Supplemental Appendix S1. COMPASS Outcome Definitions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UKRAINIAN FOOD JOURNAL 2016 V.5 Is.3.Pdf
ISSN 2313–5891 (Online) ISSN 2304–974X (Print) Ukrainian Food Journal Volume 5, Issue 3 2016 Kyiv Kиїв 2016 Ukrainian Food Journal is an Ukrainian Food Journal – міжнародне international scientific journal that наукове періодичне видання для publishes innovative papers of expert in the публікації результатів досліджень fields of food science, engineering and фахівців у галузі харчової науки, техніки technology, chemistry, economics and та технології, хімії, економіки і management. управління. The advantage of research results Перевага в публікації результатів publication available to students, graduate досліджень надається студентам, students, young scientists. аспірантам та молодим вченим. Ukrainian Food Journal is abstracted and Ukrainian Food Journal індексується indexed by scientometric databases: наукометричними базами: Index Copernicus (2012) EBSCO (2013) Google Scholar (2013) UlrichsWeb (2013) Global Impact Factor (2014) CABI full text (2014) Online Library of University of Southern Denmark (2014) Directory of Research Journals Indexing (DRJI) (2014) Universal Impact Factor (2014) Directory of Open Access scholarly Resources (ROAD) (2014) European Reference Index for the Humanities and the Social Sciences (ERIH PLUS) (2014) Directory of Open Access Journals (DOAJ) (2015) InfoBase Index (2015) Chemical Abstracts Service Source Index (CASSI) (2016) Ukrainian Food Journal включено у перелік наукових фахових видань України з технічних наук, в якому можуть публікуватися результати дисертаційних робіт на здобуття наукових ступенів доктора і кандидата наук (Наказ Міністерства освіти і науки України № 1609 від 21.11.2013) Editorial office address: Адреса редакції: National University Національний університет of Food Technologies харчових технологій Volodymyrska str., 68 вул. Володимирська, 68 Ukraine, Kyiv 01601 Київ 01601 e-mail: [email protected] Scientific Council of the National Рекомендовано вченою радою University of Food Technologies Національного університету recommends the journal for printing. -

Challenge Jogging Province De Liège 2016 8E 15 KM De Liège - 1 Mei 2016 2,7 KM
Challenge Jogging Province de Liège 2016 8e 15 KM de Liège - 1 mei 2016 2,7 KM PL NR Naam Woonplaats Club Age CAT P/CAT Tijd GEM KM-Tijd 1 20301 BARÉ François LIÈGE RFCL ATHLÉTISME 14 esh 1 0:09:08 17,74 3:23 2 46493 ARNONE RFCL 16 esh 2 0:09:10 17,67 3:24 3 20272 SENTERRE Guillaume STE-VÉ 3 SEC 3K 15 esh 3 0:09:26 17,17 3:30 4 20244 MAES Abel STE-VÉ 2 SEC 3K 14 esh 4 0:09:41 16,73 3:35 5 20035 DETHIER Alexandre 11 esh 5 0:09:45 16,62 3:37 6 20045 JAMME Martin LIÈGE RFCL 18 seh 1 0:09:52 16,42 3:39 7 20117 KALIN Lionel HENRI-CHAPELLE HAUTES FAGNES 11 esh 6 0:09:56 16,31 3:41 8 20271 SAMPSON Yanni STE-VÉ 6 PRIM 3 12 esh 7 0:10:01 16,17 3:43 9 20334 VANGEEBERGEN Hugo LIEGE RFCL 12 esh 8 0:10:09 15,96 3:46 10 20228 LAMARCHE Matéo STE-VÉ 1 SEC 3K 13 esh 9 0:10:15 15,80 3:48 11 20221 JADOUL Nicolas STE-VÉ 2 SEC 3K 14 esh 10 0:10:26 15,53 3:52 12 20258 OLIVIER Augustin STE-VÉ 2 SEC 3K 14 esh 11 0:10:32 15,38 3:54 13 20121 PIEDBOEUF Maxime EMBOURG CSM 6 esh 12 0:10:34 15,33 3:55 14 20036 GOULARD Charles Antoine LIÈGE HERSTAL ATHLÉTI 13 esh 13 0:10:35 15,31 3:55 15 20166 DALNE Victor STE-VÉ 2 SEC 3K 14 esh 14 0:10:37 15,26 3:56 16 20262 POLLERS Tim STE-VÉ 2 SEC 3K 14 esh 15 0:10:48 15,00 4:00 17 20180 D'HOEGELEER Pierre STE-VÉ SYMPATHI 14 esh 16 0:10:52 14,91 4:01 18 20288 WILSON Robert STE-VÉ PARENT 3 42 seh 2 0:10:53 14,89 4:02 19 20647 PIERRE Arthur 12 esh 17 0:10:54 14,86 4:02 20 20033 SWINNEN Eliott 8 esh 18 0:10:57 14,79 4:03 21 20154 BUSI Carla STE-VÉ 2 SEC 3K 14 esf 1 0:11:00 14,73 4:04 22 20155 BUSI Sacha STE-VÉ 2 SEC 3K 14 esf 2 0:11:00 -
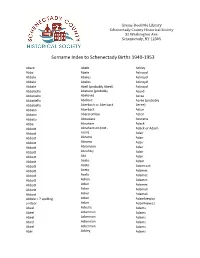
Surname Index to Schenectady Births 1940-1953
Grems-Doolittle Library Schenectady County Historical Society 32 Washington Ave. Schenectady, NY 12305 Surname Index to Schenectady Births 1940-1953 Abare Abele Ackley Abba Abele Ackroyd Abbale Abeles Ackroyd Abbale Abeles Ackroyd Abbale Abell (probably Abeel) Ackroyd Abbatiello Abelone (probably Acord Abbatiello Abelove) Acree Abbatiello Abelove Acree (probably Abbatiello Aberbach or Aberback Aeree) Abbato Aberback Acton Abbato Abercrombie Acton Abbato Aboudara Acucena Abbe Abraham Adack Abbott Abrahamson (not - Adack or Adach Abbott nson) Adair Abbott Abrams Adair Abbott Abrams Adair Abbott Abramson Adair Abbott Abrofsky Adair Abbott Abt Adair Abbott Aceto Adam Abbott Aceto Adamczak Abbott Aceto Adamec Abbott Aceto Adamec Abbott Acken Adamec Abbott Acker Adamec Abbott Acker Adamek Abbott Acker Adamek Abbzle = ? spelling Acker Adamkiewicz unclear Acker Adamkiewicz Abeel Ackerle Adams Abeel Ackerman Adams Abeel Ackerman Adams Abeel Ackerman Adams Abeel Ackerman Adams Abel Ackley Adams Grems-Doolittle Library Schenectady County Historical Society 32 Washington Ave. Schenectady, NY 12305 Surname Index to Schenectady Births 1940-1953 Adams Adamson Ahl Adams Adanti Ahles Adams Addis Ahman Adams Ademec or Adamec Ahnert Adams Adinolfi Ahren Adams Adinolfi Ahren Adams Adinolfi Ahrendtsen Adams Adinolfi Ahrendtsen Adams Adkins Ahrens Adams Adkins Ahrens Adams Adriance Ahrens Adams Adsit Aiken Adams Aeree Aiken Adams Aernecke Ailes = ? Adams Agans Ainsworth Adams Agans Aker (or Aeher = ?) Adams Aganz (Agans ?) Akers Adams Agare or Abare = ? Akerson Adams Agat Akin Adams Agat Akins Adams Agen Akins Adams Aggen Akland Adams Aggen Albanese Adams Aggen Alberding Adams Aggen Albert Adams Agnew Albert Adams Agnew Albert or Alberti Adams Agnew Alberti Adams Agostara Alberti Adams Agostara (not Agostra) Alberts Adamski Agree Albig Adamski Ahave ? = totally Albig Adamson unclear Albohm Adamson Ahern Albohm Adamson Ahl Albohm (not Albolm) Adamson Ahl Albrezzi Grems-Doolittle Library Schenectady County Historical Society 32 Washington Ave. -

Surname Range - Finn - Flemming
Friends of Dundee City Archives – Howff Graveyard of Dundee – FDCA 2010 Surname Range - Finn - Flemming First Other Surname Burial Age Birthplace Occupation Cause of Death Relationship Last Address Names Cemetery Finn Agnes 17 Aug 1824 3 wk Dundee Old Howff Finn Agnes 5 Feb 1843 11 mth Dundee Teething dau of David Finn, Sailor Finn Andrew 10 Oct 1794 Finn Ann 5 Dec 1776 Finn Ann 3 May.. 1816 Finn David 18 Jan 1831 6 wk Dundee Measles Finn Elizabeth 23 Jan 1831 60 Dundee Asthma Finn Margaret 11 Mar 1845 17 Dundee Nervous fit dau of late William Finn, Packer Bucklemaker Wynd Finn Elizabeth 20 Oct 1818 Finn Mary 4 Oct 1817 Finn Owen 31 Oct 1847 21 King's County Labourer Fever Foundry Lane Finn Rose Ann 2 Feb 1852 2 mth Dundee Small Pox dau of Edward Finn, Labourer Peddie's Close, Overgate Finn Jean 9 Feb 1782 Finn Helen 12 Jan 1826 65 Dundee Consumption Old Howff Finn (Begg) James Lapper See Ann Begg Finn (Davidson) Jean 20 Nov 1832 42 Dundee Bursting of a Blood Wife of John Davidson Vessell Finn (McCulloch) Catharine 15 Jul 1849 49 Dundee Cholera Wid of James McCulloch, Labourer Guthrie's Close, Overgate Finnan Mary 10 Jun 1846 13 mth Dundee Small Pox dau of Francis Finnan, Labourer Dudhope Street Finnan Cathatine 19 Jan 1851 2 Dundee Croup dau of Patrick Finnan, Labourer Dudhope Street Finnan (Taylor) Thomas Tidewaiter See Jane Taylor Finnegan Mary 11 Mar 1847 9 mth Dundee ChinCough dau of John Finnegan, Lamp North Tay Street Lighter Finnegan Edward 9 Nov 1833 85 Ireland Late Soldier Old Age Croft Finnen Francis 3 Jan 1847 3 mth Dundee -

Ukr Jour Food Sci V 2 I 2.Pdf
ISSN 2409-4951(Online) ISSN 2310-1008 (Print) Ukrainian Journal of Food Science Volume 2, Issue 2 2014 Kyiv 2014 Ukrainian Journal of Food Science publishes original research articles, short communications, review papers, news and literature reviews. Topic covered by the journal include: Food engineering Food nanotechnologies Food chemistry Food processes Biotechnology, microbiology Economics and management Physical property of food Automation of food processes Food quality and safety Food packaging Health Periodicity of the journal 2 issues per year (June, December). Studies must be novel, have a clear connection to food science, and be of general interest to the international scientific community. The editors make every effort to ensure rapid and fair reviews, resulting in timely publication of accepted manuscripts. Ukrainian Journal of Food Science is Abstracted and indexated by bases: EBSCO (2013), Google Scholar (2013), Index Copernicus (2014), Universal Impact Factor (2014), Directory of Open Access scholarly Resources (ROAD) (2014). Reviewing a Manuscript for Publication. All scientific articles submitted for publication in “Ukrainian Journal of Food Science” are double-blind reviewed by at least two academics appointed by the Editors' Board: one from the Editorial Board and one independent scientist. Copyright. Authors submitting articles for publication warrant that the work is not an infringement of any existing copyright and will indemnify the publisher against any breach of such warranty. For ease of dissemination and to ensure proper policing of use papers and contributions become the legal copyright of the publisher unless otherwise agreed. Academic ethics policy. The Editorial Board of "Ukrainian Journal of Food Science" follows the rules on academic writing and academic ethics, according to the work by Miguel Roig (2003, 2006) "Avoiding plagiarism, self-plagiarism, and other questionable writing practices. -

Immunotherapy of Glioblastoma: Current Strategies and Challenges in Tumor Model Development
cells Review Immunotherapy of Glioblastoma: Current Strategies and Challenges in Tumor Model Development Bernarda Majc 1,2, Metka Novak 1, Nataša Kopitar-Jerala 3 , Anahid Jewett 4 and Barbara Breznik 1,* 1 Department of Genetic Toxicology and Cancer Biology, National Institute of Biology, 111 Veˇcnapot, SI-1000 Ljubljana, Slovenia; [email protected] (B.M.); [email protected] (M.N.) 2 International Postgraduate School Jozef Stefan, 39 Jamova ulica, SI-1000 Ljubljana, Slovenia 3 Department of Biochemistry, Molecular and Structural Biology, Jozef Stefan Institute, 39 Jamova ulica, SI-1000 Ljubljana, Slovenia; [email protected] 4 Division of Oral Biology and Medicine, The Jane and Jerry Weintraub Center for Reconstructive Biotechnology, University of California School of Dentistry, 10833 Le Conte Ave, Los Angeles, CA 90095, USA; [email protected] * Correspondence: [email protected]; Tel.: +386-59-232-870 Abstract: Glioblastoma is the most common brain malignant tumor in the adult population, and im- munotherapy is playing an increasingly central role in the treatment of many cancers. Nevertheless, the search for effective immunotherapeutic approaches for glioblastoma patients continues. The goal of immunotherapy is to promote tumor eradication, boost the patient’s innate and adaptive immune responses, and overcome tumor immune resistance. A range of new, promising immunotherapeutic strategies has been applied for glioblastoma, including vaccines, oncolytic viruses, immune check- point inhibitors, and adoptive cell transfer. However, the main challenges of immunotherapy for glioblastoma are the intracranial location and heterogeneity of the tumor as well as the unique, immunosuppressive tumor microenvironment. Owing to the lack of appropriate tumor models, there are discrepancies in the efficiency of various immunotherapeutic strategies between preclinical Citation: Majc, B.; Novak, M.; studies (with in vitro and animal models) on the one hand and clinical studies (on humans) on the Kopitar-Jerala, N.; Jewett, A.; Breznik, other hand. -

ICON S Conference 17 – 19 June 2016 Humboldt University Berlin
Berlin Berlin 2016 ICON S CONFERENCE 17 – 19 JUNE 2016 HUMBOLDT UNIVERSITY BERLIN We extend a warm welcome to all participants in the 2016 Annual Meeting of ICON S, the International Society of Public Law. This will be our largest Annual Meeting since the foundation of the Society in 2013. The panels, roundtables and plenary events address the Conference’s overarching theme of “Borders, Otherness and Public Law” and other topics at the heart of contemporary public law inquiry. We are grateful to our Berlin hosts for their relentless hard work and creativity in putting together such a mega-sized event, and we thank our sponsors for their generous support. Most of all, we thank you, the ICON S members, for your overwhelmingly positive response to the call for papers this year, and for volunteering your time and energy to promote the success of the Society and its annual conference. Together, we have created what we believe is a first-rate, intellectually appealing program featuring scholars, jurists and policy makers from various disciplines and from literally four corners of the world. We hope that you enjoy it thoroughly! Gráinne de Búrca ( New York University ) and Ran Hirschl ( University of Toronto ) Co-Presidents, ICON S, the International Society of Public Law S Conference ICON WElcomE statEMEnts 1 I WELcoME STATEMENTS 1 II ICON S INAUGURAL GOVERNANCE 3 III SCHEDULE 4 IV MAP OF CONFERENCE VENUES 6 V PLENARY EVENTS 7 VI CONCURRING PANELS 15 a OVERVIEW 16 b PANEls SEssion I 26 c PANEls SEssion II 43 D PANEls SEssion III 77 E PANEls SEssion IV 110 F PANEls SEssion V 143 VII ICON S WP CONFERENCE ProcEEDINGS SERIES 179 VIII SERVICE 180 IX PARTICIPANTS 190 ICON S CONFERENCE 17 – 19 JUNE 2016 HUMBOLDT UNIVERSITY BERLIN We extend a warm welcome to all participants in the 2016 Annual Meeting of ICON S, the International Society of Public Law. -

Index to St. Louis, Missouri Naturalization Records Created After Sept
Index to St. Louis, Missouri Naturalization Records Created after Sept. 27, 1906 Alphabetical surname index L–M History & Genealogy Department St. Louis County Library 1640 S. Lindberg Blvd. St. Louis, Missouri 63131 314-994-3300, ext. 2070 [email protected] Index to St. Louis, Missouri Naturalization Records Created after Sept. 27, 1906 This index covers St. Louis, Missouri naturalization records created between October 1, 1906 and December 1928 and is based on the following sources: • Naturalizations, U.S. District Court—Eastern Division, Eastern Judicial District of Missouri, Vols. 1 – 82 • Naturalizations, U.S. Circuit Court— Eastern Division, Eastern Judicial District of Missouri, Vols. 5 – 21 Entries are listed alphabetically by surname, then by given name, and then numerically by volume number. Abbreviations and Notations SLCL = History and Genealogy Department microfilm number (St. Louis County Library) FHL = Family History Library microfilm number * = spelling taken from the signature which differed from name in index. How to obtain copies Photocopies of indexed articles may be requested by sending an email to the History and Genealogy Department at [email protected]. A limit of three searches per request applies. Please review the library's lookup policy at https://www.slcl.org/genealogy-and-local- history/services. A declaration of intention may lead to further records. For more information, contact the National Archives at the address below. Include all information listed on the declaration of intention. National Archives, Central Plains Region 400 W. Pershing Rd. Kansas City, MO 64108 (816) 268-8000 [email protected] History Genealogy Dept. Index to St. Louis, Missouri Naturalization Records St. -

Kalamazoo County Naturalization Index Order Copies of Records by Calling (517) 373-1408
Last Name First Name Middle Name First Paper Second Paper Maus Joos Cornelius V30P33 V30P33 Max Henry V2P204 Maxted Richard V2P422 May Charles B2F6P23 May Philip B2F6P55 Maybee John C B2F6P140 Mayer Elizabeth Marie V58P3714 Mayer Hendrik V17P3359 Mayer John V17P3234 Mayer Robert V51P3086 Mayers Charles B2F6P9 Mayhew Jacob B2F6P135 Mayr Emanuele Maria V62P4308 Mazkrists Ruta V65P4942 Mazur Josefa V19P3789 Mazur Josefa V55P3416 V55P3415 Mazur Marcin V15P18 Mazurak John V13P291 Mazurkevics Anatolijs V64P4726 Mazurkevics Vilhelmina V64P4727 Mc Neil James V5P72 Mc Rae John A V5P76 McAlpine Daniel Duncan V3P26 McAlpine John C V3P250 McAlpine Peeter V2P426 McArthur Charles B2F5P70 McBeth William L B2F6P84 B2F6P84 McCaffrey Edward B2F6P136 Friday, July 06, 2007 Page 299 of 577 Kalamazoo County Naturalization Index Order copies of records by calling (517) 373-1408 Archives of Michigan Home page: www.michigan.gov/archivesofmi E-mail: [email protected] Last Name First Name Middle Name First Paper Second Paper McCall Hannah V16P3084 McCallum Duncan Clyde V10P370 McCallum Duncan Clyke V23P212 V23P212 McCally Geoffrey Thomas V52P3165 McCamby Alex B2F6P1 McCamly Daniel B2F6P5 McCandless Frances Georgina Forsythe V61P4262 McCandless Hugh Milligan V20P4331 McCandry Daniel B2F6P5 McClelland George Charles V23P101 McClure Mary Abernethy V10P389 McClurky Charles B2F6P67 McCormick George W V5P33 McCormick Olga V48P2744 McCray Robert B2F6P157 McCudden John B2F6P150 McCue Hugh B2F5P56 McCue John B2F6P76 McCue Peter V62P4379 McCugan Vincent Murray V19P3955 -

The Enlightenment of Jean-Baptiste-Louis Gresset, Léger-Marie Deschamps, and Simon-Nicolas-Henri Linguet
‘TOUCHSTONES OF TRUTH’: THE ENLIGHTENMENT OF JEAN-BAPTISTE-LOUIS GRESSET, LÉGER-MARIE DESCHAMPS, AND SIMON-NICOLAS-HENRI LINGUET DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Mircea Alexandru Platon, M.A. Graduate Program in History The Ohio State University 2012 Dissertation Committee: Dr. Dale K. Van Kley, Adviser Dr. Alice Conklin, Adviser Dr. Nicholas Breyfogle Copyright Mircea Alexandru Platon 2012 ABSTRACT My dissertation, “ ‘Touchstones of Truth’: The Enlightenment of J.-B.-L. Gresset, L.-M. Deschamps, and S.-N.-H. Linguet,” focuses on three key but little studied opponents of the philosophes. I argue that the writer Jean-Baptiste-Louis Gresset (1709- 1777), the philosopher Léger-Marie Deschamps (1716-1774), and the lawyer and political theorist Simon-Nicolas-Henri Linguet (1736-1794) opposed the philosophes in the name of a set of universally valid principles against what they took to be the philosophes' superficial, self-serving, and haphazard politicization of language, philosophy and the social sciences. These three intellectuals warned that such politicization fostered economic, political, and intellectual inequality as well as cultural alienation, thereby undermining the Enlightenment’s own vision of a world of self-emancipated human beings and pushing France in the direction of a violent revolution. Gresset supported a “civic republican” political economy of virtue, and warned about the dangers of the consumer culture fostered by the philosophes. The roots of his cultural criticism lay in moral and political concerns that found expression in a patriotic discourse stressing the importance of social “harmony” and the common good while rejecting any temptation to belong to a “party.” In this spirit, Gresset defended the “ancient constitution” against idle monks, royal or ministerial despotism, parlementarian rebellion, and the philosophes. -

Land Tenure in Acadian Agricultural Settlements, 1604-1755: Cultural Retention and the Emergence of Custom Carol A
The University of Maine DigitalCommons@UMaine Electronic Theses and Dissertations Fogler Library Summer 8-5-2019 Land Tenure in Acadian Agricultural Settlements, 1604-1755: Cultural Retention and the Emergence of Custom Carol A. Blasi University of Maine, [email protected] Follow this and additional works at: https://digitalcommons.library.umaine.edu/etd Part of the Canadian History Commons, Cultural History Commons, and the Legal Commons Recommended Citation Blasi, Carol A., "Land Tenure in Acadian Agricultural Settlements, 1604-1755: Cultural Retention and the Emergence of Custom" (2019). Electronic Theses and Dissertations. 3053. https://digitalcommons.library.umaine.edu/etd/3053 This Open-Access Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. LAND TENURE IN ACADIAN AGRICULTURAL SETTLEMENTS, 1604-1755: CULTURAL RETENTION AND THE EMERGENCE OF CUSTOM by Carol Ann Blasi BA, Syracuse University, 1978 MA, The University of Chicago Divinity School, 1981 JD, Temple University School of Law, 1986 A DISSERTATION Submitted in Partial Fulfillment of the Requirements for theDegree of Doctor of Philosophy (in History) The Graduate School The University of Maine August, 2019 Advisory Committee Members: Jacques Ferland, Associate Professor of History, Advisor Alexander Grab, Emeritus Professor of History Stephen J. Hornsby, Professor of Geography and Canadian Studies Richard W. Judd, Emeritus Professor of History Liam Riordan, Professor of History © 2019 Carol Ann Blasi All Rights Reserved ii LAND TENURE IN ACADIAN AGRICULTURAL SETTLEMENTS, 1604-1755 CULTURAL RETENTION AND THE EVOLUTION OF CUSTOM By Carol Ann Blasi Dissertation Advisor: Dr. -

Watermill at No Mill Could Have Been Created Without the Millwright, and No Historical Background Complete Without His Mention
H.H.L Carpenter Liverpool College of Higher Education The Watermill at No mill could have been created without the millwright, and no historical background complete without his mention. Millwrighting was a craft which grew up with the invention of the water and windmills. It was a completely adaptable craft, for Bunbury no two mills were ever the same. It had no previous technologies to guide it, except for the construction that now remains of the 1960 complex, which of the wheel itself and the construction of the comprised the mill itself, stables and an engine shed. building. Both of these crafts came together under The miller still occupies the mill house which stands the jurisdiction of the one man who had to adapt 100 m. away. them to his needs. The wheel needed modifying The present structure is a three storied brick to take the strains imposed upon it and, more building on a sandstone foundation which is built importantly, for cogs or paddles to be fitted. into the damside. It houses the water-wheel and all The buildings, and here I include the ancillary the gearing and machinery of the mill. The dam constructions to direct the water onto the wheel, which creates the millpond has a sluice on one side had to be custom made to suit the millwright, of the mill and a culvert to direct the water onto the for this later became the task of the mason. wheel in the mill at first floor level. It also affords This idea helps to distinguish the character of access to the top floor for the off-loading and the millwright.