Mushroom Poisoning Syndromes There Are Many Different Types of Mycotoxins
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abies Alba Mill.) Differ Largely in Mature Silver Fir Stands and in Scots Pine Forecrops Rafal Ważny
Ectomycorrhizal communities associated with silver fir seedlings (Abies alba Mill.) differ largely in mature silver fir stands and in Scots pine forecrops Rafal Ważny To cite this version: Rafal Ważny. Ectomycorrhizal communities associated with silver fir seedlings (Abies alba Mill.) differ largely in mature silver fir stands and in Scots pine forecrops. Annals of Forest Science, Springer Nature (since 2011)/EDP Science (until 2010), 2014, 71 (7), pp.801 - 810. 10.1007/s13595-014-0378-0. hal-01102886 HAL Id: hal-01102886 https://hal.archives-ouvertes.fr/hal-01102886 Submitted on 13 Jan 2015 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Annals of Forest Science (2014) 71:801–810 DOI 10.1007/s13595-014-0378-0 ORIGINAL PAPER Ectomycorrhizal communities associated with silver fir seedlings (Abies alba Mill.) differ largely in mature silver fir stands and in Scots pine forecrops Rafał Ważny Received: 28 August 2013 /Accepted: 14 April 2014 /Published online: 14 May 2014 # The Author(s) 2014. This article is published with open access at Springerlink.com Abstract colonization of seedling roots was similar in both cases. This & Context The requirement for rebuilding forecrop stands suggests that pine stands afforested on formerly arable land besides replacement of meadow vegetation with forest plants bear enough ECM species to allow survival and growth of and formation of soil humus is the presence of a compatible silver fir seedlings. -

Molecular Phylogenetic Studies in the Genus Amanita
1170 Molecular phylogenetic studies in the genus Amanita I5ichael Weiß, Zhu-Liang Yang, and Franz Oberwinkler Abstracl A group of 49 Amanita species that had been thoroughly examined morphologically and amtomically was analyzed by DNA sequence compadson to estimate natural groups and phylogenetic rclationships within the genus. Nuclear DNA sequences coding for a part of the ribosomal large subunit were determined and evaluated using neighbor-joining with bootstrap analysis, parsimony analysis, conditional clustering, and maximum likelihood methods, Sections Amanita, Caesarea, Vaginatae, Validae, Phalloideae, and Amidella were substantially confirmed as monophyletic groups, while the monophyly of section Lepidell.t remained unclear. Branching topologies between and within sections could also pafiially be derived. Stbgenera Amanita an'd Lepidella were not supported. The Mappae group was included in section Validae. Grouping hypotheses obtained by DNA analyses are discussed in relation to the distribution of morphological and anatomical chamcters in the studied species. Key words: fungi, basidiomycetes phylogeny, Agarrcales, Amanita systematics, large subunit rDNA, 28S. R6sum6 : A partir d'un groupe de 49 esp,ces d'Amanita prdalablement examinees morphologiquement et anatomiquement, les auteurs ont utilisd la comparaison des s€quences d'ADN pour ddfinir les groupes naturels et les relations phylog6ndtiques de ce genre. Les sdquences de I'ADN nucl6aire codant pour une partie de la grande sous-unit6 ribosomale ont 6t6 ddterminEes et €valu6es en utilisant l'analyse par liaison en lacet avec le voisin (neighbor-joining with bootstrap), l'analyse en parcimonie, le rcgroupement conditionnel et les m€thodes de ressemblance maximale. Les rdsultats confirment substantiellement les sections Afiarira, Caesarea, Uaqinatae, Ualidae, Phalloideae et Amidella, comme groupes monophyldtiques, alors que la monophylie de la section Lepidella demerxe obscure. -
Annotated Check List and Host Index Arizona Wood
Annotated Check List and Host Index for Arizona Wood-Rotting Fungi Item Type text; Book Authors Gilbertson, R. L.; Martin, K. J.; Lindsey, J. P. Publisher College of Agriculture, University of Arizona (Tucson, AZ) Rights Copyright © Arizona Board of Regents. The University of Arizona. Download date 28/09/2021 02:18:59 Link to Item http://hdl.handle.net/10150/602154 Annotated Check List and Host Index for Arizona Wood - Rotting Fungi Technical Bulletin 209 Agricultural Experiment Station The University of Arizona Tucson AÏfJ\fOTA TED CHECK LI5T aid HOST INDEX ford ARIZONA WOOD- ROTTlNg FUNGI /. L. GILßERTSON K.T IyIARTiN Z J. P, LINDSEY3 PRDFE550I of PLANT PATHOLOgY 2GRADUATE ASSISTANT in I?ESEARCI-4 36FZADAATE A5 S /STANT'" TEACHING Z z l'9 FR5 1974- INTRODUCTION flora similar to that of the Gulf Coast and the southeastern United States is found. Here the major tree species include hardwoods such as Arizona is characterized by a wide variety of Arizona sycamore, Arizona black walnut, oaks, ecological zones from Sonoran Desert to alpine velvet ash, Fremont cottonwood, willows, and tundra. This environmental diversity has resulted mesquite. Some conifers, including Chihuahua pine, in a rich flora of woody plants in the state. De- Apache pine, pinyons, junipers, and Arizona cypress tailed accounts of the vegetation of Arizona have also occur in association with these hardwoods. appeared in a number of publications, including Arizona fungi typical of the southeastern flora those of Benson and Darrow (1954), Nichol (1952), include Fomitopsis ulmaria, Donkia pulcherrima, Kearney and Peebles (1969), Shreve and Wiggins Tyromyces palustris, Lopharia crassa, Inonotus (1964), Lowe (1972), and Hastings et al. -

The Mycophile 52:2 March/April 2012
VOLUME 52:2 March-April 2012 www.namyco.org PRESIDENT’S MESSAGE by Bob Fulgency I am pleased to report that outstanding west coast in food establishments.” The growing problem of safety mycologist Dr. Tom Bruns has accepted an invitaon to associated with the unregulated sale of wild mushroom become a NAMA Ins:tu:onal Trustee. Tom is a to the public was what generated CFP’s interest. professor and associate chair at the Department of Plant and Microbial Biology at the University of California, The Commi`ee’s plan is to develop a blueprint that Berkeley, and he is a past president of the Mycological regulatory agencies can follow to allow them to exercise Society of America. He received an M.S. from the meaningful control over all facets of wild mushroom University of Minnesota and a Ph.D. from the University harves:ng and distribu:on. At this :me, the Commi`ee of Michigan. He has published over 120 ar:cles on fungal intends to submit five recommendaons to CFP for ecology and evolu:on and is best known for his work of consideraon. Of par:cular interest is the training of ectomycorrhizal communi:es. I know Tom will make approved mushroom iden:fiers. Based on this plan, each important contribu:ons to NAMA's ongoing mission of state or region will be expected to develop a list of suppor:ng the scien:fic study of fungi. mushrooms that can be collected in the area. Further, it will be responsible for training candidates and Issues surrounding regulatory oversight of wild subsequently test them for their knowledge of wild mushroom harves:ng and sale s:ll linger. -

Key Features for the Identification of the Fungi in This Guide
Further information Key features for the identifi cation Saprotrophic recycler fungi Books and References of the fungi in this guide Mushrooms. Roger Phillips (2006). Growth form. Fungi come in many different shapes and Fruit body colours. The different parts of the fruit body Collybia acervata Conifer Toughshank. Cap max. 5cm. Macmillan. Excellent photographs and descriptions including sizes. In this fi eld guide most species are the classic can be differently coloured and it is also important This species grows in large clusters often on the ground many species from pinewoods and other habitats. toadstool shape with a cap and stem but also included to remember that the caps sometimes change colour but possibly growing on buried wood. Sometimes there are are some that grow out of wood like small shelves or completely or as they dry out. Making notes or taking Fungi. Roy Watling and Stephen Ward (2003). several clusters growing ± in a ring. The caps are reddish brackets and others that have a coral- like shape. Take photographs can help you remember what they looked Naturally Scottish Series. Scottish Natural Heritage, Battleby, Perth. brown but dry out to a buff colour. The stems are smooth, note of whether the fungus is growing alone, trooping like when fresh. In some fungi the fl esh changes colour Good introduction to fungi in Scotland. and red brown and the gills are white and variably attached, or in a cluster. when it is damaged. Try cutting the fungus in half or Fungi. Brian Spooner and Peter Roberts (2005). adnate to free. Spore print white. -

Pt Reyes Species As of 12-1-2017 Abortiporus Biennis Agaricus
Pt Reyes Species as of 12-1-2017 Abortiporus biennis Agaricus augustus Agaricus bernardii Agaricus californicus Agaricus campestris Agaricus cupreobrunneus Agaricus diminutivus Agaricus hondensis Agaricus lilaceps Agaricus praeclaresquamosus Agaricus rutilescens Agaricus silvicola Agaricus subrutilescens Agaricus xanthodermus Agrocybe pediades Agrocybe praecox Alboleptonia sericella Aleuria aurantia Alnicola sp. Amanita aprica Amanita augusta Amanita breckonii Amanita calyptratoides Amanita constricta Amanita gemmata Amanita gemmata var. exannulata Amanita calyptraderma Amanita calyptraderma (white form) Amanita magniverrucata Amanita muscaria Amanita novinupta Amanita ocreata Amanita pachycolea Amanita pantherina Amanita phalloides Amanita porphyria Amanita protecta Amanita velosa Amanita smithiana Amaurodon sp. nova Amphinema byssoides gr. Annulohypoxylon thouarsianum Anthrocobia melaloma Antrodia heteromorpha Aphanobasidium pseudotsugae Armillaria gallica Armillaria mellea Armillaria nabsnona Arrhenia epichysium Pt Reyes Species as of 12-1-2017 Arrhenia retiruga Ascobolus sp. Ascocoryne sarcoides Astraeus hygrometricus Auricularia auricula Auriscalpium vulgare Baeospora myosura Balsamia cf. magnata Bisporella citrina Bjerkandera adusta Boidinia propinqua Bolbitius vitellinus Suillellus (Boletus) amygdalinus Rubroboleus (Boletus) eastwoodiae Boletus edulis Boletus fibrillosus Botryobasidium longisporum Botryobasidium sp. Botryobasidium vagum Bovista dermoxantha Bovista pila Bovista plumbea Bulgaria inquinans Byssocorticium californicum -

Catalogue No. 121 – Sale, Special Offers and Recent Acquisitions
C. Arden, Bookseller Darren Bloodworth The Nursery, Forest Road, Hay-on-Wye, HR3 5DT, U.K. Tel: +44 (0) 1497-820471 Email: [email protected] Web: www.ardenbooks.co.uk Catalogue No. 121 – Sale, Special Offers and Recent Acquisitions Sale items : Botany 1 - 112 Entomology 113 - 140 Fine, Illustrated & Antiquarian 141 - 151 Gardening 152 - 207 General 208 - 254 Natural History & Zoology 255 - 266 New Naturalist s 267 - 302 Ornithology 303 - 346 Special offers : Botany 347 - 404 and recent Entomology 405 - 440 acquisitions Fine, Illustrated & Antiquarian 441 - 458 Gardening 459 - 512 Natural History & Zoology 513 - 562 New Naturalists 563 - 611 Ornithology 612 - 688 The stock in the Sale part of this catalogue (items 1 to 346) is an attempt to clear the remains of stock from the year’s previous catalogues. Book prices have already been reduced in many cases and further reductions are available to those who wish to take a risk that their chosen books will be available 10 or even 20 days after receiving this catalogue. Books will be dispatched once orders are complete – this may take up to three weeks if you order books at 50% off. How the Sale works First 10 days of sale…….All books available at prices shown in the catalogue After 10 days……………..If books are still available, we reduce their prices by 25% After 20 days……………..If books are still available, we reduce their prices by 50% We have also included over three hundred Special offers and recent acquisitions at the end of the catalogue (items 347 to 688). These Special offers and recent acquisitions are available at the prices indicated and are not part of the Sale terms. -

Forest Fungi in Ireland
FOREST FUNGI IN IRELAND PAUL DOWDING and LOUIS SMITH COFORD, National Council for Forest Research and Development Arena House Arena Road Sandyford Dublin 18 Ireland Tel: + 353 1 2130725 Fax: + 353 1 2130611 © COFORD 2008 First published in 2008 by COFORD, National Council for Forest Research and Development, Dublin, Ireland. All rights reserved. No part of this publication may be reproduced, or stored in a retrieval system or transmitted in any form or by any means, electronic, electrostatic, magnetic tape, mechanical, photocopying recording or otherwise, without prior permission in writing from COFORD. All photographs and illustrations are the copyright of the authors unless otherwise indicated. ISBN 1 902696 62 X Title: Forest fungi in Ireland. Authors: Paul Dowding and Louis Smith Citation: Dowding, P. and Smith, L. 2008. Forest fungi in Ireland. COFORD, Dublin. The views and opinions expressed in this publication belong to the authors alone and do not necessarily reflect those of COFORD. i CONTENTS Foreword..................................................................................................................v Réamhfhocal...........................................................................................................vi Preface ....................................................................................................................vii Réamhrá................................................................................................................viii Acknowledgements...............................................................................................ix -

The Bioaccumulation of Some Heavy Metals in the Fruiting Body of Wild Growing Mushrooms
Available online at www.notulaebotanicae.ro Print ISSN 0255-965X; Electronic 1842-4309 Not. Bot. Hort. Agrobot. Cluj 38 (2) 2010, Special Issue, 147-151 Notulae Botanicae Horti Agrobotanici Cluj-Napoca The Bioaccumulation of Some Heavy Metals in the Fruiting Body of Wild Growing Mushrooms Carmen Cristina ELEKES1) , Gabriela BUSUIOC1) , Gheorghe IONITA 2) 1) Valahia University of Targoviste, Faculty of Environmental Engineering and Biotechnologies, Bd. Regele Carol I, no. 2, Romania; [email protected] 2) Valahia University of Targoviste, Faculty of Materials Engineering, Mechatronics and Robotics, Bd. Regele Carol I, no. 2, Romania Abstract Due to their effective mechanism of accumulation of heavy metals from soil, the macrofungi show high concentrations of metals in their fruiting body. According with this ability, the mushrooms can be used to evaluate and control the level of environmental pollution, but also represent danger for human ingestion. We analyzed some macrofungi species from a wooded area to establish the heavy metal concentrations and ability of bioaccumulation and translocation for Zn, Cu and Sn in fruiting body. The metallic content was established by the Inductively Coupled Plasma-Atomic Emission Spectrometry method (ICP-AES). The minimal detection limits of method is 0.4 mg/kg for Zn and Cu and 0.6 mg/kg for Sn. Heavy metals concentrations in the fruiting body ranged between 6.98- 20.10 mg/kg for Zn (the higher value was for Tapinella atrotomentosa); 16.13-144.94 mg/kg for Cu (the higher value was for Hypholoma fasciculare); and 24.36-150.85 mg/kg for Sn (the higher value was for Paxillus involutus). -

The Ectomycorrhizal Fungus Amanita Phalloides Was Introduced and Is
Molecular Ecology (2009) doi: 10.1111/j.1365-294X.2008.04030.x TheBlackwell Publishing Ltd ectomycorrhizal fungus Amanita phalloides was introduced and is expanding its range on the west coast of North America ANNE PRINGLE,* RACHEL I. ADAMS,† HUGH B. CROSS* and THOMAS D. BRUNS‡ *Department of Organismic and Evolutionary Biology, Biological Laboratories, 16 Divinity Avenue, Harvard University, Cambridge, MA 02138, USA, †Department of Biological Sciences, Gilbert Hall, Stanford University, Stanford, CA 94305-5020, USA, ‡Department of Plant and Microbial Biology, 111 Koshland Hall, University of California, Berkeley, CA 94720, USA Abstract The deadly poisonous Amanita phalloides is common along the west coast of North America. Death cap mushrooms are especially abundant in habitats around the San Francisco Bay, California, but the species grows as far south as Los Angeles County and north to Vancouver Island, Canada. At different times, various authors have considered the species as either native or introduced, and the question of whether A. phalloides is an invasive species remains unanswered. We developed four novel loci and used these in combination with the EF1α and IGS loci to explore the phylogeography of the species. The data provide strong evidence for a European origin of North American populations. Genetic diversity is generally greater in European vs. North American populations, suggestive of a genetic bottleneck; polymorphic sites of at least two loci are only polymorphic within Europe although the number of individuals sampled from Europe was half the number sampled from North America. Endemic alleles are not a feature of North American populations, although alleles unique to different parts of Europe were common and were discovered in Scandinavian, mainland French, and Corsican individuals. -

615.9Barref.Pdf
INDEX Abortifacient, abortifacients bees, wasps, and ants ginkgo, 492 aconite, 737 epinephrine, 963 ginseng, 500 barbados nut, 829 blister beetles goldenseal blister beetles, 972 cantharidin, 974 berberine, 506 blue cohosh, 395 buckeye hawthorn, 512 camphor, 407, 408 ~-escin, 884 hypericum extract, 602-603 cantharides, 974 calamus inky cap and coprine toxicity cantharidin, 974 ~-asarone, 405 coprine, 295 colocynth, 443 camphor, 409-411 ethanol, 296 common oleander, 847, 850 cascara, 416-417 isoxazole-containing mushrooms dogbane, 849-850 catechols, 682 and pantherina syndrome, mistletoe, 794 castor bean 298-302 nutmeg, 67 ricin, 719, 721 jequirity bean and abrin, oduvan, 755 colchicine, 694-896, 698 730-731 pennyroyal, 563-565 clostridium perfringens, 115 jellyfish, 1088 pine thistle, 515 comfrey and other pyrrolizidine Jimsonweed and other belladonna rue, 579 containing plants alkaloids, 779, 781 slangkop, Burke's, red, Transvaal, pyrrolizidine alkaloids, 453 jin bu huan and 857 cyanogenic foods tetrahydropalmatine, 519 tansy, 614 amygdalin, 48 kaffir lily turpentine, 667 cyanogenic glycosides, 45 lycorine,711 yarrow, 624-625 prunasin, 48 kava, 528 yellow bird-of-paradise, 749 daffodils and other emetic bulbs Laetrile", 763 yellow oleander, 854 galanthamine, 704 lavender, 534 yew, 899 dogbane family and cardenolides licorice Abrin,729-731 common oleander, 849 glycyrrhetinic acid, 540 camphor yellow oleander, 855-856 limonene, 639 cinnamomin, 409 domoic acid, 214 rna huang ricin, 409, 723, 730 ephedra alkaloids, 547 ephedra alkaloids, 548 Absorption, xvii erythrosine, 29 ephedrine, 547, 549 aloe vera, 380 garlic mayapple amatoxin-containing mushrooms S-allyl cysteine, 473 podophyllotoxin, 789 amatoxin poisoning, 273-275, gastrointestinal viruses milk thistle 279 viral gastroenteritis, 205 silibinin, 555 aspartame, 24 ginger, 485 mistletoe, 793 Medical Toxicology ofNatural Substances, by Donald G. -
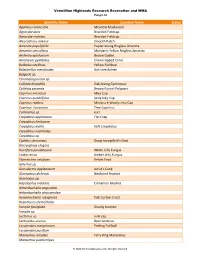
Scientific Name Common Name Status Agaricus Campestris
Vermillion Highlands Research Recreation and WMA Fungi List Scientific Name Common Name Status Agaricus campestris Meadow Mushroom Agrocybe dura Bearded Fieldcap Agrocybe molesta Bearded Fieldcap Aleurodiscus oakesii Smooth Patch Amanita populiphila Poplar-loving Ringless Amanita Amanita sinicoflava Mandarin Yellow Ringless Amanita Arrhenia epichysium Brown Goblet Artomyces pyxidatus Crown-tipped Coral Bolbitius vitellinus Yellow Fieldcap Boletinellus merulioides Ash-tree Bolete Bulgaria sp. Chromelosporium sp. Collybia dryophila Oak-loving Gymnopus Coltricia perennis Brown Funnel Polypore Coprinus micaceus Mica Cap Coprinus quadrifidus Scaly Inky Cap Coprinus radians Miniature Woolly Inky Cap Coprinus truncorum Tree Coprinus Cortinarius sp. cort Crepidotus applanatus Flat Crep Crepidotus herbarum Crepidotus mollis Soft Crepidotus Crepidotus nephrodes Crepidotus sp. Cyathus stercoreus Dung-loving Bird’s Nest Dacryopinax elegans Ductifera pululahuana White Jelly Fungus Exidia recisa Amber Jelly Fungus Flammulina velutipes Velvet Foot Galerina sp. Ganoderma applanatum Artist’s Conk Gloeoporus dichrous Bicolored Bracket Gymnopus sp. Hapalopilus nidulans Cinnamon Bracket Hohenbuehelia angustata Hohenbuehelia atrocaerulea Hymenochaete rubiginosa Oak Curtain Crust Hypomyces tremellicola Inocybe fastigiata Deadly Inocybe Inocybe sp. Lactarius sp. milk cap Lentinellus ursinus Bear Lentinus Lycoperdon marginatum Peeling Puffball Lycoperdon pusillum Marasmius oreades Fairy Ring Marasmius Marasmius pulcherripes © 2020 MinnesotaSeasons.com. All rights