Intermountain Dixie Regional Medical Center Community Health Needs Assessment 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Life and Contributions of Lee Hafen to Athletics at Dixie College
Utah State University DigitalCommons@USU All Graduate Theses and Dissertations Graduate Studies 5-1968 The Life and Contributions of Lee Hafen to Athletics at Dixie College Douglas V. Allred Utah State University Follow this and additional works at: https://digitalcommons.usu.edu/etd Part of the Education Commons Recommended Citation Allred, Douglas V., "The Life and Contributions of Lee Hafen to Athletics at Dixie College" (1968). All Graduate Theses and Dissertations. 2858. https://digitalcommons.usu.edu/etd/2858 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@USU. It has been accepted for inclusion in All Graduate Theses and Dissertations by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. THE LIFE AND CONTRIBUTIONS OF LEE HAFE TO ATHLETICS AT DIXIE COLLEGE by Douglas V. Allred A thesis submitted in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in Physical Education Alproved: UTAH STATE UNIVERSITY Logan, Utah 1968 Figure 1. Coach Leland Hafen (Born September 1, 1895, Died November 23, 1959). ACKNOWLEDGMENTS The writer wishes to express his grateful appreciation to the Thesis Chairman, Professor H. B. Hunsaker, for his help and guidance. I am grateful to the Committee Members: Professor s John Pennock, Dale Rasmussen also to Dr. Lincoln McClellan for their suggestions. Sincere appreciation is expressed to Clark Hafen and Mrs. Edna Gregerson for their constructive criticism. Finally, to my wife, Elaine, the writer expr esses a husband's appreciation for the many hours spent in 1yping and for her patienc e and encouragement to complete this study Douglas Vance Allred TABLE OF CONTENTS Page ACKNOWLEDGMENTS iii LIST OF TABLES ·v LIST OF FIGURES Vi' ABSTRACT v ii INTRODUCTION Chapter I. -

David and Dixie Harvey V. City of Cedar Hills : Brief of Appellee Utah Court of Appeals
Brigham Young University Law School BYU Law Digital Commons Utah Court of Appeals Briefs 2008 David and Dixie Harvey v. City of Cedar Hills : Brief of Appellee Utah Court of Appeals Follow this and additional works at: https://digitalcommons.law.byu.edu/byu_ca3 Part of the Law Commons Original Brief Submitted to the Utah Court of Appeals; digitized by the Howard W. Hunter Law Library, J. Reuben Clark Law School, Brigham Young University, Provo, Utah; machine-generated OCR, may contain errors. Eric Todd Johnson; R. Christopher Preston; Kyle Fielding; Smith Hartvigsen, PLLC; Attorneys for Appellees. Gordon Duval; Duval Haws and Moody, P.C.; Attorneys for Appellants. Recommended Citation Brief of Appellee, Harvey v. Cedar Hills, No. 20080586 (Utah Court of Appeals, 2008). https://digitalcommons.law.byu.edu/byu_ca3/1035 This Brief of Appellee is brought to you for free and open access by BYU Law Digital Commons. It has been accepted for inclusion in Utah Court of Appeals Briefs by an authorized administrator of BYU Law Digital Commons. Policies regarding these Utah briefs are available at http://digitalcommons.law.byu.edu/utah_court_briefs/policies.html. Please contact the Repository Manager at [email protected] with questions or feedback. IN THE UTAH COURT OF APPEALS IN THE MATTER OF THE DISCONNECTION OF TERRITORY FROM THE CITY OF CEDAR HILLS BRIEF OF APPELLEE DAVID and DIXIE HARVEY, Appellate Case No. 20080586-CA Petitioners/Appellants, v. CITY OF CEDAR HILLS Respondent/Appellee. Appeal from the Order of the Fourth Judicial District, Utah County, State of Utah, The Honorable James R. Taylor, Presiding Gordon Duval Eric Todd Johnson (No.06901) Duval Haws and Moody, P.C. -

2018 Dixie State Men's Soccer Roster
2018 Dixie State Men’s Soccer Roster # NAME Yr. Pos. Ht. Wt. HOMETOWN/PREVIOUS SCHOOL(S) 0 Levi Lord So. GK 6-2 160 Las Vegas, Nev./Palo Verde HS 1 Zach Nielson R-Jr. GK 6-2 175 West Point, Utah/Northridge HS 2 Gustavo Ortega R-Jr. F 5-8 165 Las Vegas, Nev./Cimarron Memorial HS 3 Daniel Brubaker Fr. F 5-8 143 Hurricane, Utah/Hurricane HS 4 Hudson Ashcraft Fr. D 6-1 174 Long Beach, Calif./Wilson Classical HS 5 Ricky Nunez Jr. D 5-9 170 Henderson, Nev./Green Valley HS/Yavapai CC 6 Enrique Bucio R-Jr. MF 5-6 140 Silt, Colo./Coal Ridge HS 7 Moises Medina Jr. F 6-0 165 Mesquite, Nev./Virgin Valley HS 8 Cole Shaffer Fr. MF 5-9 150 Murrieta, Calif./Vista Murrieta HS 9 Dresden Quackenbush Fr. F 5-10 175 Las Vegas, Nev./West Career and Technical Acad. 10 Dominic Damato Sr. MF 5-8 170 Las Vegas, Nevada/Shadow Ridge HS 11 Jandir Porta Jr. MF 5-6 143 West Valley City, Utah/Hunter HS 13 Kaleb Schultz R-Jr. D 6-0 180 Crested Butte, Colo./Crested Butte HS/Otero JC 14 Zach Beckman Sr. MF 5-8 185 Centerville, Utah/Viewmont HS 15 Giancarlo Castillo Fr. MF 5-8 150 West Jordan, Utah/Copper Hills HS 17 Julius Nguyen Fr. MF 5-5 125 Seattle, Wash./John F. Kennedy Catholic HS 18 Ricardo Villa R-So. MF 5-8 148 Somerton, Ariz./Kofa HS 19 Zac McCulloch Sr. D 5-11 175 Draper, Utah/Alta HS/Southern Virginia 20 Ascari Robles R-Sr. -
2019 Annual Report
President & CEO Message After my first complete year as President & CEO, I can safely say I am immensely proud of the work we do, and the way we do it, to feed the 374,000 Utahns facing hunger. With an amazing staff, aided by an army of volunteers, and the support of our community, we distributed 45.7 million pounds of food last year. That's 38 million meals! It was the highest distribution year in our 115-year history, a milestone that’s hard to celebrate when the number of food-insecure Utahns had been declining in the past few years. This indicates that while there may be fewer Utahns facing hunger, they are needing more help, and for longer periods of Ginette Bott President & CEO time, than before. The growth and success of our Mobile School Pantry program in recent years has been remarkable. At the same time, it uncovered an unexpected need—the lack of resources at some of our local schools is so great that food needs to be available to students and their families every day. To that end, we expanded our in-school pantry program, which is now offered in 23 local schools and universities. Adding in-school pantries has enabled us to expand our Mobile School Pantry program, adding new locations in Utah and Washington Counties, which raised our total to 69 sites. Kent Liston 2019 also brought with it a federal government shutdown. This crisis was unlike any we had seen in recent Chief Financial Officer history. It shone a light on the many Americans struggling to keep afloat, with millions just one financial setback away from disaster. -

Utah Public Art Program & Dixie State University
Utah public Art Program & Dixie State University Health Sciences & Human Performance Center St. George, Utah Call for artist’s qualifications to create public art for the Dixie State University – Human Performance Center St. George, Utah Deadline for Submission: August 3, 2018 Letters of interest and qualifications are requested from artists interested in creating site specific art for the public area(s) of the new Dixie State University Human Performance Center in St. George, Utah. Dixie State University Human Performance Center The new Dixie State University Human Performance Center is an innovative combination of three major campus functions: academics, recreation and athletics. Dixie State envisions the new facility as an iconic landmark serving as a gateway for the west entry of campus. At approximately 155,000 square feet, the center provides extensive opportunities for recreation, activity and interdisciplinary academic programs for the University and the St. George community. The Human Performance Center includes classrooms, teaching labs, office and administration space, conference rooms, an Olympic-size competition pool/natatorium with an elevated spectator seating area, full-service fitness center with three multipurpose rooms, indoor and outdoor/rooftop basketball courts, indoor and outdoor running track, 65-foot climbing wall, 12-foot bouldering wall, nutrition bar and lounge, and an exterior plaza with gas-fueled fire pit. DSU College of Health Sciences https://health.dixie.edu/ The mission of the Dixie State University College of Health Sciences is to prepare students for employment in healthcare settings, service to the community, and lifelong learning. The vision is to contribute to excellence in healthcare by inspiring future healthcare providers to lead by example; seek further knowledge; and passionately advocate for all patients, communities, and populations. -

John Carbaugh and Dixie Carbaugh V. Asbestos Corporation Limited, Et Al : Reply Brief Utah Court of Appeals
Brigham Young University Law School BYU Law Digital Commons Utah Court of Appeals Briefs 2005 John Carbaugh and Dixie Carbaugh v. Asbestos Corporation Limited, et al : Reply Brief Utah Court of Appeals Follow this and additional works at: https://digitalcommons.law.byu.edu/byu_ca2 Part of the Law Commons Original Brief Submitted to the Utah Court of Appeals; digitized by the Howard W. Hunter Law Library, J. Reuben Clark Law School, Brigham Young University, Provo, Utah; machine-generated OCR, may contain errors. unknown. S. Brook Millard; Courtney G. Broaden; Brayton, Purcell, Eisenberg, Gilchrist & Morton. Recommended Citation Reply Brief, Carbaugh v. Asbestos Corp, No. 20050822 (Utah Court of Appeals, 2005). https://digitalcommons.law.byu.edu/byu_ca2/6037 This Reply Brief is brought to you for free and open access by BYU Law Digital Commons. It has been accepted for inclusion in Utah Court of Appeals Briefs by an authorized administrator of BYU Law Digital Commons. Policies regarding these Utah briefs are available at http://digitalcommons.law.byu.edu/utah_court_briefs/policies.html. Please contact the Repository Manager at [email protected] with questions or feedback. IN THE SUPREME COURT OF UTAH JOHN CARBAUGH and REPLY BRIEF OF THE APPELLANT DIXIE CARBAUGH, Plaintiff/ Appellant, vs. Supreme Court Case No.: 20050822-SC ASBESTOS CORPORATION LIMITED, et al., Civil No.:010910746 AS Master Case No. 010900863 AS Defendants/ Appellee. APPEAL FROM A FINAL JUDGEMENT OF THE THIRD JUDICIAL DISTRICT COURT OF SALT LAKE COUNTY, STATE OF UTAH JUDGE GLENN K. IWASAKI S. BROOK MILLARD (#7415) COURTNEY G. BROADEN (#10913) BRAYTON •> PURCELL SEE FOLLOWING PAGE FOR EISENBERG, GILCHRIST & DEFENDANT PARTIES MORTON 215 South State Street, Suite 900 Salt Lake City, Utah 84111 Telephone: (801) 366-9100 FILED UTAH APPELLATE COURTS JUL 0 3 2006 IN THE SUPREME COURT OF UTAH JOHN CARBAUGH and REPLY BRIEF OF THE APPELLANT DIXIE CARBAUGH, Plaintiff/Appellant, vs. -

City of St. George Active Transportation Plan
City of St. George Active Transportation Plan JANUARY 2017 Table of Contents PROJECT STEERING COMMITTEES & CONSULTANT TEAM: Vision & Goals 1: Introduction . 1. About the Plan ..................................................................1 About St. George .............................................................1 ST. GEORGE ACTIVE TRANSPORTATION COMMITTEE Why Walking & Bicycling Matters ................................2 Cimarron Chacon, Event Organizer 2: Existing Conditions & Needs Analysis . 7. Craig Shanklin, SUBA & Healthy Dixie Council Walking & Bicycling Trends ............................................7 Eric Martin, Business Owner Connectivity to Transit................................................. 11 Jordan Merrill, SW Utah Public Health Department Natural Obstacles to Bicycling and Walking .......... 12 Karen Bess, Washington Co. School Dist. Existing System Analysis ............................................. 13 Kye Nordfelt, SW Utah Public Health Department Crashes ............................................................................ 15 Kyle Wells, Dixie State University Needs, Gaps, Opportunities, & Constraints.......... 19 Launi Schmutz-Harden, Washington Co. School Dist. Existing Plans & Studies .............................................. 21 Mark McLaughlin, Owner of Bicycles Unlimited 3: Public Involvement . 27 Mitch Cloward, Dixie Regional Medical Center Field Investigation Bike Ride ...................................... 27 Rachel Cieslewicz, Business Owner Interactive Online Mapping Tool ............................. -

Dixie National Forest Visitor Guide
ixie National Forest VISITOR GUIDE A Contrast in Color, Climate, & Culture Pine Valley Reservoir Red Canyon What’s Inside place of diversity, the Dixie National Forest straddles the divide between the Great Basin and the Colorado History .................................. 2 Scenic Byways, A River in southern Utah. Scenery ranges from desert Backways, & Drives ............. 3 canyon gorges of amber, rose, and sienna to high Special Places ..................... 4 mountain forests, plateaus, and alpine lakes. Our Natural Resources ........ 6 Map ....................................... 8 Campgrounds & Guard Station Rentals ....... 10 Fast Forest Facts he Dixie National Trails .................................... 11 TForest is characterized by Activities .............................. 12 contrast. As a part of the Know Before You Go............ 14 Elevation Range: 3,000’–11,000’ Contact Information ............ 16 world-renowned landscapes Acres: Nearly 2 million of Southern Utah, the forest provides a backdrop and serves as a gateway to The Name: Southwest Utah was called Utah’s Dixie by early settlers from the surrounding National Parks and Monuments. southern states sent to the desert to Nationally recognized highways and trails grow cotton and silk; the forest was course through the forest and provide named after the area. ready access to the distinctive natural Temperature Range: From mountain highlights of the forest landscape. lows of -30 degrees to valley highs of over 100 degrees Fahrenheit. Come see for yourself! Sego Lily This Visitor Guide provides the information you can use to plan your trip to the Dixie National Forest. G et to Know Us History What is now the Dixie National Forest was once orested lands in inhabited by the Paleo-Indian Culture who hunted woolly FSouthern Utah are vital mammoths and megafauna. -

A Century of Dixie State College by Douglas D
THE JUANITA BROOKS LECTURE SERIES presents The 28th Annual Lecture A Century of Dixie State College by Douglas D. Alder St. George Tabernacle March 23, 2011 7:00 P.M. Co-sponsored by Val Browning Library, Dixie State College St. George, Utah and the Obert C. Tanner Foundation This is blank Juanita Brooks was a professor at [then] Dixie College for many years and became a well-known author. She is recognized, by scholarly consent, to be one of Utah’s and Mormondom’s most eminent historians. Her total honesty, unwavering courage, and perceptive interpretation of fact set more stringent standards of scholarship for her fellow historians to emulate. Dr. Obert C. and Grace Tanner had been lifelong friends of Mrs. Brooks and it was their wish to perpetuate her name through this lecture series. Dixie State College and the Brooks family express their thanks to the Tanner family. Copyright 2011, Dixie State College of Utah St. George, Utah 84770 All rights reserved The author, Douglas D. Alder, received B.A. and M.A. degrees from the University of Utah in 1957 and 1959. His Ph.D. is from the University of Oregon, 1966. He did his research for his doctoral dissertation on a Fulbright Fellowship in Vienna, Austria. He taught European History at Utah State University from 1963 to 1986. Then he was appointed president of Dixie College, serving until 1993. He remained at Dixie after his presidency, teaching history full-time until 1999. From 2002 to 2009 he was an adjunct professor there. Since then he has been doing historical research and writing. -
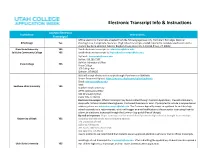
Electronic Transcript Info & Instructions
Electronic Transcript Info & Instructions Accepts Electronic Institution Instructions Transcripts? Official electronic transcripts accepted from the following agencies only: Parchment Exchange, National BYU/Ensign Yes Clearinghouse, Escript Safe, Naviance. High School transcripts are not required to complete application until a student has Been admitted. Mail to: Brigham Young University A-41 ASB Provo, UT. 84602 Dixie State University YES Email electronic transcripts to: [email protected]. Salt Lake Community College YES Email electronic transcripts to: [email protected]. By Email: [email protected] By Fax: 435.283.7157 By Mail: Admissions Office Snow College YES Snow College 150 College Ave Ephraim, UT 84627 SUU will accept electronic transcript through: Parchment or SENDedu Secure Document Upload: https://my.suu.edu/secure/upload/adminfo Email: [email protected] Mail: Southern Utah University YES Southern Utah University ATTN: Admissions Office 351 W University Blvd. Cedar City, UT 84721 Electronic transcripts: Official transcripts may be submitted through Common Application, Credential Solutions, eScip-Safe, National Student Clearinghouse, Parchment/Naviance or Scoir. If prompted to include a recipient email address, please use [email protected]. The Common App will prompt an applicant to add their high school counselor as a recommender, which will trigger an email notification to the counselor instructing them to suBmit an electronic transcript through the Common App portal (free of charge). By mail or in-person: Paper transcripts can Be mailed directly from the high school or Brought in an envelope University of Utah YES sealed By the high school to the following address. The University of Utah Office of Admissions 201 South 1460 East, Room 250s Salt Lake City, UT 84112 Due to COVID-19, we recommend that students use an approved electronic service or mail in official transcripts. -

Escalante in Dixie Arizona Strip
Escalante in Dixie Arizona Strip BY HERBERT EUGENE BOLTON, PH D. UNIVERSITY OF CALIFORNIA Reprinted from THE NEW MEXICO HISTORICAL REVIEW Vol. III, No. 1, January, 1928 _. ..........=.....r___ I =r-l= _ ,...T.... --' - SCALE i 0 ,.. ESCALANTES , .., ...1 RAIL •rt 5C•Ps‘... %)t" Aillik alliaM A ,... •s, ,0 4..)0,/ RD CD OMPF k f C>INS I at '-( DE n P P LA " ZA A GO7LA • 4 a.,.• >,.. 4.. .,.., .... --.., 111 i 0 , 1111‘' 0 Iv TI: 4 NSANIE )..Z L i i L Q 4 ...4 GA s HUGQLIN ,11111 — 5 , II re — S , :: TAeti,?5A,;N22,1 / /t IFt PAC HIS St CDORC / ii • • win,* mu?, -- o MN LO IN. De 0 ti. 2 wto ''' ( Cr-i" ? ICP , _ • t / / / A 7711 I GA TA - GERTRUDIG I... ADDIADOID SAN ANGEL 1 ii onf, TEAM PL. , D 0110 MIMS ? il 31 N $AMUL. DOM DI WPM'S DIUDVOID Ilir ,Obtontœr ennt q .. / \ \\ik,„,, v _IN EDIDLD R „Ilrpoll 1 nt emote R, 0 401.10 CD at P.:4 *TM M jillI I INA 111 ' • ti ESCALANTE IN "DIXIE" AND THE ARIZONA STRIP MAP COMPILED BY H. E. BOLTON ESCALANTE IN DIXIE 41 ESCALANTE IN DIXIE AND THE ARIZONA STRIP HERBERT EUGENE BOLTON INTRODUCTORY Remarkable among explorations in North America in the later eighteenth century — that time of remarkable explorations in the Southwest and on the Pacific Slope — was the expedition made by Father Escalante in 1776. The friar's aim was two-fold. The government in Mexico de- sired to open direct communication between old Santa Fe and newly founded Monterey, in Upper California. -

The Utah Black Hawk War 1865-1871
Utah State University DigitalCommons@USU All Graduate Plan B and other Reports Graduate Studies 5-1969 The Utah Black Hawk War 1865-1871 Deloy J. Spencer Utah State University Follow this and additional works at: https://digitalcommons.usu.edu/gradreports Part of the Sociology Commons Recommended Citation Spencer, Deloy J., "The Utah Black Hawk War 1865-1871" (1969). All Graduate Plan B and other Reports. 600. https://digitalcommons.usu.edu/gradreports/600 This Report is brought to you for free and open access by the Graduate Studies at DigitalCommons@USU. It has been accepted for inclusion in All Graduate Plan B and other Reports by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. THE UTAH BLACK HAWK WAR 1865-1871 by DeJoy J Spencer A report submitted in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in Social Science Plan B UTAH STATE UNIVERSITY Logan, Utah 1969 Black Hawk and his redskin band, Was a terror in the land, Proud he was the Indian chief, Who could live on Mormon beef. F. Christensen PREFACE From 1865 until 1871 the Territory of Utah was the scene of a little known war. The Ute and Piute Indians responding to pressure of white settlers devastated much of Utah south of Spanish Fork. During the first three years of warfare the Mormon Settlements south of the Utah Valley struggled to exist. The next three years saw improving conditions but a continuation of raids by the Navaho in the south. This was a private war.