Managing Depression with Buddhist Practices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Notes and Topics: Synopsis of Taranatha's History
SYNOPSIS OF TARANATHA'S HISTORY Synopsis of chapters I - XIII was published in Vol. V, NO.3. Diacritical marks are not used; a standard transcription is followed. MRT CHAPTER XIV Events of the time of Brahmana Rahula King Chandrapala was the ruler of Aparantaka. He gave offerings to the Chaityas and the Sangha. A friend of the king, Indradhruva wrote the Aindra-vyakarana. During the reign of Chandrapala, Acharya Brahmana Rahulabhadra came to Nalanda. He took ordination from Venerable Krishna and stu died the Sravakapitaka. Some state that he was ordained by Rahula prabha and that Krishna was his teacher. He learnt the Sutras and the Tantras of Mahayana and preached the Madhyamika doctrines. There were at that time eight Madhyamika teachers, viz., Bhadantas Rahula garbha, Ghanasa and others. The Tantras were divided into three sections, Kriya (rites and rituals), Charya (practices) and Yoga (medi tation). The Tantric texts were Guhyasamaja, Buddhasamayayoga and Mayajala. Bhadanta Srilabha of Kashmir was a Hinayaist and propagated the Sautrantika doctrines. At this time appeared in Saketa Bhikshu Maha virya and in Varanasi Vaibhashika Mahabhadanta Buddhadeva. There were four other Bhandanta Dharmatrata, Ghoshaka, Vasumitra and Bu dhadeva. This Dharmatrata should not be confused with the author of Udanavarga, Dharmatrata; similarly this Vasumitra with two other Vasumitras, one being thr author of the Sastra-prakarana and the other of the Samayabhedoparachanachakra. [Translated into English by J. Masuda in Asia Major 1] In the eastern countries Odivisa and Bengal appeared Mantrayana along with many Vidyadharas. One of them was Sri Saraha or Mahabrahmana Rahula Brahmachari. At that time were composed the Mahayana Sutras except the Satasahasrika Prajnaparamita. -

Yoga of Hevajra
Y oga of H evajra Practice of the Y uan K hans? Zoltán Cser Dharma Gate Buddhist College, Budapest Premise1 In the article of Shen Weirong we read2: “It has been widely accepted that Tibetan tantric Buddhism was very popular at the court of the great Mongol khans, yet little is known about the details of the Buddhist teaching that were taught and practiced enthusiastically in and outside the Mongol court of the Yuan dynasty. Due to the prevailing misconception that it was the tantric practice of Tibetan Buddhism, notoriously epitomized in the so-called Secret Teach ing of Supreme Bliss mimi daxile fa; esoteric samádhi of great joy), that caused the rapid downfall of the great Mongol-Yuan dynasty.” “Twenty years ago, I. Christopher Beckwith drew attention to a till then unnoticed Yuan-period collection in Chinese on Tibetan tantric Buddhist teachings. This col lection is called ^ fill? itt Dacheng yaodao miji, or Secret Collection of Works on the Quintessential Path of the Mahdyana. It includes at least 28 texts devoted3 to ÜtH daoguo, or lam ‘bras (the path and fruit) teaching, which are particularly fa voured by the Sa skya pa sect, and to da shouyin, or Mahdmudra. According to the publisher’s preface, this collection became a basic teachings text of the esoteric school in China, and from the Yuan through the Ming and Manchu Qing dynasties down to the present day it has been revered as a ‘sacred classic of the esoteric school.’ This collection attributed to Phagpa lama (1235-1280).” Let us see first of all the historical background, how the Khans were initiated into Hevajra tantra, one of the highest teaching in Buddhism. -

Mindfulness and the Buddha's Noble Eightfold Path
Chapter 3 Mindfulness and the Buddha’s Noble Eightfold Path Malcolm Huxter 3.1 Introduction In the late 1970s, Kabat-Zinn, an immunologist, was on a Buddhist meditation retreat practicing mindfulness meditation. Inspired by the personal benefits, he de- veloped a strong intention to share these skills with those who would not normally attend retreats or wish to practice meditation. Kabat-Zinn developed and began con- ducting mindfulness-based stress reduction (MBSR) in 1979. He defined mindful- ness as, “the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment to moment” (Kabat-Zinn 2003, p. 145). Since the establishment of MBSR, thousands of individuals have reduced psychological and physical suffering by attending these programs (see www.unmassmed.edu/cfm/mbsr/). Furthermore, the research into and popularity of mindfulness and mindfulness-based programs in medical and psychological settings has grown exponentially (Kabat-Zinn 2009). Kabat-Zinn (1990) deliberately detached the language and practice of mind- fulness from its Buddhist origins so that it would be more readily acceptable in Western health settings (Kabat-Zinn 1990). Despite a lack of consensus about the finer details (Singh et al. 2008), Kabat-Zinn’s operational definition of mindfulness remains possibly the most referred to in the field. Dozens of empirically validated mindfulness-based programs have emerged in the past three decades. However, the most acknowledged approaches include: MBSR (Kabat-Zinn 1990), dialectical behavior therapy (DBT; Linehan 1993), acceptance and commitment therapy (ACT; Hayes et al. 1999), and mindfulness-based cognitive therapy (MBCT; Segal et al. -

Beyond Mind II: Further Steps to a Metatranspersonal Philosophy and Psychology Elías Capriles University of the Andes
International Journal of Transpersonal Studies Volume 25 | Issue 1 Article 3 1-1-2006 Beyond Mind II: Further Steps to a Metatranspersonal Philosophy and Psychology Elías Capriles University of the Andes Follow this and additional works at: https://digitalcommons.ciis.edu/ijts-transpersonalstudies Part of the Philosophy Commons, Psychology Commons, and the Religion Commons Recommended Citation Capriles, E. (2006). Capriles, E. (2006). Beyond mind II: Further steps to a metatranspersonal philosophy and psychology. International Journal of Transpersonal Studies, 25(1), 1–44.. International Journal of Transpersonal Studies, 25 (1). http://dx.doi.org/ 10.24972/ijts.2006.25.1.1 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the Journals and Newsletters at Digital Commons @ CIIS. It has been accepted for inclusion in International Journal of Transpersonal Studies by an authorized administrator of Digital Commons @ CIIS. For more information, please contact [email protected]. Beyond Mind II: Further Steps to a Metatranspersonal Philosophy and Psychology Elías Capriles University of The Andes Mérida, Venezuela Some of Wilber’s “holoarchies” are gradations of being, which he views as truth itself; however, being is delusion, and its gradations are gradations of delusion. Wilber’s supposedly universal ontogenetic holoarchy contradicts all Buddhist Paths, whereas his view of phylogeny contradicts Buddhist Tantra and Dzogchen, which claim delusion/being increase throughout the aeon to finally achieve reductio ad absur- dum. Wilber presents spiritual healing as ascent; Grof and Washburn represent it as descent—yet they are all equally off the mark. -

And Daemonic Buddhism in India and Tibet
Florida State University Libraries Electronic Theses, Treatises and Dissertations The Graduate School 2012 The Raven and the Serpent: "The Great All- Pervading R#hula" Daemonic Buddhism in India and Tibet Cameron Bailey Follow this and additional works at the FSU Digital Library. For more information, please contact [email protected] THE FLORIDA STATE UNIVERSITY COLLEGE OF ARTS AND SCIENCES THE RAVEN AND THE SERPENT: “THE GREAT ALL-PERVADING RHULA” AND DMONIC BUDDHISM IN INDIA AND TIBET By CAMERON BAILEY A Thesis submitted to the Department of Religion in partial fulfillment of the requirements for the degree of Master of Religion Degree Awarded: Spring Semester, 2012 Cameron Bailey defended this thesis on April 2, 2012. The members of the supervisory committee were: Bryan Cuevas Professor Directing Thesis Jimmy Yu Committee Member Kathleen Erndl Committee Member The Graduate School has verified and approved the above-named committee members, and certifies that the thesis has been approved in accordance with university requirements. ii For my parents iii ACKNOWLEDGEMENTS I would like to thank, first and foremost, my adviser Dr. Bryan Cuevas who has guided me through the process of writing this thesis, and introduced me to most of the sources used in it. My growth as a scholar is almost entirely due to his influence. I would also like to thank Dr. Jimmy Yu, Dr. Kathleen Erndl, and Dr. Joseph Hellweg. If there is anything worthwhile in this work, it is undoubtedly due to their instruction. I also wish to thank my former undergraduate advisor at Indiana University, Dr. Richard Nance, who inspired me to become a scholar of Buddhism. -

Mongol Rulers, Yugur Subjects, and Tibetan Buddhism 377
Mongol Rulers, Yugur Subjects, and Tibetan Buddhism 377 Chapter 15 Mongol Rulers, Yugur Subjects, and Tibetan Buddhism Translated by Ilia Mozias and Meir Shahar Yang Fuxue and Zhang Haijuan Yang and Zhang Tibetan Buddhism has played a pivotal part in Asian history. The formation of a distinct ethnic group with an equally distinct culture, the Yugurs (Chinese: Yugu zu 裕固族) is an excellent example of such influence. Officially recog- nized as one of China’s fifty-six national minorities, the Yugurs reside in present-day Gansu Province. Their origins can be traced back to the Yuan period (1279–1368), when the local Uighur population (Chinese: Weiwuer zu 維 吾爾族) was ruled by a Mongol clan, (hereafter: the Bin 豳 Clan, after the title that was bestowed upon its chieftains by Kublai Khan (1215–1294)). The leaders of the Bin Clan were ardent supporters of Tantric Buddhism. Under their influ- ence the Mongols and Uighurs converted to the Tibetan faith, a move that served to unite them. Their common religion enabled the Mongol rulers and their Uighur subjects to forge a very particular identity, to wit, the Yugur nationality. The dual ethnic origins of the Yugurs—Uighur and Mongol—are linguisti- cally attested. To this day, the Yugurs are split down the language divide: one group speaks a variant of the Uighur (Turkic) language whereas the other con- verses in a Mongolian dialect. At the same time, their shared Tantric beliefs distinguish both subgroups from the Uighur Muslim population in Western Xinjiang Province while their Uighur heritage differentiates them from the Mongols to the north. -
Introduction to Tibetan Buddhism, Revised Edition
REVISED EDITION John Powers ITTB_Interior 9/20/07 2:23 PM Page 1 Introduction to Tibetan Buddhism ITTB_Interior 9/20/07 2:23 PM Page 2 ITTB_Interior 9/20/07 2:23 PM Page 3 Introduction to Tibetan Buddhism revised edition by John Powers Snow Lion Publications ithaca, new york • boulder, colorado ITTB_Interior 9/20/07 2:23 PM Page 4 Snow Lion Publications P.O. Box 6483 • Ithaca, NY 14851 USA (607) 273-8519 • www.snowlionpub.com © 1995, 2007 by John Powers All rights reserved. First edition 1995 Second edition 2007 No portion of this book may be reproduced by any means without prior written permission from the publisher. Printed in Canada on acid-free recycled paper. Designed and typeset by Gopa & Ted2, Inc. Library of Congress Cataloging-in-Publication Data Powers, John, 1957- Introduction to Tibetan Buddhism / by John Powers. — Rev. ed. p. cm. Includes bibliographical references and indexes. ISBN-13: 978-1-55939-282-2 (alk. paper) ISBN-10: 1-55939-282-7 (alk. paper) 1. Buddhism—China—Tibet. 2. Tibet (China)—Religion. I. Title. BQ7604.P69 2007 294.3’923—dc22 2007019309 ITTB_Interior 9/20/07 2:23 PM Page 5 Table of Contents Preface 11 Technical Note 17 Introduction 21 Part One: The Indian Background 1. Buddhism in India 31 The Buddha 31 The Buddha’s Life and Lives 34 Epilogue 56 2. Some Important Buddhist Doctrines 63 Cyclic Existence 63 Appearance and Reality 71 3. Meditation 81 The Role of Meditation in Indian and Tibetan Buddhism 81 Stabilizing and Analytical Meditation 85 The Five Buddhist Paths 91 4. -

The Tibetan Translation of the Indian Buddhist Epistemological Corpus
187 The Tibetan Translation of the Indian Buddhist Epistemological Corpus Pascale Hugon* As Buddhism was transmitted to Tibet, a huge number of texts were translated from Sanskrit, Chinese and other Asian languages into Tibetan. Epistemological treatises composed by In dian Buddhist scholars – works focusing on the nature of »valid cognition« and exploring peripheral issues of philosophy of mind, logic, and language – were, from the very beginning, part of the translated corpus, and had a profound impact on Tibetan intellectual history. This paper looks into the progression of the translation of such works in the two phases of the diffusion of Buddhism to Tibet – the early phase in the seventh to the ninth centuries and the later phase starting in the late tenth century – on the basis of lists of translated works in various catalogues compiled in these two phases and the contents of the section »epistemo logy« of canonical collections (Tenjur). The paper inquires into the prerogatives that directed the choice of works that were translated, the broader or narrower diffusion of existing trans lations, and also highlights preferences regarding which works were studied in particular contexts. I consider in particular the contribution of the famous »Great translator«, Ngok Loden Shérap (rngog blo ldan shes rab, 10591109), who was also a pioneer exegete, and discuss some of the practicalities and methodology in the translation process, touching on the question of terminology and translation style. The paper also reflects on the status of translated works as authentic sources by proxy, and correlatively, on the impact of mistaken translations and the strategies developed to avoid them. -
A Brief Introduction to Buddhism and the Sakya Tradition
A brief introduction to Buddhism and the Sakya tradition © 2016 Copyright © 2016 Chödung Karmo Translation Group www.chodungkarmo.org International Buddhist Academy Tinchuli–Boudha P.O. Box 23034 Kathmandu, Nepal www.internationalbuddhistacademy.org Contents Preface 5 1. Why Buddhism? 7 2. Buddhism 101 9 2.1. The basics of Buddhism 9 2.2. The Buddha, the Awakened One 12 2.3. His teaching: the Four Noble Truths 14 3. Tibetan Buddhism: compassion and skillful means 21 4. The Sakya tradition 25 4.1. A brief history 25 4.2. The teachings of the Sakya school 28 5. Appendices 35 5.1. A brief overview of different paths to awakening 35 5.2. Two short texts on Mahayana Mind Training 39 5.3. A mini-glossary of important terms 43 5.4. Some reference books 46 5 Preface This booklet is the first of what we hope will become a small series of introductory volumes on Buddhism in thought and practice. This volume was prepared by Christian Bernert, a member of the Chödung Karmo Translation Group, and is meant for interested newcomers with little or no background knowledge about Buddhism. It provides important information on the life of Buddha Shakyamuni, the founder of our tradition, and his teachings, and introduces the reader to the world of Tibetan Buddhism and the Sakya tradition in particular. It also includes the translation of two short yet profound texts on mind training characteristic of this school. We thank everyone for their contributions towards this publication, in particular Lama Rinchen Gyaltsen, Ven. Ngawang Tenzin, and Julia Stenzel for their comments and suggestions, Steven Rhodes for the editing, Cristina Vanza for the cover design, and the Khenchen Appey Foundation for its generous support. -

How to Do Prostration by Sakya Pandita
How to do prostration By Sakya Pandita NAMO MANJUSHRIYE NAMO SUSHIRIYE NAMA UTAMA SHIRIYE SVAHA NAMO GURU BHYE NAMO BUDDHA YA NAMO DHARMA YA NAMO SANGHA YA By offering prostrations toward the exalted Three Jewels, may I and all sentient beings be purified of our negativities and obscurations. Folding the two hands evenly, may we attain the integration of method and wisdom. Placing folded hands on the crown, may we be born in the exalted pure realm of Sukhavati. Placing folded hands at the forehead, may we purify all negative deeds and obscurations of the body. Placing folded hands at the throat, may we purify all negative deeds and obscurations of the voice. Placing folded hands at the heart, may we purify all negative deeds and obscurations of the mind. Separating the folded hands, may we be able to perform the benefit of beings through the two rupakaya. Touching the two knees to the floor, may we gradually travel the five paths and ten stages. Placing the forehead upon the ground, may we attain the eleventh stage of perpetual radiance. Bending and stretching the four limbs, may we spontaneously accomplish the four holy activities of peace, increase, magnetizing, and subjugation of negative forces. Bending and stretching all veins and channels, may we untie the vein knots. Straightening and stretching the backbone and central channel, may we be able to insert all airs without exception into the central channel. Rising from the floor, may we be able to attain liberation by not abiding in samsara. 1 Repeatedly offering this prostration many times, may we be able to rescue sentient beings by not abiding in peace. -
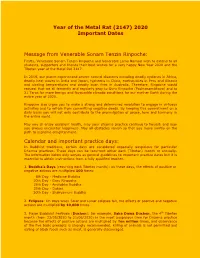
2020 Important Dates Message from Venerable Sonam Tenzin Rinpoche
Year of the Metal Rat (2147) 2020 Important Dates Message from Venerable Sonam Tenzin Rinpoche: Firstly, Venerable Sonam Tenzin Rinpoche and Venerable Lama Namsai wish to extend to all students, supporters and friends their best wishes for a very happy New Year 2020 and the Tibetan year of the Metal Rat 2147. In 2019, our planet experienced severe natural disasters including deadly cyclones in Africa, deadly heat waves in India and Japan, typhoons in China, earthquakes in Peru and Albania and sizzling temperatures and deadly bush fires in Australia. Therefore, Rinpoche would request that we all fervently and regularly pray to Guru Rinpoche (Padmasambhava) and to 21 Taras for more benign and favourable climatic conditions for our mother Earth during the entire year of 2020. Rinpoche also urges you to make a strong and determined resolution to engage in virtuous activities and to refrain from committing negative deeds. By keeping this commitment on a daily basis you will not only contribute to the promulgation of peace, love and harmony in the entire world. May you all enjoy excellent health, may your dharma practice continue to flourish and may you always encounter happiness. May all obstacles vanish so that you move swiftly on the path to supreme enlightenment. Calendar and important practice days: In Buddhist traditions, certain days are considered especially auspicious for particular Dharma practices. These days can be recurrent either each (Tibetan) month or annually. The information below only serves as general guidelines to important practice dates but it is essential to obtain instructions from a fully qualified teacher. -

Sakya Pandita's "Subbasitaratnanidid" a Work on Elegant Sayings
SAKYA PANDITA'S "SUBBASITARATNANIDID" A WORK ON ELEGANT SAYINGS -BY BHAJAGOVINDA GHOSH. Sakya Pandita or (Sa-pan as he i~ usually known among the Tibetan). flourished in 1182-1251 AD. who like hi~ nephew. Lama 'Phagspa (1235-80 AD) played an important role in i1Jhe Moogolian period. Sa-pan was not ooly an important abbot in the loog line. and al~ the leader of ooe of the most powerful Lamaist sect but also it appearS as the king of a large part of Tibet (H. Hoffmann: Religions of Tibet. p. 129). Be was an erudite shoclar in Buddhist lore and composed many original texts on Buddhist philosophy and Tantra and Sanskrit and Tibetan poetics. The pr~~nt work under discussioo, is a famous work on witty. epigrammatic, instructive and descriptive verses with their sources like Subhasita Ratna BhaJQ4agara or gems of Sanskrit poetry (Ed. by Narayan Ram ACarya, Bombay. 1952). The book consists of the following chapters. 1. mkhar. pa. brtag. po. ste. rab. tu. ~d. pa. dang. Pd0, the first ch. Analysis of scholar; 2. ya. rabs. bl'lag. pa. ste. rab. tu. byed. pa. gnyis. p(j0, the second ch. Analysis of NOble class; 3. blunt po. brtag. po. $Ie. rab. tu· byed. po. gsum. pa'o, the third ch. Analysis of fool; 4. spel. rna. brtag. po. ste. rab. tu. byed. pa. bshi. pa'o, the fourth ch. Analysis of mixed subjects; 5. neon. spyod. brtag. pa. ate. rab. Ju. byed. po. inga. pdo. the fifth 00. Analysis of ill manners; 6. rang. bshin. gyi, tshul. brtag.