exception that specimens were collected after removal of the coronal gutta-percha with Gates Glidden drills (Dentsply-Sirona, Switzerland). -

Detection of Streptococcus Pneumoniae and Moraxella Catarrhalis in Patients with Paranasal Chronic Sinusitis by Polymerase Chain Reaction Method
Available online at www.sciencedirect.com ScienceDirect Journal of the Chinese Medical Association 79 (2016) 440e444 www.jcma-online.com Original Article Detection of Streptococcus pneumoniae and Moraxella catarrhalis in patients with paranasal chronic sinusitis by polymerase chain reaction method Ahmad Farajzadeh Sheikh a, Khadijeh Ahmadi b,*, Soheila Nikakhlagh c a Health Research Institute, Infectious and Tropical Diseases Research Center, Department of Microbiology, Medicine Faculty, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran b Department of Microbiology, Medicine Faculty, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran c Head and Neck Surgery, Hearing and Speech Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran Received April 27, 2015; accepted January 18, 2016 Abstract Background: Sinusitis is a complex involvement of the upper respiratory system by bacteria, viruses, fungi, or other allergens. Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis are the dominant bacterial microorganisms involved in acute sinusitis, whereas in chronic sinusitis, Staphylococcus aureus and some anaerobic bacteria are the prevailing pathogens. Appropriate antibiotic treatment requires sinusitis bacteriology assessment. The aim of this study was to isolate bacteria in clinical samples from patients with chronic sinusitis. Methods: A total of 55 samples were collected from patients with chronic sinusitis undergoing surgery at Imam Khomeini Hospital in Ahvaz, Iran. Samples were cultured in conventional medium, and for each culture, Gram staining, catalase, coagulase, oxidase, and DNAse tests were performed and isolates were stored for polymerase chain reaction analysis. Results: Twenty-three isolates were obtained from five patients, including S. aureus (23.6%), Rhizomucor (1.8%), and Escherichia (1.8%) by the culture method and M. -

Extensive Subclinical Sinusitis Leading to Moraxella Osloensis Meningitis
IDCases 6 (2016) 39–42 Contents lists available at ScienceDirect IDCases journal homepage: www.elsevier.com/locate/idcr Case report Extensive subclinical sinusitis leading to Moraxella osloensis meningitis a, a b a a b a,c A. Fox-Lewis *, G. Coltart , S. Rice , R. Sen , Y. Gourtsoyannis , H. Hyare , R.K. Gupta a Division of Infection, University College London Hospital NHS Foundation Trust, London, UK b Radiology Department, University College London Hospital NHS Foundation Trust, London, UK c Department of Infection, University College London, London, UK A R T I C L E I N F O A B S T R A C T Article history: Received 20 July 2016 We report a case of a 31 year old male with extensive subclinical sinusitis leading to erosion in the Received in revised form 19 August 2016 cribriform plate and subsequent meningitis caused by the organism Moraxella osloensis. The patient Accepted 19 August 2016 presented to the emergency department with rapid onset confusion, neck stiffness and headache. Inflammatory markers, renal and liver function, and a chest radiograph were all normal. CT Head showed extensive polyp disease in the paranasal sinuses with expansion of the left frontal sinus and CT Sinuses revealed an area of low attenuation in the cribriform plate consistent with bony erosion. MRI Head showed thick loculated sinus inflammation. Lumbar puncture yielded CSF with a high white cell count of predominantly mononuclear cells, no visible organisms and an elevated protein. CSF microscopy, culture and viral PCR were not diagnostic, and so the CSF was sent for 16S rDNA PCR screening, which identified the rDNA of Moraxella osloensis. -

Investigation of Gram-Negative Bacterial
Investigation of Gram-negative bacterial surface glycans: characterisation of Moraxella bovis lipooligosaccharide and progress towards developing a Nontypeable Haemophilus influenzae/Moraxella catarrhalis vaccine candidate Author Singh, Sanjesh Published 2019 Thesis Type Thesis (PhD Doctorate) School School of Medical Science DOI https://doi.org/10.25904/1912/2443 Copyright Statement The author owns the copyright in this thesis, unless stated otherwise. Downloaded from http://hdl.handle.net/10072/388637 Griffith Research Online https://research-repository.griffith.edu.au Investigation of Gram-negative bacterial surface glycans: characterisation of Moraxella bovis lipooligosaccharide and progress towards developing a Nontypeable Haemophilus influenzae/Moraxella catarrhalis vaccine candidate TITLE PAGE Sanjesh Singh BHSc, MMedRes A Thesis Submitted to the Griffith Graduate Research School for the Fulfilment of the Requirement for the Degree of Doctor of Philosophy December 2018 Menzies Health Institute, School of Medical Science & Institute for Glycomics Griffith University “Failure is the condiment that gives success its flavour” Truman Capote ii STATEMENT OF ORIGINALITY This work has not been previously submitted for a degree or diploma in any university. To the best of my knowledge and belief, the thesis contains no material previously published or written by another person except where due reference is made in the thesis itself. Sanjesh Singh December 2018 iii ACKNOWLEDGMENTS This project would not have been possible without the financial support from the School of Medical Science, Griffith University Postgraduate Research Scholarship and The John Viller’s Trust. I would like to extend my sincere thanks to the School of Medical Science and Institute for Glycomics for permitting me to undertake this project and to use their facilities. -

Identification of Pseudomonas Species and Other Non-Glucose Fermenters
UK Standards for Microbiology Investigations Identification of Pseudomonas species and other Non- Glucose Fermenters Issued by the Standards Unit, Microbiology Services, PHE Bacteriology – Identification | ID 17 | Issue no: 3 | Issue date: 13.04.15 | Page: 1 of 41 © Crown copyright 2015 Identification of Pseudomonas species and other Non-Glucose Fermenters Acknowledgments UK Standards for Microbiology Investigations (SMIs) are developed under the auspices of Public Health England (PHE) working in partnership with the National Health Service (NHS), Public Health Wales and with the professional organisations whose logos are displayed below and listed on the website https://www.gov.uk/uk- standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical- laboratories. SMIs are developed, reviewed and revised by various working groups which are overseen by a steering committee (see https://www.gov.uk/government/groups/standards-for-microbiology-investigations- steering-committee). The contributions of many individuals in clinical, specialist and reference laboratories who have provided information and comments during the development of this document are acknowledged. We are grateful to the Medical Editors for editing the medical content. For further information please contact us at: Standards Unit Microbiology Services Public Health England 61 Colindale Avenue London NW9 5EQ E-mail: [email protected] Website: https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality- and-consistency-in-clinical-laboratories