Melanocytic Nevi and Melanoma: Unraveling a Complex Relationship
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Features of Benign Tumors of the External Auditory Canal According to Pathology
Central Annals of Otolaryngology and Rhinology Research Article *Corresponding author Jae-Jun Song, Department of Otorhinolaryngology – Head and Neck Surgery, Korea University College of Clinical Features of Benign Medicine, 148 Gurodong-ro, Guro-gu, Seoul, 152-703, South Korea, Tel: 82-2-2626-3191; Fax: 82-2-868-0475; Tumors of the External Auditory Email: Submitted: 31 March 2017 Accepted: 20 April 2017 Canal According to Pathology Published: 21 April 2017 ISSN: 2379-948X Jeong-Rok Kim, HwibinIm, Sung Won Chae, and Jae-Jun Song* Copyright Department of Otorhinolaryngology-Head and Neck Surgery, Korea University College © 2017 Song et al. of Medicine, South Korea OPEN ACCESS Abstract Keywords Background and Objectives: Benign tumors of the external auditory canal (EAC) • External auditory canal are rare among head and neck tumors. The aim of this study was to analyze the clinical • Benign tumor features of patients who underwent surgery for an EAC mass confirmed as a benign • Surgical excision lesion. • Recurrence • Infection Methods: This retrospective study involved 53 patients with external auditory tumors who received surgical treatment at Korea University, Guro Hospital. Medical records and evaluations over a 10-year period were examined for clinical characteristics and pathologic diagnoses. Results: The most common pathologic diagnoses were nevus (40%), osteoma (13%), and cholesteatoma (13%). Among the five pathologic subgroups based on the origin organ of the tumor, the most prevalent pathologic subgroup was the skin lesion (47%), followed by the epithelial lesion (26%), and the bony lesion (13%). No significant differences were found in recurrence rate, recurrence duration, sex, or affected side between pathologic diagnoses. -

CASE REPORT Intradermal Nevus of the External Auditory Canal
Int. Adv. Otol. 2009; 5:(3) 401-403 CASE REPORT Intradermal Nevus of the External Auditory Canal: A Case Report Sedat Ozturkcan, Ali Ekber, Riza Dundar, Filiz Gulustan, Demet Etit, Huseyin Katilmis Department of Otorhinolaryngology and Head and Neck Surgery ‹zmir Atatürk Research and Training Hospital, Ministry of Health, ‹ZM‹R-TURKEY (SO, AE, FG, DE, HK) Department of Otorhinolaryngology and Head and Neck Surgery Etimesgut Military Hospital , ANKARA-TURKEY (RD) Intradermal nevus is the most common skin tumor in humans; however, its occurrence in the external auditory canal (EAC) is uncommon. The clinical manifestations of pigmented nevus of the EAC have been reported to include ear fullness, foreign body sensation, hearing impairment, and otalgia, but some cases were asymptomatic and were found incidentally. The treatment of choice for a symptomatic intradermal nevus in the EAC is complete excision. There has been no recurrence reported in the literature . A pedunculated, papillomatous hair-bearing lesion was detected in the external auditory canal of the patient who was on follow-up for pruritus. Clinical and pathologic features of an intradermal nevus of the external auditory canal are presented, and the literature reviewed. Submitted : 14 October 2008 Revised : 01 July 2009 Accepted : 09 July 2009 Intradermal nevus is the most common skin tumor in left external auditory canal. Otomicroscopic humans; however, its occurrence in the external examination revealed a pedunculated, papillomatous auditory canal (EAC) is uncommon [1-4]. Intradermal hair-bearing lesion in the postero-inferior cartilaginous nevus is considered to be a form of benign cutaneous portion of the external auditory canal (Figure 1). -

Critical Evaluation of the So-Called “Junction Nevus”
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector CRITICAL EVALUATION OF THE SO-CALLED "JUNCTION NEVUS* S. WILLIAM BECKER, MS., M.D. The serious study of pigmented nevi was undertaken by many workers in the closing years of the 19th Century. All recognized that the microscopic picture of nevi differed from anything seen in other organs. The presence of nevus cells in both the epidermis and dermis led to concepts of origin at one or the other site, or at both sites. Dermal Origin: Demieville (1) believed that the nevus cells arose from adven- titial and endothelial cells of blood vessels. Bauer (2) and vonRecklinghausen (3) thought that the origin was from endothelium of lymph vessels rather than of blood vessels. Epidermal Origin: According to Abesser (4), Duranti, in 1871, was the first to suggest an epidermal origin of nevus cells. Kromayer (5) stated that the endo- thelium-like cells originate in the basal portion of the epidermis as "Bläschen- zellen", migrate to the dermis and develop connective tissue and elastic fibers, a change which he called "desmoplasia". Abesser (4) agreed that the cells origi- ated in the epithelium and lost their intercellular bridges, but migrated into the dermis as epithelium-like cells, and remained such. Unna (6) advanced the concept that the epithelial cells changed by losing their intercellular bridges and multiplied in groups, a process which he called "Ab- sonderung", then migrated as groups to the dermis, which he called "Abtrop- fung", thus forming pigmented nevi. -

Acral Compound Nevus SJ Yun S Korea
University of Pennsylvania, Founded by Ben Franklin in 1740 Disclosures Consultant for Myriad Genetics and for SciBase (might try to sell you a book, as well) Multidimensional Pathway Classification of Melanocytic Tumors WHO 4th Edition, 2018 Epidemiologic, Clinical, Histologic and Genomic Aspects of Melanoma David E. Elder, MB ChB, FRCPA University of Pennsylvania, Philadelphia, PA, USA Napa, May, 2018 3rd Edition, 2006 Malignant Melanoma • A malignant tumor of melanocytes • Not all melanomas are the same – variation in: – Epidemiology – risk factors, populations – Cell/Site of origin – Precursors – Clinical morphology – Microscopic morphology – Simulants – Genomic abnormalities Incidence of Melanoma D.M. Parkin et al. CSD/Site-Related Classification • Bastian’s CSD/Site-Related Classification (Taxonomy) of Melanoma – “The guiding principles for distinguishing taxa are genetic alterations that arise early during progression; clinical or histologic features of the primary tumor; characteristics of the host, such as age of onset, ethnicity, and skin type; and the role of environmental factors such as UV radiation.” Bastian 2015 Epithelium associated Site High UV Low UV Glabrous Mucosa Benign Acquired Spitz nevus nevus Atypical Dysplastic Spitz Borderline nevus tumor High Desmopl. Low-CSD Spitzoid Acral Mucosal Malignant CSD melanoma melanoma melanoma melanoma melanoma 105 Point mutations 103 Structural Rearrangements 2018 WHO Classification of Melanoma • Integrates Epidemiologic, Genomic, Clinical and Histopathologic Features • Assists -

Atypical Mole Syndrome and Dysplastic Nevi: Identification of Populations at Risk for Developing Melanoma - Review Article
CLINICS 2011;66(3):493-499 DOI:10.1590/S1807-59322011000300023 REVIEW Atypical mole syndrome and dysplastic nevi: identification of populations at risk for developing melanoma - review article Juliana Hypo´ lito Silva,I Bianca Costa Soares de Sa´,II Alexandre Leon Ribeiro de A´ vila,II Gilles Landman,III Joa˜ o Pedreira Duprat NetoII I Oncology School Celestino Bourroul - Hospital AC Camargo, Sa˜ o Paulo, SP, Brazil. II Skin Oncology Department - Hospital AC Camargo - Sa˜ o Paulo, SP, Brazil. III Pathology Department - Hospital AC Camargo - Sa˜ o Paulo, SP, Brazil. Atypical Mole Syndrome is the most important phenotypic risk factor for developing cutaneous melanoma, a malignancy that accounts for about 80% of deaths from skin cancer. Because the diagnosis of melanoma at an early stage is of great prognostic relevance, the identification of Atypical Mole Syndrome carriers is essential, as well as the creation of recommended preventative measures that must be taken by these patients. KEYWORDS: Dysplastic Nevus Syndrome; dysplastic nevi; melanoma; early diagnosis; Risk Factors. Silva JH, de Sa´ BC, Avila ALR, Landman G, Duprat Neto JP. Atypical mole syndrome and dysplastic nevi: identification of populations at risk for developing melanoma - review article. Clinics. 2011;66(3):493-499. Received for publication on November 23, 2010; First review completed on November 24, 2010; Accepted for publication on November 24, 2010 E-mail: [email protected] Tel.: 55 11 2189-5135 INTRODUCTION Several studies have shown that the presence of dysplas- tic nevi considerably increases the risk of developing The incidence of cutaneous melanoma has increased melanoma, which demonstrates that these lesions, aside rapidly worldwide.1-5 Although it corresponds to only 4% of 4 from being precursors to disease are also important risk all skin cancers, it accounts for 80% of skin cancer deaths. -
A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta)
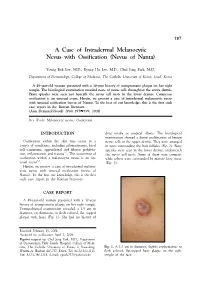
197 A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta) Young Bok Lee, M.D., Kyung Ho Lee, M.D., Chul Jong Park, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature. (Ann Dermatol (Seoul) 20(4) 197∼199, 2008) Key Words: Melanocytic nevus, Ossification INTRODUCTION drug intake or medical illness. The histological examination showed a dense proliferation of benign Ossification within the skin may occur in a nevus cells in the upper dermis. They were arranged variety of conditions, including pilomatricoma, basal in nests surrounding the hair follicles (Fig. 2). Bony cell carcinoma, appendageal and fibrous prolifera- spicules were seen in the lower dermis, underneath 1,2 tion, inflammation and trauma . The occurrence of the nevus cell nests. Some of them were compact ossification within a melanocytic nevus is an un- while others were surrounded by mature fatty tissue 3-5 usual event . (Fig. 3). Herein, we present a case of intradermal melano- cytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature. -

Digital Epiluminescence Microscopy Monitoring of High-Risk Patients
STUDY Digital Epiluminescence Microscopy Monitoring of High-Risk Patients June K. Robinson, MD; Brian J. Nickoloff, MD, PhD Objective: To examine the outcome of digital epilumi- dence in and comfort with dermatologic surveillance and nescence microscopic (DELM) surveillance of atypical skin self-examination performance were assessed. nevi in a high-risk population for 4 years. Results: During annual surveillance with DELM, 5.5% of Design: Atypical, flat melanocytic lesions in 100 pa- the lesions changed. Among the 193 excisional biopsy speci- tients at high risk of developing melanoma were fol- mens there were 4 melanomas in situ, 169 dysplastic nevi, lowed annually with DELM. Pigmentary changes or an and 20 common nevi. Confidence in and comfort with sur- increase in DELM diameter of 1 mm or greater was an veillance and skin self-examination improved after DELM. indication to perform an excisional biopsy. Conclusions: The criteria applied to detect substantial Setting: Cardinal Bernardin Cancer Center Melanoma DELM changes were an increase in DELM diameter of 1 Program, Loyola University Health System, Maywood. mm or greater and pigmentary changes, including ra- dial streaming, focal enlargement, peripheral black dots, Patients: A consecutive sample of 3482 lesions from 100 and “clumping” within the irregular pigment network. patients (aged 18-65 years) with at least 2 images of the Use of DELM enhanced confidence in and comfort with same lesion. care, which extended to performing more extensive skin self-examination. Main Outcome Measures: -

Case Report of Giant Congenital Melanocytic Nevus
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Bathing Trunks Nevus: Case Report of Giant Congenital Melanocytic Nevus Ronald Russ, DO; Lisa Light, MS-IV Bathing trunks nevi, a subtype of giant congeni- 34 years. All maternal and prenatal history was unre- tal melanocytic nevi (CMN), are skin tumors that markable. Upon initial physical examination as a new- present by 2 years of age and occur in a low born (1 hour following delivery), the infant had a large percentage of all births. We report a case of (≥5% body surface area), circumferentially pigmented bathing trunks nevus that was initially suspected area from the umbilicus to mid thigh bilaterally to be melanoma, and describe the history, patho- (Figure 1). Interposed darkened lesions were pres- physiology, and treatment options for CMN. We ent, with 3 distinct, raised, lipomatous-type nodules also discuss the risk for neurocutaneous melano- (2 cm, 1.3 cm, and 3 cm in diameter from left to right) sis (NCM), which is a rare syndrome in patients over the lower lumbar spine (Figure 2). There were no with giant CMN. signs of jaundice, hemolysis, meningomyelocele, or Cutis. 2009;83:69-72. abnormal hair growth. The rest of the physical exami- nation was unremarkable, including cardiovascular, pulmonary, and abdominal systems, and genitourinary athing trunks nevus is a specific subtype of functioning was normal. Cord blood testing revealed giant congenital melanocytic nevus (CMN) A Rh-positive blood type, and a direct Coombs test B with spread resembling bathing trunks. This was negative for antibodies. Complete blood cell rare variant is clinically significant because of the count was within reference range, with the excep- increased risk for progression to melanoma and its tion of a low platelet count of 2343103/µL (reference association with neurocutaneous melanosis (NCM).1 range, 250–4503103/µL). -

What Are Basal and Squamous Cell Skin Cancers?
cancer.org | 1.800.227.2345 About Basal and Squamous Cell Skin Cancer Overview If you have been diagnosed with basal or squamous cell skin cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Are Basal and Squamous Cell Skin Cancers? Research and Statistics See the latest estimates for new cases of basal and squamous cell skin cancer and deaths in the US and what research is currently being done. ● Key Statistics for Basal and Squamous Cell Skin Cancers ● What’s New in Basal and Squamous Cell Skin Cancer Research? What Are Basal and Squamous Cell Skin Cancers? Basal and squamous cell skin cancers are the most common types of skin cancer. They start in the top layer of skin (the epidermis), and are often related to sun exposure. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer cells. To learn more about cancer and how it starts and spreads, see What Is Cancer?1 Where do skin cancers start? Most skin cancers start in the top layer of skin, called the epidermis. There are 3 main types of cells in this layer: ● Squamous cells: These are flat cells in the upper (outer) part of the epidermis, which are constantly shed as new ones form. When these cells grow out of control, they can develop into squamous cell skin cancer (also called squamous cell carcinoma). -

Acral Melanoma Toshiaki Saida, Hiroshi Koga, Yoriko Yamazaki, Masaru Tanaka IV.2
Chapter IV.2 Acral Melanoma Toshiaki Saida, Hiroshi Koga, Yoriko Yamazaki, Masaru Tanaka IV.2 Contents thickness, biological behavior is not different among the four histogenetic types [16]. More- IV.2.1 Definition . .196 over, cutaneous melanomas not infrequently IV.2 IV.2.2 Clinical Features . .197 show overlapping histopathological features of IV2.3 Dermoscopic Criteria. 198 the four types [36]. Ackerman repeatedly criti- cized the validity of the Clark’s classification IV.2.4 Relevant Clinical Differential and proposed the unifying concept of melano- Diagnosis. 198 ma [1]. IV.2.5 Histopathology. .199 Recently, Bastian and co-workers defined ac- ral melanoma as melanoma occurring on the IV.2.6 Management. .200 non-hair-bearing skin of the palms or soles or IV.2.7 Case Study. .200 under the nails and found that this type of mel- References. .202 anoma was unique in frequent amplifications of chromosomes 5p15, 5p13, 11q13, and 12q14 [4, 7]. Particularly, amplification of 11q13 was de- tected in ~50% of this type of melanoma. Cyclin D1 is the most important candidate gene located in this chromosome region. It is noteworthy IV.2.1 Definition that 5 of 36 acral melanomas defined by Bastian and co-workers were superficial spreading mel- Acral melanoma is a melanoma that affects ac- anoma according to Clark’s classification [7]. ral areas of the skin, which is the most prevalent Another characteristic of acral melanoma is site of melanoma in non-Caucasians [5, 10]. very low rate of mutation of the BRAF onco- Strictly speaking, acral lentiginous melanoma is gene, which is commonly found in superficial not a synonym for acral melanoma. -

Melanomas Are Comprised of Multiple Biologically Distinct Categories
Melanomas are comprised of multiple biologically distinct categories, which differ in cell of origin, age of onset, clinical and histologic presentation, pattern of metastasis, ethnic distribution, causative role of UV radiation, predisposing germ line alterations, mutational processes, and patterns of somatic mutations. Neoplasms are initiated by gain of function mutations in one of several primary oncogenes, typically leading to benign melanocytic nevi with characteristic histologic features. The progression of nevi is restrained by multiple tumor suppressive mechanisms. Secondary genetic alterations override these barriers and promote intermediate or overtly malignant tumors along distinct progression trajectories. The current knowledge about pathogenesis, clinical, histological and genetic features of primary melanocytic neoplasms is reviewed and integrated into a taxonomic framework. THE MOLECULAR PATHOLOGY OF MELANOMA: AN INTEGRATED TAXONOMY OF MELANOCYTIC NEOPLASIA Boris C. Bastian Corresponding Author: Boris C. Bastian, M.D. Ph.D. Gerson & Barbara Bass Bakar Distinguished Professor of Cancer Biology Departments of Dermatology and Pathology University of California, San Francisco UCSF Cardiovascular Research Institute 555 Mission Bay Blvd South Box 3118, Room 252K San Francisco, CA 94158-9001 [email protected] Key words: Genetics Pathogenesis Classification Mutation Nevi Table of Contents Molecular pathogenesis of melanocytic neoplasia .................................................... 1 Classification of melanocytic neoplasms -

Thrombotic Thrombocytopenic Purpura Due to Checkpoint Inhibitors
Hindawi Case Reports in Hematology Volume 2018, Article ID 2464619, 4 pages https://doi.org/10.1155/2018/2464619 Case Report Thrombotic Thrombocytopenic Purpura due to Checkpoint Inhibitors Alexey Youssef,1 Nawara Kasso,2 Antonio Sergio Torloni,3 Michael Stanek,4 Tomislav Dragovich,5 Mark Gimbel,6 and Fade Mahmoud 6 1Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK 2Faculty of Medicine, Tishreen University, Lattakia, Syria 3Medical Director, Stem Cell )erapy, Apheresis, and Transfusion Medicine, Banner MD Anderson Cancer Center, Gilbert, AZ, USA 4Division of Hematology, Banner MD Anderson Cancer Center, Gilbert, AZ, USA 5Chief, Division of Medical Oncology and Hematology, Banner MD Anderson Cancer Center, Gilbert, AZ, USA 6)e T.W. Lewis Melanoma Center of Excellence, Banner MD Anderson Cancer Center, Gilbert, AZ, USA Correspondence should be addressed to Fade Mahmoud; [email protected] Received 16 September 2018; Revised 23 November 2018; Accepted 28 November 2018; Published 20 December 2018 Academic Editor: Akimichi Ohsaka Copyright © 2018 Alexey Youssef et al. ,is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Ipilimumab is a monoclonal antibody that enhances the efficacy of the immune system by targeting a cytotoxic T-lymphocyte- associated protein 4 (CTLA-4), which is a protein receptor that downregulates the immune system. Nivolumab is also a hu- manized monoclonal antibody that targets another protein receptor that prevents activated T cells from attacking the cancer; this receptor is called programmed cell death 1 (PD-1).