Major Emergency Procedure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accounts Commission Papers for Meeting
The Accounts Commission for Scotland Agenda Meeting on Thursday 20 January 2011, in the offices of Audit Scotland, 18 George Street, Edinburgh The meeting will begin at 10:00 am 1. Apologies for absence 2. Declarations of interest 3. Decisions on taking business in private: The Commission will consider whether to take items 13, 14 and 15 in private. 4. Minutes of meeting of 9 December 2010 5. Minutes of meeting of the Performance Audit Committee of 9 December 2010 6. Chair’s introduction: The Chair will report on recent activity and issues of interest to the Commission. 7. Update report by the Controller of Audit: The Commission will consider a report from the Controller of Audit on significant recent activity in relation to the audit of local government. 8. Public Services Reform (Scotland) Act 2010: The Commission will consider a report on duties arising from the Act. 9. Scottish Government Spending Plans and Draft Budget 2011/12: The Commission will consider a briefing. 10. Grampian Police and Grampian Joint Police Board - Best Value Audit and Inspection: The Commission will consider a joint report by the Controller of Audit and Her Majesty’s Inspectorate of Constabulary for Scotland. 11. Shetland Islands Council: The Commission will consider a report by the Controller of Audit on the annual audit 2009/10. 12. 2010 Local Government Overview: The Commission will consider a report by the Controller of Audit. 13. Grampian Police and Grampian Joint Police Board - Best Value Audit and Inspection: The Commission will consider the action it wishes to take on the report. -

BBC Radio Post-1967
1967 1968 1969 1970 1971 1972 1973 1974 1975 1976 1977 1978 1979 1980 1981 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021 Operated by BBC Radio 1 BBC Radio 1 Dance BBC Radio 1 relax BBC 1Xtra BBC Radio 1Xtra BBC Radio 2 BBC Radio 3 National BBC Radio 4 BBC Radio BBC 7 BBC Radio 7 BBC Radio 4 Extra BBC Radio 5 BBC Radio 5 Live BBC Radio Five Live BBC Radio 5 Live BBC Radio Five Live Sports Extra BBC Radio 5 Live Sports Extra BBC 6 Music BBC Radio 6 Music BBC Asian Network BBC World Service International BBC Radio Cymru BBC Radio Cymru Mwy BBC Radio Cymru 2 Wales BBC Radio Wales BBC Cymru Wales BBC Radio Wales BBC Radio Wales BBC Radio Wales BBC Radio Gwent BBC Radio Wales Blaenau Gwent, Caerphilly, Monmouthshire, Newport & Torfaen BBC Radio Deeside BBC Radio Clwyd Denbighshire, Flintshire & Wrexham BBC Radio Ulster BBC Radio Foyle County Derry BBC Northern Ireland BBC Radio Ulster Northern Ireland BBC Radio na Gaidhealtachd BBC Radio nan Gàidheal BBC Radio nan Eilean Scotland BBC Radio Scotland BBC Scotland BBC Radio Orkney Orkney BBC Radio Shetland Shetland BBC Essex Essex BBC Radio Cambridgeshire Cambridgeshire BBC Radio Norfolk Norfolk BBC East BBC Radio Northampton BBC Northampton BBC Radio Northampton Northamptonshire BBC Radio Suffolk Suffolk BBC Radio Bedfordshire BBC Three Counties Radio Bedfordshire, Hertfordshire & North Buckinghamshire BBC Radio Derby Derbyshire (excl. -
Papers for Accounts Commission Meeting
The Accounts Commission for Scotland Agenda Meeting on Thursday 17 March 2011, in the offices of Audit Scotland, 18 George Street, Edinburgh The meeting will begin at 10:00 am 1. Apologies for absence 2. Declarations of interest 3. Decisions on taking business in private: The Commission will consider whether to take item 13 in private. 4. Minutes of meeting of 17 February 2011 5. Minutes of meeting of the Financial Audit and Assurance Committee of 10 February 2011 6. Chair’s introduction: The Chair will report on recent activity and issues of interest to the Commission. 7. Update report by the Controller of Audit: The Commission will consider a report from the Controller of Audit on significant recent activity in relation to the audit of local government. 8. Co-ordination of local government scrutiny functions: The Commission will consider correspondence from the Cabinet Secretary for Finance and Sustainable Growth. 9. Local government overview reporting: The Commission will consider its approach to future local government overview reports. 10. Reports by the Controller of Audit: The Commission will consider the development of guidance on procedures for consideration of reports by the Controller of Audit. 11. Code of Audit Practice – 2011: The Commission will consider a revised Code of Audit Practice. 12. Accounts Commission Digest: The Commission will consider any points that arise from its regular briefing on current issues. 13. Audit appointments for 2011/12 to 2015/16: The Commission will consider proposals for audit appointments -

Radio in 1984
UK and Ireland Radio Stations in 1984 During the 1980s, there were six main radio services in the UK: Radios 1 to 4, BBC 1984 is a good point at which to take a snapshot. A major expansion of BBC and local and regional radio and a single tier of independent local stations. Most Independent local radio had just completed, supported by the opening of new stations broadcast on both FM and AM, known as simulcasting. The main FM spectrum between 102 and 105 MHz. Most parts of the country could receive exception was Radio 1, which was only available on AM. However, the BBC either a BBC or independent local radio station, but not necessarily both. The national networks broadcast separate FM and AM programmes at certain times. reorganisation of the local radio FM sub-bands did not happen until 1986-7, so Radio 1 borrowed Radio 2’s FM network for a few hours a week. A few Radio 2 many stations (or their successors) now use different frequencies. Many music programmes were also carried on FM only with sport opting out on AM. transmitter powers were also increased after the frequency changes. Radio 3’s AM network sometimes broadcast cricket commentaries with regular By 1984, all of the minor upgrades to the BBC’s national AM networks, following programmes on FM only. Meanwhile Radio 4’s FM network opted out with the reorganisation in 1978 had been completed, leaving them (essentially in their education programmes. final form). The re-engineering of the FM network had begun with 30 new sites Simulcasting was needed because most car radios were AM-only during the added since the late 1970s and several transmitters upgraded to mixed 1980s and many AM-only portable radios purchased in the 1960s and early 1970s polarisation. -
National Qualifications Curriculum Support
NATIONAL QUALIFICATIONS CURRICULUM SUPPORT English and Communication Using Scottish Texts Support Notes and Bibliographies [MULTI-LEVEL] Edited by David Menzies INTRODUCTION First published 1999 Electronic version 2001 © Scottish Consultative Council on the Curriculum 1999 This publication may be reproduced in whole or in part for educational purposes by educational establishments in Scotland provided that no profit accrues at any stage. Acknowledgement Learning and Teaching Scotland gratefully acknowledge this contribution to the Higher Still support programme for English. The help of Gordon Liddell is acknowledged in the early stages of this project. Permission to quote the following texts is acknowledged with thanks: ‘Burns Supper’ by Jackie Kay, from Two’s Company (Blackie, 1992), is reproduced by permission of Penguin Books Ltd; ‘War Grave’ by Mary Stewart, from Frost on the Window (Hodder, 1990), is reproduced by permission of Hodder & Stoughton Ltd; ‘Stealing’, from Selling Manhattan by Carol Ann Duffy, published by Anvil Press Poetry in 1987; ‘Ophelia’, from Ophelia and Other Poems by Elizabeth Burns, published by Polygon in 1991. ISBN 1 85955 823 2 Learning and Teaching Scotland Gardyne Road Dundee DD5 1NY www.LTScotland.com HISTORY 3 CONTENTS Section 1: Introduction (David Menzies) 1 Section 2: General works and background reading (David Menzies) 4 Section 3: Dramatic works (David Menzies) 7 Section 4: Prose fiction (Beth Dickson) 30 Section 5: Non-fictional prose (Andrew Noble) 59 Section 6: Poetry (Anne Gifford) 64 Section 7: Media texts (Margaret Hubbard) 85 Section 8: Gaelic texts in translation (Donald John MacLeod) 94 Section 9: Scots language texts (Liz Niven) 102 Section 10: Support for teachers (David Menzies) 122 ENGLISH III INTRODUCTION HISTORY 5 INTRODUCTION SECTION 1 Introduction One of the significant features of the provision for English in the Higher Still Arrangements is the prominence given to the study of Scottish language and literature. -

Ripe 2019: Universalism in Public Service Media
UNIVERSALISM IN PUBLIC SERVICE MEDIA RIPE 2019 Edited by: Philip Savage, Mercedes Medina, & Gregory Ferrell Lowe Ferrell Lowe, G. & Savage, P. (2020). Universalism in public service media: Paradoxes, challenges, and development in Philip Savage, Mercedes Medina and Gregory Ferrell Lowe (eds.) Universalism in Public Service Media. Gteborg: Nordicom. NORDICOM 1 Logotyp Logotyp Nordicoms huvudlogotyp består av namnet Nordicoms huvudlogotyp består av namnet ”Nordicom”. Logotypen är det enskilt viktigaste ”Nordicom”. Logotypen är det enskilt viktigaste elementet i Nordicoms visuella identitet och den Centrum fr nordisk medieforskning Centrum fr nordisk medieforskning ska finnas med i allt material där Nordicom står som avsändare. Använd alltid godkända original, de kan laddas ner här. Logotypens tre versioner Nordicoms logotyp finns i tre godkända grundversioner. • Logotyp. • Logotyp med undertext. • Logotyp på platta. Centre for Nordic Media Research Centre for Nordic Media Research Logotyp med undertext ska användas i lite större Logotyp med undertext ska användas i lite större format för att presentera Nordicom. Logotyp format för att presenteraBased at the Nordicom. University of Gothenburg,Logotyp Nordicom is a Nordic non-proft knowledge Contacts på platta ska användas där det behövs något centre that collects and communicates facts and research in the feld of media and communication. The purpose of our work is to develop the knowledge of media’s role Editor Administration, sales Postal address grafiskt med mer tyngd. in society. We do this through: Johannes Bjerling, PhD Anne Claesson Nordicom phone: +46 766 18 12 39 phone: +46 31 786 12 16 University of Gothenburg Following and documenting media development in terms of media structure, • [email protected] [email protected] PO Box 713 media ownership, media economy, and media use. -

NHS Shetland Written Submission
HS/S5/18/16/6 Evidence for the Scottish Parliament Health and Sport Committee 15 May 2018 Ralph Roberts Chief Executive NHS Shetland April 2018 Page 1 of 293 HS/S5/18/16/6 1 Context Community Planning and the Islands (Scotland) Bill As the Islands (Scotland) Bill says, “island communities face challenges around geographic remoteness, declining populations, transport and digital connections...”. The Government has stated a commitment to supporting the island communities and improving outcomes by creating the right conditions for growth. Specifically, we consider a strong health service in Shetland to be a pre-requisite of a thriving economy. A strong emergency care response, at the Gilbert Bain Hospital and through other emergency service providers, is essential to businesses being able to invest in, locate to and operate in these islands. It goes without saying that the 200 miles of sea between us and the mainland means that we must have skilled and competent people on the island to deal with any emergencies, as well as a providing a good level of general health care which enables people to feel safe to live in these islands. The concept of community planning is inherent in the way of life for islands. All elements of public, private and voluntary sectors work together, especially in emergency situations, to address issues. Natural connections exists between organisations and individuals which helps build resilience and a flexible approach to making things work at a local level. It is difficult therefore to see Health and Care services in isolation from other essential public services (such as transport, housing and education). -
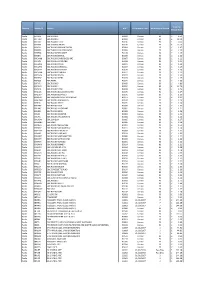
Domain Station ID Station UDC Performance Date No of Days in Period Total Per Minute Rate Radio BR ONE BBC RADIO 1 B0001 Census
Total Per Domain Station ID Station UDC Performance Date No of Days in Period Minute Rate Radio BR ONE BBC RADIO 1 B0001 Census 90 £ 4.51 Radio BR TWO BBC RADIO 2 B0002 Census 90 £ 18.00 Radio BR1EXT BBC RADIO 1XTRA B0106 Census 90 £ 0.60 Radio BR4DIG BBC SCHOOL RADIO B0109 Census 90 £ 13.70 Radio BRASIA BBC RADIO ASIAN NETWORK B0064 Census 90 £ 1.47 Radio BRBEDS BBC THREE COUNTIES RADIO B0065 Census 90 £ 1.25 Radio BRBERK BBC RADIO BERKSHIRE B0103 Census 90 £ 1.19 Radio BRBRIS BBC RADIO BRISTOL B0066 Census 90 £ 1.16 Radio BRCAMB BBC RADIO CAMBRIDGESHIRE B0067 Census 90 £ 1.22 Radio BRCLEV BBC RADIO CLEVELAND B0068 Census 90 £ 1.22 Radio BRCMRU BBC RADIO CYMRU B0011 Census 90 £ 1.24 Radio BRCORN BBC RADIO CORNWALL B0069 Census 90 £ 1.29 Radio BRCOVN BBC RADIO COVENTRY B0070 Census 90 £ 1.18 Radio BRCUMB BBC RADIO CUMBRIA B0071 Census 90 £ 1.23 Radio BRDEVN BBC RADIO DEVON B0072 Census 90 £ 1.30 Radio BRDRBY BBC RADIO DERBY B0073 Census 90 £ 1.25 Radio BRESSX BBC ESSEX B0074 Census 90 £ 1.36 Radio BRFIVE BBC RADIO 5 B0005 Census 90 £ 4.89 Radio BRFOUR BBC RADIO 4 B0004 Census 90 £ 13.70 Radio BRFOYL BBC RADIO FOYLE B0019 Census 90 £ 1.76 Radio BRGLOS BBC RADIO GLOUCESTERSHIRE B0075 Census 90 £ 1.17 Radio BRGUER BBC RADIO GUERNSEY B0076 Census 90 £ 1.13 Radio BRHRWC BBC HEREFORD AND WORCESTER B0077 Census 90 £ 1.21 Radio BRHUMB BBC RADIO HUMBERSIDE B0078 Census 90 £ 1.29 Radio BRJERS BBC RADIO JERSEY B0079 Census 90 £ 1.14 Radio BRKENT BBC RADIO KENT B0080 Census 90 £ 1.32 Radio BRLANC BBC RADIO LANCASHIRE B0081 Census 90 £ 1.21 Radio -

The Dalradian Rocks of the Shetland Islands, Scotland
Revised Manuscript 8/7/12 Click here to view linked References 1 2 3 4 5 The Dalradian rocks of the Shetland Islands, 6 7 Scotland 8 9 10 D. Flinn, P. Stone and D. Stephenson 11 12 Derek Flinn (deceased) formerly The Jane Herdman Laboratories of 13 Geology, University of Liverpool. 14 Phillip Stone British Geological Survey, Murchison House, West 15 Mains Road, Edinburgh EH9 3LA. 16 * David Stephenson British Geological Survey, Murchison House, 17 West Mains Road, Edinburgh EH9 3LA. 18 [email protected] 19 0131 650 0323 20 21 * Corresponding author 22 23 24 Keywords: 25 Geological Conservation Review 26 Shetland Islands 27 Dalradian Supergroup 28 Lithostratigraphy 29 Structural geology 30 Metamorphism 31 32 33 34 35 ABSTRACT 36 37 Metasedimentary and metavolcanic rocks to the east of the Walls 38 Boundary Fault on Shetland have lithological similarities to those 39 of the Dalradian Supergroup of the Scottish mainland. In 40 particular, the middle part of the succession, termed the Whiteness 41 Group, includes numerous metalimestones and associated pelites in a 42 shallow-marine succession that recalls the upper parts of the Appin 43 Group and the Argyll Group of mainland Scotland. Metavolcanic 44 rocks within the deeper water turbiditic sequence of the succeeding 45 Clift Hills Group might be broadly coeval with those of the 46 Southern Highland Group of Scotland. Beyond that, correlations 47 with the established Dalradian succession are tenuous and are not 48 possible at formation level. A local succession immediately west 49 of the Walls Boundary Fault is of even more-dubious Dalradian 50 affinity. -

Hamish Ross Phd Thesis
THE LAST GLACIATION OF SHETLAND Hamish Ross A Thesis Submitted for the Degree of PhD at the University of St Andrews 1997 Full metadata for this item is available in St Andrews Research Repository at: http://research-repository.st-andrews.ac.uk/ Please use this identifier to cite or link to this item: http://hdl.handle.net/10023/15278 This item is protected by original copyright The Last Glaciation of Shetland Hamish Ross University of St Andrews 1996 ProQuest Number: 10171081 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest 10171081 Published by ProQuest LLC(2017). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 Abstract Evidence of the last glaciation of the Shetland Islands, UK, is re-examined and combined with new data on terrestrial glacigenic deposits and recent offshore data from the continental shelf to produce a dynamic, integrated model of the history of the whole ice cap. • It is shown that evidence which has previously been attributed to last glacial, or earlier, Scandinavian ice incursion, might be explained by the eastwards migration of local ice sheds. -
Preparing for Emergencies in the Highlands and Islands
Preparing for Emergencies in the Highlands and Islands A Guide to Civil Contingencies and Resilience Contents O Civil Contingencies 1 O Integrated Emergency Management 2 O Planning your own Emergency Arrangements 5 O How to put together an “Emergency Supply Kit” 6 O Evacuation 10 O Shelter 12 O Local Television and Radio Stations 13 O Floods 14 O Winter storms and extreme cold 17 O Heatwave 20 O Information on Flu 21 O Incidents with hazardous materials 23 O Fire 24 O Pets 27 O The recovery from a disaster 28 O The Procurator Fiscal Service 30 O Useful contact numbers and web pages 31 Introduction In today’s world there is an ongoing need to plan for the unpredictable and unexpected. Emergencies are triggered by a variety of causes - like the weather, transport accidents and terrorism, to name just three. This Guide, produced by the Highlands and Islands Strategic Co-ordinating Group (SCG), provides basic information about what Government does and is doing to protect its population and what you can do to protect yourself and your family in the event of a major emergency. The Guide provides general information and the basic dos and don’ts in simple steps to prepare for such an emergency without unnecessary interruption to day to day activities. The SCG welcomes this opportunity to inform the public and hopes that the information in this guide provides useful help to improve your ability to respond to any emergency. Civil Contingencies Central Government’s approach to civil Resilience is built around several contingency planning is built around the key activities. -
List of Radio Stations in the United Kingdom - Wikipedia, the Free Encyclopedia List of Radio Stations in the United Kingdom from Wikipedia, the Free Encyclopedia
2014년 5월 8일 List of radio stations in the United Kingdom - Wikipedia, the free encyclopedia List of radio stations in the United Kingdom From Wikipedia, the free encyclopedia This is a list of radio stations in the United Kingdom: Contents 1 National analogue and digital stations 2 Semi-National analogue, digital & online stations 3 Local and regional stations 3.1 BBC Local Radio 3.2 BBC Regional Radio 3.3 Local Commercial Radio 3.3.1 England 3.3.2 Former English stations 3.3.3 Northern Ireland 3.3.4 Former Northern Irish stations 3.3.5 Scotland 3.3.6 Former Scottish stations 3.3.7 Wales 3.3.8 Former Welsh stations 3.3.9 The Channel Islands & the Isle of Man 4 Community radio stations 5 Former community radio stations 6 RSL stations 7 Student and schools radio 8 Hospital radio stations 9 Satellite radio stations 10 Other 11 Frequencies 12 See also 13 References 14 External links National analogue and digital stations This list does not include stations which broadcast on numerous local digital multiplexes or MW licences to achieve near-national coverage DAB Name Format FM Frequencies AM Frequencies Freeview Freesat Sky Virgin Channels 11D (England, adult- Wales and Absolute 1197, 1215, 1233, 1242, 1260 orientated 105.8 FM (London) Northern 727 724 0107 915 Radio MW pop/rock music Ireland) 12A (Scotland) 11D (England, Wales and Absolute Music from the Northern 726 0200 951 80s 1980s Ireland) 12A (Scotland) 11D (England, Absolute Wales and Music from the Radio Northern 0203 1990s 90s Ireland) 12A (Scotland) youth- BBC orientated pop 97.6