Triclosan [CAS 3380-34-5]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chemical Disinfectants for Biohazardous Materials (3/21)
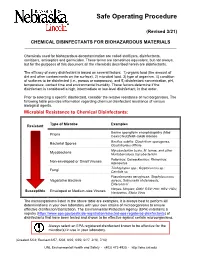
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Sodium Dodecyl Sulfate
Catalog Number: 102918, 190522, 194831, 198957, 811030, 811032, 811033, 811034, 811036 Sodium dodecyl sulfate Structure: Molecular Formula: C12H25NaSO4 Molecular Weight: 288.38 CAS #: 151-21-3 Synonyms: SDS; Lauryl sulfate sodium salt; Dodecyl sulfate sodium salt; Dodecyl sodium sulfate; Sodium lauryl sulfate; Sulfuric acid monododecyl ester sodium salt Physical Appearance: White granular powder Critical Micelle Concentration (CMC): 8.27 mM (Detergents with high CMC values are generally easy to remove by dilution; detergents with low CMC values are advantageous for separations on the basis of molecular weight. As a general rule, detergents should be used at their CMC and at a detergent-to-protein weight ratio of approximately ten. 13,14 Aggregation Number: 62 Solubility: Soluble in water (200 mg/ml - clear, faint yellow solution), and ethanol (0.1g/10 ml) Description: An anionic detergent3 typically used to solubilize8 and denature proteins for electrophoresis.4,5 SDS has also been used in large-scale phenol extraction of RNA to promote the dissociation of protein from nucleic acids when extracting from biological material.12 Most proteins bind SDS in a ratio of 1.4 grams SDS to 1 gram protein. The charges intrinsic to the protein become insignificant compared to the overall negative charge provided by the bound SDS. The charge to mass ratio is essentially the same for each protein and will migrate in the gel based only on protein size. Typical Working Concentration: > 10 mg SDS/mg protein Typical Buffer Compositions: SDS Electrophoresis -

A Review on Antimicrobial Resistance in Developing Countries
mac har olo P gy : & O y r p t e s i n Biochemistry & Pharmacology: Open A m c e c h e c Ravalli, et al. Biochem Pharmacol 2015, 4:2 s o i s B Access DOI: 10.4172/2167-0501.1000r001 ISSN: 2167-0501 Review Open Access A Review on Antimicrobial Resistance in Developing Countries Ravalli R1*, NavaJyothi CH2, Sushma B3 and Amala Reddy J4 1Deparment of Pharmaceutical Sciences, Andhra University, Vishakapatnam, India 2University College of Technology, Osmania University, Hyderabad, India 3Deparment of Medicinal Chemistry, National Institute of Pharmaceutical Education and Research (NIPER) Hyderabad, India 4Deparment of Pharmaceutical Sciences, Osmania University, Hyderabad, India *Corresponding author: Ravalli R, Deparment of Pharmaceutical Sciences, Andhra University, Vishakapatnam, India, Tel: + 0437-869-033; E-mail: [email protected] Received date: April 13, 2015; Accepted date: April 14, 2015; Published date: April 21, 2015 Copyright: © 2015 Ravalli Remella. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestri cted use, distribution, and reproduction in any medium, provided the original author and source are credited. Availability of Antimicrobial Drugs isolates were proof against Principen, Co-trimoxazole, and bactericide, and 14-40% were given with Mecillinam [6]. This was associate degree Although foremost potent and recently developed antimicrobial outsized increase over the half resistant isolates notable in 1991, before medicine are offered throughout the globe, in developing countries the drug was wide on the market. Throughout infectious disease their use is confined to people who are flush enough to afford them. In epidemics the organism has the flexibleness to develop increasing tertiary referral hospitals like the Kenyatta National Hospital in resistance, typically by acquisition of plasmids. -

Decontamination of Rooms, Medical Equipment and Ambulances Using an Aerosol of Hydrogen Peroxide Disinfectant B.M
Journal of Hospital Infection (2006) 62, 149–155 www.elsevierhealth.com/journals/jhin Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant B.M. Andersena,*, M. Rascha, K. Hochlina, F.-H. Jensenb, P. Wismarc, J.-E. Fredriksend aDepartment of Hospital Infection, Ulleva˚l University Hospital, Oslo, Norway bDivision of Pre-hospital Care, Ulleva˚l University Hospital, Oslo, Norway cDepartment of Medical Equipment, Ulleva˚l University Hospital, Oslo, Norway dHealth and Environment AS, Oslo, Norway Received 17 November 2004; accepted 1 July 2005 KEYWORDS Summary A programmable device (Sterinis, Gloster Sante Europe) Room decontamina- providing a dry fume of 5% hydrogen peroxide (H2O2) disinfectant was tion; Ambulance tested for decontamination of rooms, ambulances and different types of decontamination; medical equipment. Pre-set concentrations were used according to the Medical equipment decontamination; volumes of the rooms and garages. Three cycles were performed with Hydrogen peroxide increasing contact times. Repetitive experiments were performed using fume decontamina- Bacillus atrophaeus (formerly Bacillus subtilis) Raven 1162282 spores to tion; Spore test control the effect of decontamination; after a sampling plan, spore strips were placed in various positions in rooms, ambulances, and inside and outside the items of medical equipment. Decontamination was effective in 87% of 146 spore tests in closed test rooms and in 100% of 48 tests in a surgical department when using three cycles. One or two cycles had no effect. The sporicidal effect on internal parts of the medical equipment was only 62.3% (220 tests). When the devices were run and ventilated during decontamination, 100% (57/57) of spore strips placed inside were decontaminated. -

(12) United States Patent (10) Patent No.: US 7.427.405 B2 Agrawal Et Al
USOO7427405B2 (12) United States Patent (10) Patent No.: US 7.427.405 B2 Agrawal et al. (45) Date of Patent: Sep. 23, 2008 (54) IMMUNOSTIMULATORY Tokunaga et al., “Antitumor Activity of Deoxyribonucleic Acid Frac OLGONUCLEOTDE MULTIMERS tion from Mycobaterium bovis BCG. I. Isolation. Physicochemical Characterization, and Antitumor Activity”. J. Natl. Cancer Inst. 72: (75) Inventors: Sudhir Agrawal, Shrewsbury, MA (US); 955-962(1984). Pisetsky et al., “Stimulation of in vitro proliferation of murine lym Ekambar Kandimala, Southboro, MA phocytes by synthetic oligodeoxynucleotides'. Molecular Biology (US); Dong Yu, Westboro, MA (US) Reports 18:217-221 (1993). Krieg et al., “CpG motifs in bacterial DNA trigger direct B-cell (73) Assignee: Idera Pharmaceuticals, Inc., activation”, Nature 374: 546-549 (1995). Cambridge, MA (US) Sato et al., “Immunostimulatory DNA Sequence Necessary for Effective Intradermal Gene Immunization', Science 273: 352-354 (*) Notice: Subject to any disclaimer, the term of this (1996). patent is extended or adjusted under 35 Krieg et al., “CpG Motifs in Bacterial DNA and their Immune U.S.C. 154(b) by 209 days. Effects”, Annu. Rev. Immunol. 20: 709-760 (2002). Dalpke et al., “Immunopharmacology of CpG DNA'. Biol. Chem. (21) Appl. No.: 11/174,282 383: 1491-1500 (2002). Kandimala et al., “Towards Optimal Design of Second-Generation (22) Filed: Jul. 1, 2005 Immunomodulatory Oligonucleotides'. Curr. Opin. Mol. Ther. 4(2): 122-129 (2002). (65) Prior Publication Data Kandimala et al., “Immunomers-novel 3'-3'-Linked CpG Oligodeoxyribonucleotides as Potent Immunomodulatory Agents'. US 2006/OO19919 A1 Jan. 26, 2006 Nucleic Acids Res. 30: 4460-4469 (2002). Kandimala et al. -
Mankocide® Fungicide/Bactericide
SAFETY DATA SHEET Issue Date 25-Feb-2017 Revision Date 25-Feb-2017 Version 1 1. IDENTIFICATION Product identifier Product Name ManKocide® Fungicide/Bactericide Other means of identification Product Code 91411-7 Synonyms ManKocide DF, B12262770 Registration Number(s) 91411-7-70051 Recommended use of the chemical and restrictions on use Recommended Use Fungicide Bactericide Uses advised against No information available Details of the supplier of the safety data sheet Manufacturer Address Distributed by: Kocide LLC Certis U.S.A. L.L.C. 9145 Guilford Road, Suite 175 9145 Guilford Road, Suite 175 Columbia, MD 21046 Columbia, MD 21046 USA USA Website: www.kocide.com www.certisusa.com Emergency telephone number Company Phone Number Certis USA +1 301-604-7340 Emergency Telephone ChemTel, Inc.: 1-800-255-3924 (outside the U.S. 1-813-248-0585) POISON CONTROL CENTER: 800-222-1222 2. HAZARDS IDENTIFICATION Classification OSHA Regulatory Status This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute toxicity - Oral Category 4 Acute toxicity - Inhalation (Dusts/Mists) Category 4 Serious eye damage/eye irritation Category 1 Skin sensitization Category 1 Carcinogenicity Category 1A Reproductive toxicity Category 2 Label elements Emergency Overview Danger Hazard statements Harmful if swallowed Harmful if inhaled Causes serious eye damage May cause an allergic skin reaction May cause cancer Suspected of damaging fertility or the unborn child _____________________________________________________________________________________________ -

National Center for Toxicological Research
National Center for Toxicological Research Annual Report Research Accomplishments and Plans FY 2015 – FY 2016 Page 0 of 193 Table of Contents Preface – William Slikker, Jr., Ph.D. ................................................................................... 3 NCTR Vision ......................................................................................................................... 7 NCTR Mission ...................................................................................................................... 7 NCTR Strategic Plan ............................................................................................................ 7 NCTR Organizational Structure .......................................................................................... 8 NCTR Location and Facilities .............................................................................................. 9 NCTR Advances Research Through Outreach and Collaboration ................................... 10 NCTR Global Outreach and Training Activities ............................................................... 12 Global Summit on Regulatory Science .................................................................................................12 Training Activities .................................................................................................................................14 NCTR Scientists – Leaders in the Research Community .................................................. 15 Science Advisory Board ................................................................................................... -
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic
Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic Vickie Leonard, PhD Environmental Health in Early Care and Educaon Project, Western States Pediatric Environmental Health Specialty Unit (WSPEHSU) 1 Why Should We Be Concerned about Environmental Health in ECE? 2 Why Should We Be Concerned about Environmental Health in ECE? • There are 8 million children in child care centers in the U.S. A child may spend up to 12,500 hours in an ECE facility. A million child care providers work in these centers in the U.S. Half are child-bearing age. • Many toxicants found in child care facilities are not addressed in state child care health and safety regulations. • No agency at the state or federal level is charged with ensuring children’s health and safety in and around schools and ECE facilities. • No systematic means exists for collecting data on environmental exposures in these buildings. • Teachers have more protection in these buildings (unions, OSHA) than children do 3 Why Should We Be Concerned about Environmental Health in ECE? • Many people think that adults and children are exposed to, and affected by, toxic chemicals in the same way. • This is not the case. • Children • have higher exposures to toxicants in the environment, • are more vulnerable to the effects of those toxicants than adults. 4 Cleaning and Disinfec?ng Products: A Major Source of Exposure in Child Care and Schools • Products used to clean, sanitize and disinfect child care facilities and schools are a good example of the pervasive and unregulated use of toxic chemicals that put the health of our children at risk. -
Tutorial on Working with Micelles and Other Model Membranes
Tutorial on Working with Micelles and Model Membranes Chuck Sanders Dept. of Biochemistry, Dept. of Medicine, and Center for Structural Biology Vanderbilt University School of Medicine. http://structbio.vanderbilt.edu/sanders/ March, 2017 There are two general classes of membrane proteins. This presentation is on working with integral MPs, which traditionally could be removed from the membrane only by dissolving the membrane with detergents or organic solvents. Multilamellar Vesicles: onion-like assemblies. Each layer is one bilayer. A thin layer of water separates each bilayer. MLVs are what form when lipid powders are dispersed in water. They form spontaneously. Cryo-EM Micrograph of a Multilamellar Vesicle (K. Mittendorf, C. Sanders, and M. Ohi) Unilamellar Multilamellar Vesicle Vesicle Advances in Anesthesia 32(1):133-147 · 2014 Energy from sonication, physical manipulation (such as extrusion by forcing MLV dispersions through filters with fixed pore sizes), or some other high energy mechanism is required to convert multilayered bilayer assemblies into unilamellar vesicles. If the MLVs contain a membrane protein then you should worry about whether the protein will survive these procedures in folded and functional form. Vesicles can also be prepared by dissolving lipids using detergents and then removing the detergent using BioBeads-SM dialysis, size exclusion chromatography or by diluting the solution to below the detergent’s critical micelle concentration. These are much gentler methods that a membrane protein may well survive with intact structure and function. From: Avanti Polar Lipids Catalog Bilayers can undergo phase transitions at a critical temperature, Tm. Native bilayers are usually in the fluid (liquid crystalline) phase. -

Journal of Arthroscopy and Joint Surgery 6 (2019) 98E102
Journal of Arthroscopy and Joint Surgery 6 (2019) 98e102 Contents lists available at ScienceDirect Journal of Arthroscopy and Joint Surgery journal homepage: www.elsevier.com/locate/jajs Comparative evaluation of periarticular infiltration of two cocktail regimens for analgesia in post-operative patients of total knee replacement * V.K. Gautam a, Ajeet Kumar a, Munisha Agarwal b, Bushu Harna a, , Rishabh Saini a, Siddharth Sharma a, Dhananjaya Sabat a a Dept. of Orthopaedics, Maulana Azad Medical College, New Delhi, India b Dept. of Anaesthesia, Maulana Azad Medical College, New Delhi, India article info abstract Article history: Purpose: To compare the efficacy of two periarticular cocktail regimens for analgesia in postoperative Received 30 April 2018 patients of total knee replacement. Received in revised form Method: This is a Randomized Control study done over the duration of 1.5 years. Twenty-five knees of 28 October 2018 either gender were selected with inclusion criteria (All osteoarthritis patients planned for TKA) and Accepted 9 November 2018 exclusion criteria (Inflammatory arthritis, patients allergic to local anaesthetic e.g. Ropivacaine, bupi- Available online 19 November 2018 vacaine, known cardiac disorder patient having AV block, arrhythmia) & divided into 2 groups. Group A was given a cocktail of Ropivacaine, adrenaline, clonidine & cefuroxime. Keywords: & Periarticular Group B was given a cocktail of bupivacaine, fentanyl, methylprednisolone cefuroxime. The preoper- Multimodal approach ative pain of the patient was assessed using VAS score. Combined spinal and epidural anaesthesia was Perioperative analgesia given using 0.5% 2 ml of bupivacaine heavy in all patients. After taking bone cuts & before the placement Corticosteroids of the implant, cocktail of the drug was infiltrated using sterile technique into 9 specific sites. -

A Screening-Based Approach to Circumvent Tumor Microenvironment
JBXXXX10.1177/1087057113501081Journal of Biomolecular ScreeningSingh et al. 501081research-article2013 Original Research Journal of Biomolecular Screening 2014, Vol 19(1) 158 –167 A Screening-Based Approach to © 2013 Society for Laboratory Automation and Screening DOI: 10.1177/1087057113501081 Circumvent Tumor Microenvironment- jbx.sagepub.com Driven Intrinsic Resistance to BCR-ABL+ Inhibitors in Ph+ Acute Lymphoblastic Leukemia Harpreet Singh1,2, Anang A. Shelat3, Amandeep Singh4, Nidal Boulos1, Richard T. Williams1,2*, and R. Kiplin Guy2,3 Abstract Signaling by the BCR-ABL fusion kinase drives Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ ALL) and chronic myelogenous leukemia (CML). Despite their clinical activity in many patients with CML, the BCR-ABL kinase inhibitors (BCR-ABL-KIs) imatinib, dasatinib, and nilotinib provide only transient leukemia reduction in patients with Ph+ ALL. While host-derived growth factors in the leukemia microenvironment have been invoked to explain this drug resistance, their relative contribution remains uncertain. Using genetically defined murine Ph+ ALL cells, we identified interleukin 7 (IL-7) as the dominant host factor that attenuates response to BCR-ABL-KIs. To identify potential combination drugs that could overcome this IL-7–dependent BCR-ABL-KI–resistant phenotype, we screened a small-molecule library including Food and Drug Administration–approved drugs. Among the validated hits, the well-tolerated antimalarial drug dihydroartemisinin (DHA) displayed potent activity in vitro and modest in vivo monotherapy activity against engineered murine BCR-ABL-KI–resistant Ph+ ALL. Strikingly, cotreatment with DHA and dasatinib in vivo strongly reduced primary leukemia burden and improved long-term survival in a murine model that faithfully captures the BCR-ABL-KI–resistant phenotype of human Ph+ ALL.