Winscombe Surgery Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

5 Sycamore Close Shipham, BS25 1TY
Non -printing text ignore if visible 5 Sycamore Close Shipham, BS25 1TY Non -printing text ignore if visible 5 Sycamore Close, Shipham, Winscombe, BS25 1TY Price: £3 55,000 Beautifully presented family home in tucked away location Contemporary kitchen with breakfast bar Very private, south facing gardens Additional study plus playroom Loads of parking, with garage In favoured Kings of Wessex school catchment DESCRIPTION An ideal property for a growing family, number 5 is tucked away in this lovely village, whilst We have noticed ... My vendors have cleverly organised a set of outline plans for being in walking distance to amenities and the local primary school. The property has been purchasers to look at, who might be interested in adding further accommodation. This will loved by the current owners who have brought their own children up her e and now after 37 be made available on viewings for inspection. years have decided that now is the time to downsize to something a bit smaller. Thus, lea ving the next chapter to begin for the next purchasers. SITUATION Comprising a gorgeous contemporary kitchen with breakfast bar, integrated dishwasher and Shipham is an Area of Outstanding Natural Beauty (AONB) and a highly sought after village, ceramic sink, a light, bright and stunningly presented sitting room, with feature log burner for nestled in the picturesque Somerset countryside. It is well served by first, middle and senior cosy nights in and doors leading directly out into the private sunny south facing garden. schools and is much sought after by those commuting to Bristol, as it offers all the advantages Upstairs there are three double bedrooms, a modern bathroom and space for potential to add of rural living with many bridleways and footpaths, inc luding the West Mendip Way which an ensuite. -

Cedar Barn Banwell North Somerset, BS29
Cedar Barn Banwell North Somerset, BS29 Cedar Barn Cedar barn is situated between the popular villages of Banwell and Sandford in a semi-rural se ing on the edge of the Mendip Hills, with very pre y views. A newly renovated linked barn conversion fi nished to a high andard throughout, with fl exible accommodation and o ering the perfe environment for family living and entertaining alike. The property boa s all the fi nishes Bristol 16 miles, Wells 15 miles, expe ed of a high quality and contemporary house with features such as under fl oor heating and fl oor to ceiling high doors opening M5 (J21) 2 miles, Bristol Airport 8 out from the fanta ic kitchen/dining living room to the garden miles, Bath 25 miles, Rail Station at we facing garden. Yatton 6 miles, Winscombe (3 miles) Weston-Super-Mare 5 miles (all One of two unique barn conversions, the property o ers acious distances are approximate). and comfortable living accommodation. The ground fl oor includes a fabulous double height kitchen/dining/living room with high Local Authority: quality appliances, under fl oor heating, fl ag one fl ooring and North Somerset District Council - sliding doors; a utility room and boiler room o the kitchen; three 01934 888 888. bathrooms, one of which is en suite, and a family bathroom. There are two aircases. One leads up from the kitchen/living Services: dining room to a reception room/bedroom with doors out to a Mains water and electricity. Air roof terrace, taking in the fanta ic views to the we . -
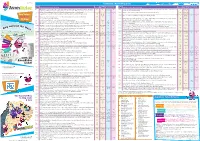
Tickets Are Accepted but Not Sold on This Service
May 2015 Guide to Bus Route Frequencies Route Frequency (minutes/journeys) Route Frequency (minutes/journeys) No. Route Description / Days of Operation Operator Mon-Sat (day) Eves Suns No. Route Description / Days of Operation Operator Mon-Sat (day) Eves Suns 21 Musgrove Park Hospital , Taunton (Bus Station), Monkton Heathfield, North Petherton, Bridgwater, Dunball, Huntspill, BS 30 1-2 jnys 60 626 Wotton-under-Edge, Kingswood, Charfield, Leyhill, Cromhall, Rangeworthy, Frampton Cotterell, Winterbourne, Frenchay, SS 1 return jny Highbridge, Burnham-on-Sea, Brean, Lympsham, Uphill, Weston-super-Mare Daily Early morning/early evening journeys (early evening) Broadmead, Bristol Monday to Friday (Mon-Fri) start from/terminate at Bridgwater. Avonrider and WestonRider tickets are accepted but not sold on this service. 634 Tormarton, Hinton, Dyrham, Doyton, Wick, Bridgeyate, Kingswood Infrequent WS 2 jnys (M, W, F) – – One Ticket... 21 Lulsgate Bottom, Felton, Winford, Bedminster, Bristol Temple Meads, Bristol City Centre Monday to Friday FW 2 jnys –– 1 jny (Tu, Th) (Mon-Fri) 635 Marshfield, Colerne, Ford, Biddestone, Chippenham Monday to Friday FS 2-3 jnys –– Any Bus*... 26 Weston-super-Mare , Locking, Banwell, Sandford, Winscombe, Axbridge, Cheddar, Draycott, Haybridge, WB 60 –– (Mon-Fri) Wells (Bus Station) Monday to Saturday 640 Bishop Sutton, Chew Stoke, Chew Magna, Stanton Drew, Stanton Wick, Pensford, Publow, Woollard, Compton Dando, SB 1 jny (Fri) –– All Day! 35 Bristol Broad Quay, Redfield, Kingswood, Wick, Marshfield Monday to Saturday -

Mendip Hills AONB Partnership Committee Draft Minutes of the Meeting at Ubley Parish Hall 21St March 2019
Mendip Hills AONB Partnership Committee Draft Minutes of the meeting at Ubley Parish Hall 21st March 2019 Present: Partnership Committee Cllr Liz Richardson (Vice Chair) Bath & North East Somerset Council Jim Hardcastle AONB Manager Cllr Mike Adams North Somerset Parish Representative Tom Lane Natural England Cllr Ann Harley North Somerset Council Ian Clemmett National Trust Richard Frost Mendip Society Pippa Rayner Somerset Wildlife Trust Steve Dury Somerset County Council Officer Cllr Roger Dollins Somerset Parishes Representative Becky Collier CPRE Other attendees Tim Haselden AONB Project Development Officer Sarah Catling AONB Support & Communications Officer Pete Douglas Somerset Wildlife Trust Apologies Di Sheppard Bath & North East Somerset Council Officer Chris Lewis CPRE Cllr Nigel Taylor (Chair) Somerset County Council Tim Curley Avon Wildlife Trust Cllr E Brimmell Bath & North East Somerset Council Parish Reps Julie Cooper Sedgemoor District Council Officer John Flannigan North Somerset Council Officer Cllr Tom Killen Mendip District Council Rachel Tadman Mendip District Council Officer Andy Wear National Farmers Union 1 Summary of Actions Item Item Notes Action 1 Declaration of No declarations Interest 2 Notes of Previous Accepted as a true and accurate record Meeting Proposer RD Seconder MA Apologies as stated. Tim Curley will now be representing Avon Wildlife Trust on the Partnership. 3 Paper A - OSG Additional points to note, RP is no longer the Mendip Report District Council Officer, Rachel Tadman has been appointed with immediate effect. Point 3 - Finance underspend resulting from the delayed delivery of the new vehicle has now been allocated to partnership working with Bristol Avon Rivers Trust on The Chew Headwaters Assessment Project and QGIS mapping. -

Here Needs Conserving and Enhancing
OS EXPLORER MAP OS EXPLORER MAP OS EXPLORER MAP OS EXPLORER MAP 141 141 154 153 GRID REFERENCE GRID REFERENCE GRID REFERENCE GRID REFERENCE A WILD LAND VISITOR GUIDE VISITOR ST 476587 ST466539 ST578609 ST386557 POSTCODE POSTCODE POSTCODE POSTCODE READY FOR BS40 7AU CAR PARK AT THE BOTTOM OF BS27 3QF CAR PARK AT THE BOTTOM BS40 8TF PICNIC AND VISITOR FACILITIES, BS25 1DH KINGS WOOD CAR PARK BURRINGTON COMBE OF THE GORGE NORTH EAST SIDE OF LAKE ADVENTURE BLACK DOWN & BURRINGTON HAM CHEDDAR GORGE CHEW VALLEY LAKE CROOK PEAK Courtesy of Cheddar Gorge & Caves This area is a very special part of Mendip.Open The internationally famous gorge boasts the highest Slow down and relax around this reservoir that sits in The distinctive peak that most of us see from the heathland covers Black Down, with Beacon Batch at inland limestone cliffs in the country. Incredible cave the sheltered Chew Valley. Internationally important M5 as we drive by. This is iconic Mendip limestone its highest point. Most of Black Down is a Scheduled systems take you back through human history and are for the birds that use the lake and locally loved by the countryside, with gorgeous grasslands in the summer ADVENTURE Monument because of the archaeology from the late all part of the visitor experience. fishing community. and rugged outcrops of stone to play on when you get Stone Age to the Second World War. to the top. Travel on up the gorge and you’ll be faced with Over 4000 ducks of 12 different varieties stay on READY FOR FOR READY Burrington Combe and Ham are to the north and adventure at every angle. -

FPS/G3300/14A/21 Decision Dated 21 November 2019
Appeal Decision by Susan Doran BA Hons MIPROW an Inspector appointed by the Secretary of State for Environment, Food and Rural Affairs Decision date: 21 November 2019 Appeal Ref: FPS/G3300/14A/21 • This Appeal is made under Section 53(5) and Paragraph 4(1) of Schedule 14 of the Wildlife and Countryside Act 1981 against the decision of Somerset County Council not to make an Order under Section 53(2) of that Act. • The Application dated 1 October 2015 was refused by Somerset County Council on 31 January 2019. • The Appellant claims that the appeal route should be added to the definitive map and statement for the area as a bridleway/restricted byway/byway open to all traffic. Decision 1. The appeal is dismissed. Preliminary Matters 2. I have been directed by the Secretary of State for Environment, Food and Rural Affairs to determine an appeal under Section 53(5) and Paragraph 4(1) of Schedule 14 of the Wildlife and Countryside Act 1981 (‘the 1981 Act’). 3. I have not visited the site but I am satisfied I can make my decision without the need to do so. 4. The appeal concerns an application made by Venetia Craggs on behalf of the Sedgemoor Byways and Bridleways Association, with submissions also made by Joanna Roseff (together referred to below as ‘the Appellant’). The application was made to add a bridleway/restricted byway/byway open to all traffic running from AX1/19 on the A38 Bridgwater Road to connect with AX29/37 and AX1/20 and connect with AX13/7 on the Shipham Road, known as Callow Drove (’the appeal route’). -

North Somerset Council Dog Control Order Consultation | Your Views
North Somerset Council Dog Control Order Consultation | your views Introduction Throughout June we asked you what you thought of new Dog Control Order proposals. The proposals were designed to replace existing and outdated by-laws (in many cases not changing their current status) and in conjunction with the Clean Neighbourhoods and Environment Act 2005. Prior to the consultation beginning, our Environmental Protection Officers met with local Town and Parish Councils to discuss what measures they would like to be suggested which is reflected in the proposals that were put forward. Areas involved Banwell, Recreation Grounds Portbury, Ponds Banwell, Scout Hut and Children’s Centre Portishead, Brampton Way Play Area Bleadon, Allotments Portishead, Marina Bleadon, Village Cross Area Redhill, Christchurch Churchyard Cleeve, King George V Playing Field Weston-super-Mare, St Georges Village Play Clevedon, Coleridge Vale Playing Fields Area Clevedon, Promenade Tickenham, Village Hall Field Felton, Vee Lane Playing Fields Weston-super-Mare, Clarence Park West Hutton, Phippen Park Weston-super-Mare, Promenade Locking, Village Allotments Winscombe, Longfield RFC Nailsea, Engine Lane Winscombe, War Memorial Recreation Ground Nailsea, Fryth Way Wrington, Glebe Field Nailsea, Greenfield Crescent Nailsea, Grove Playing Fields Your opinion In total 606 individual responses were received regarding the consultation. As each respondent could comment on more than one dog control order, there were 826 responses over all. Responses were captured through an online survey as well as through letters, emails, telephone calls, eConsult and petitions. To all that responded – thank you. Your comments will be taken into consideration when a decision is made later this year as to whether to implement the orders or make modifications. -

Winscombe Court Winscombe
Winscombe Court Winscombe Winscombe Court Winscombe Hill Winscombe North Somerset BS25 1DE ~ (Between Bristol, Wells and Wedmore) ~ Beautiful example of gothic revival architecture Over 8700 Sq. Ft of Accommodation Coach House Tennis Court & Heated Swimming Pool Potential to run a business (Subject to necessary consents) About the area The North Somerset village of Winscombe nestles in the beautiful Mendip countryside within commuting distance of Bristol. The village's atmosphere is one of bustling activity, with a variety of shops, professional of@ices and community facilities including church, doctor and primary school (www.winscombewoodborough.n-somerset.sch.uk). Winscombe is in the Churchill Academy and Sixth Form Centre (www.churchill.n- somerset.sch.uk) catchment area for secondary education, where there is also an excellent sports centre and dry ski slope nearby. Private sector schooling is also close by at Sidcot and further aield (Millield near Wells and Clifton College in Bristol). Country activities available within the area include horse-riding, walking on the Mendips and sailing on Axbridge Reservoir, and there are also several excellent golf courses in the area. The lovely cathedral city of Wells is a drive away, as is the famous beauty spot, Cheddar Gorge. As mentioned, Winscombe is within commuting distance of Bristol but also has good access to the seaside town of Weston-super-Mare and the M5 at junction 21 to travel north or junction 22 to travel south. Bristol International Drive is within a 15 minute drive and a mainline rail link to London, at Weston-super-Mare, is only 10 minutes’ drive away. -

Breeding Birds of the Strawberry Line (Vale of Winscombe Section)
BREEDING BIRDS OF THE STRAWBERRY LINE (VALE OF WINSCOMBE SECTION) By Dr. Lincoln Garland Introduction The Strawberry Line, or Cheddar Valley Railway Line, is a footpath/cycleway extending for 10 miles along a dismantled railway corridor between Yatton and Cheddar in North Somerset. It is deeply cherished by neighbouring communities and I am very fortunate to have lived alongside it for the last six years. Over this time, I have become increasingly familiar with its natural seasonal rhythms, including those of its birdlife, which are the subject of this article. During the COVID-19 lockdown, I decided to make use of my permissible daily exercise to record the distribution of the breeding birds on my particular ‘patch’ of the Strawberry Line - the Vale of Winscombe section. This stretch of the Strawberry Line breaches the picturesque Mendip Hills between Sandford Station and Shute Shelve Tunnel, passing through the village of Winscombe halfway across (Figure 1). I was partly inspired into action by what I perceived to be a particularly high abundance of birdlife along the Strawberry Line in contrast with neighbouring relatively intensively managed farmland and even compared with some local Ancient woodlands, where birdsong often seems conspicuous by its absence. As a consequence of the lockdown and associated reduction in noise pollution, multiple media stories have described how the pace of life slowed for many people, who in turn became increasingly cognizant of their natural surroundings, and in particular of birdsong and the psychologically healing (biophilic) effect that nature’s soundscape can have. In telling the story of the Strawberry Line’s birdlife I hope that I can provide an added layer of interest for locals and visitors, which might also help in these difficult times deliver an enhanced dose of Vitamin N or Nature’s Fix, to borrow the biophilic terminology of Richard Louv (2017) and Florence Williams (2017) respectively. -

By Hook Or by Crook…Around the Peak
Take time out Walk By hook or by Crook... around the Peak tart in King’s Wood Continue on the track Scar park where the which runs along the National Trust invites stone wall on your donations of £1. right. The views Dogs are welcome get better as you in the area but continue. Look owners should note out for Cheddar the ‘free-roaming reservoir in the cattle’ sign on the distance and for the gate. free-roaming ponies blocking the track! Go through the wooden gate at the The track will gradually back of the car park and get steeper again and you take the track on the will climb up a steep How to get there right going uphill. hill. When you reach the top you will see Start at map ref: Follow the Crook Peak. Here ST 422561 track through you can have a Car: the woodland well-earned picnic Park at the King’s continuing on while enjoying the Wood car park the right. It will extraordinary 360 off the A38 at gradually get degree views of the Winscombe Hill steeper until you North Somerset coast, reach a green at the Bus: the Somerset levels and top where glorious 126 Wells to across to Cheddar and views await. Weston-super-Mare Wells. 16 • North Somerset Life • AprilMonth 2014 Year Walk Take time out Route information Distance: 3 miles Difficulty: Some steep sections Crook Peak has been an important Duration: landmark and boundary since early 1.5 hours (including times. The origins of the name are picnic time) unclear. -

The Stratford Lane Roman Road and Other Early Routes on Mendip
Proc, Univ. Bristol Spelaeol. Soc, 1992 19 (2), 151-182 THE STRATFORD LANE ROMAN ROAD AND OTHER EARLY ROUTES ON MENDIP by R.G..I.WILLIAMS ABSTRACT The existence of the Stratford Lane Road was first suggested in 1906- Opinions have differed firstly as lo us course from Ihe Mendip hilltop into Ihe Chew Valley and secondly as to Us function. This road and some medieval mutes in the ure;i wliidi might have Roman or earlier origins are examined in detail in this paper which also queries Ihe theory that the River Chew was used to transport Roman lead. Fieldwork was aided by the study of documents dating from ihe .sixteenth century held locally and in Ihe United Stales »f America. Fresh information on some archaeological sites on Mendip is given, including newly identified round-barrows, old boundary stones, a pillow mound and Ihe boundary of a medieval warren. INTRODUCTION In all ages since the neolithic farming communities became settled there has been a need for both local communication between habitation sites and access to resources. The elaborately constructed wooden trackways, dated to the Neolithic, Bronze Age and Iron Age periods, found in the peat moors south of the Mendip Hills, suggest a planned communication system with connections to other areas. Iron Age settlement on Ihe central Mendip plateau in caves, enclosures and hill-forts is confined to the edges of the escarpment but there is a dispersed pattern of farmsteads in the surrounding valleys, There is evidence of bronze and iron working at these .sites but there was only a limited use of lead in the Iron Age. -

Land at Shipham Lane, Winscombe SITE ALLOCATIONS PLAN
Site : Land at Shipham Lane, Winscombe SITE ALLOCATIONS PLAN: FURTHER ASSESSMENT OF RESIDENTIAL SITES Site assessment process The purpose of the site assessment process is, through a combination of Housing and Economic Land Availability Assessment and Sustainability Appraisal techniques, to assess the suitability of potential housing sites to address the housing supply issue identified by the Inspector. The assessments will be formally considered by Executive Committee on 5 September 2017. Site address: Site details Site reference SAP Previous references HELAA 2014 ref HE1453. Site address/location Land off Shipham Lane, Winscombe Site area (ha) 1.26ha Previously developed (%) No Current land use Agricultural. Surrounding uses Residential to north and west; business uses to south at Slough Pit Farm. Development Pre-application Management status (any recent planning applications/consents) Green Belt (%) No Site Allocations Plan examination: Further assessment of residential sites: draft templates published 1 August in advance of formal consideration by Executive Committee 5 September 2017. Site : Land at Shipham Lane, Winscombe AONB (%) Part of site is in the AONB. Indicative capacity 28 based on pre-application. Site notes e.g. any change to boundary Site suitability Flood risk status (include Site not indicated to be within FZ 3. fluvial, tidal, and surface and drainage) Archaeology Potential for Roman archaeology to existing. Further investigations would be required. Heritage No constraint identified. Landscape (incl. character, Given location partly within AONB there is potential coalescence, and setting) for significant adverse impact. Ecology/ Environmental Strong hedgerow features likely to provide rich (Species/habitats’designations) ecological habitat. Potential for bat foraging on site. Transport and highways No major constraints identified although access issues may be present.