Introduction to the Respiratory System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -
Inhalation Devices: Various Forms of Administration for Therapeutic Optimization
vv ISSN: 2640-8082 DOI: https://dx.doi.org/10.17352/oja CLINICAL GROUP Renata Cristina de Angelo Calsaverini Leal* Review Article Santa Fé do Sul Foundation of Education and Culture, Brazil Inhalation Devices: Various forms Dates: Received: 31 May, 2017; Accepted: 26 June, of administration for Therapeutic 2017; Published: 27 June, 2017 *Corresponding author: Renata Cristina de Angelo Optimization Calsaverini Leal, Santa Fé do Sul Foundation of Education and Culture, Brazil, Tel: 55 (17) 3272-2769, E-mail: Keywords: Inhalation; Aerosol; Nebulizer Summary https://www.peertechz.com Introduction: Aerosol therapy consists of spraying liquid particles suspended for therapeutic purposes in the respiratory tract. With direct absorption and deposition at the lung level, avoiding side effects and presenting fast response time. Several factors infl uence the drug action, such as size, particle movement, ventilatory fl ow, pulmonary expansion, anatomy, respiratory mechanics and the nebulizer and patient interface. The therapeutic optimization depends on the type of nebulizer differentiating itself by the physical principle that generates the mist. Objectives: Check advantages and disadvantages of different inhalation devices. Methodology. This is a review of the PubMed database using descriptors: ultrasonic and jet nebulizer, aerosol deposition in the lung, metered dose inhaler and dry, inhaler therapy. Results: Different devices are mentioned in the literature: pneumatic and ultrasonic nebulizers (administering solutions), metered pressurized inhalers - pMDI used with or without expander chamber (administering suspensions) and dry powder inhalers - DPI (administering powder). Discussion and Conclusion: The US has advantages: quiet, does not require coordinating abilities, without propellant gases and quick nebulization with small amount of solution. Disadvantages: change in the active principle of thermosensitive drugs, deposition in the oropharynx and VAI of 2% of inhaled particles. -

Larynx Anatomy
LARYNX ANATOMY Elena Rizzo Riera R1 ORL HUSE INTRODUCTION v Odd and median organ v Infrahyoid region v Phonation, swallowing and breathing v Triangular pyramid v Postero- superior base àpharynx and hyoid bone v Bottom point àupper orifice of the trachea INTRODUCTION C4-C6 Tongue – trachea In women it is somewhat higher than in men. Male Female Length 44mm 36mm Transverse diameter 43mm 41mm Anteroposterior diameter 36mm 26mm SKELETAL STRUCTURE Framework: 11 cartilages linked by joints and fibroelastic structures 3 odd-and median cartilages: the thyroid, cricoid and epiglottis cartilages. 4 pair cartilages: corniculate cartilages of Santorini, the cuneiform cartilages of Wrisberg, the posterior sesamoid cartilages and arytenoid cartilages. Intrinsic and extrinsic muscles THYROID CARTILAGE Shield shaped cartilage Right and left vertical laminaà laryngeal prominence (Adam’s apple) M:90º F: 120º Children: intrathyroid cartilage THYROID CARTILAGE Outer surface à oblique line Inner surface Superior border à superior thyroid notch Inferior border à inferior thyroid notch Superior horns à lateral thyrohyoid ligaments Inferior horns à cricothyroid articulation THYROID CARTILAGE The oblique line gives attachement to the following muscles: ¡ Thyrohyoid muscle ¡ Sternothyroid muscle ¡ Inferior constrictor muscle Ligaments attached to the thyroid cartilage ¡ Thyroepiglottic lig ¡ Vestibular lig ¡ Vocal lig CRICOID CARTILAGE Complete signet ring Anterior arch and posterior lamina Ridge and depressions Cricothyroid articulation -

Respiratory System
Respiratory system Department of Histology and Embryology of Jilin university ----Jiang Wenhua 1. General description z the nose, the pharynx, the larynx, the trachea, bronchus, lung zFunction: inspiring oxygen, expiring carbon dioxide The lung synthesises many materials 2.Trachea and bronchi General structure mucosa submucosa adventitia The trachea is a thin-walled tube about 11centimeters long and 2 centimeters in diameter, with a somewhat flattened posterior shape. The wall of the trachea is composed of three layers: mucosa, submucosa, and adventitia 2.1 mucosa 2.1.1 pseudostratified ciliated columnar epithelium 2.1.1.1 ciliated columnar cells These cells are columnar in shape with a centrally –located oval –shaped nucleus, on the free surface of the cells are microvilli and cilia, which regularly sweep toward the pharynx to remove inspired dust particles 2.1.1.2 brush cells These cells are columnar in shape with a round or oval –shaped nucleus located in the basal portion. on the free surface the microvilli are arranged into the shape of a brush. These cells are considered to be a type of under-developed ciliated columnar cell Schematic drawing of the trachea mucosa Scanning electron micrographs of the surface of mucosa Schematic drawing of the trachea mucosa 2.1.1.3 goblet cells secrete mucus to lubricate and protect the epithelium Schematic drawing of the trachea mucosa 2.1.1.4 basal cells These cells are cone –shaped and situated in the deep layer of the epithelium. Their apices are not exposed to the lumen, and their nuclei are round in shape, such cells constitute a variety of undifferentiated cells 2.1.1.5 small granular cells These cells are a kind of endocrine cells . -

How the Larynx (Voice Box) Works
How the Larynx (Voice Box) Works Charles R. Larson, PhD If you love opera, or if you admire the voices of pop singers such as Celine Dion or Barbra Streisand, you may have wondered how it is these marvelous singers are able to create such beautiful music with this instrument we call the human voice. You may also know of someone who has a bad voice or has had to have their voice box, or larynx, removed because of illness or injury. The larynx is a critical organ of human speech and singing, and it serves important biological functions as well. Let's have a look at the larynx to understand its functions, what it looks like and how it works. It is thought that the same factors that favored the evolution of air‐breathing animals on earth led to the evolution of the larynx. Lungs are comprised of very delicate tissues that must be maintained within strict biological limits, that is, temperature, humidity and freedom from foreign particles. Thus, along with the first air‐breathing animals, there appeared a primitive sort of larynx, whose one and only function was protection of the lung. This function remains the most important of those the larynx has assumed in subsequent evolutionary developments. Now, of course we recognize that the larynx is critical for human speech and singing. But we also should realize that the larynx is important for swallowing, coughing, vomiting and eliminating contents of the abdomen. If you have ever felt your 'Adam's Apple', then you know where the larynx is. -

1. Launch the View! • Launch Human Anatomy Atlas. • Navigate to Quizzes/Lab Activities, Find the Respiratory Lab Section
Name: __________________________________________________________ Date: ______________________________ Activity 1: Respiratory System Lab 1. Launch the view! • Launch Human Anatomy Atlas. • Navigate to Quizzes/Lab Activities, find the Respiratory Lab section. • Launch Augmented Reality mode and scan the image below. • Don’t have AR? Select view 1. Respiratory System. 2. Fill in the blanks. • Find the structures listed in the word bank. • Read the definitions, then fill in the blank with the correct respiratory system structure from the word bank. © Argosy Publishing, Inc., 2007-2018. All Rights Reserved. 1/2 Name: __________________________________________________________ Date: ______________________________ Word bank: • Alveoli • Nasopharynx • Bronchi • Oropharynx • Laryngopharynx • Primary bronchi • Lungs • Trachea • Nasal cavity The ______________________________ is composed of the chambers of the internal nose that function as a part of the upper respiratory system. The ______________________________ is the most posterior part of the pharynx. It is shared by the respiratory system and the digestive system. The upper respiratory and upper digestive tracts diverge right after this structure. The front of this structure merges with the triangular entrance of the larynx. The ______________________________ conveys air between the upper and lower respiratory structures. The ______________________________ is a portion of the pharynx that begins at the rear of the nasal cavity and functions as an airway in the upper respiratory system. Its cavity always stays open, unlike the other parts of the pharynx. The ______________________________ are two organs that are responsible for gas exchange. The ______________________________ are the major airways of the lower respiratory system. The ______________________________ are the main sites of gas exchange, where oxygen is brought into the bloodstream and carbon dioxide is removed. -
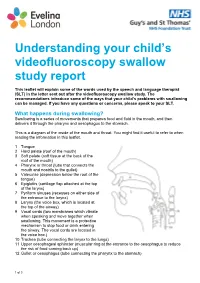
Understanding Your Child's Videofluoroscopy
Understanding your child’s videofluoroscopy swallow study report This leaflet will explain some of the words used by the speech and language therapist (SLT) in the letter sent out after the videofluoroscopy swallow study. The recommendations introduce some of the ways that your child’s problems with swallowing can be managed. If you have any questions or concerns, please speak to your SLT. What happens during swallowing? Swallowing is a series of movements that prepares food and fluid in the mouth, and then delivers it through the pharynx and oesophagus to the stomach. This is a diagram of the inside of the mouth and throat. You might find it useful to refer to when reading the information in this leaflet. 1 Tongue 2 Hard palate (roof of the mouth) 3 Soft palate (soft tissue at the back of the roof of the mouth) 4 Pharynx or throat (tube that connects the mouth and nostrils to the gullet) 5 Valeculae (depression below the root of the tongue) 6 Epiglottis (cartilage flap attached at the top of the larynx) 7 Pyriform sinuses (recesses on either side of the entrance to the larynx) 8 Larynx (the voice box, which is located at the top of the airway) 9 Vocal cords (two membranes which vibrate when speaking and move together when swallowing. This movement is a protective mechanism to stop food or drink entering the airway. The vocal cords are located in the voice box.) 10 Trachea (tube connecting the larynx to the lungs) 11 Upper oesophageal sphincter (muscular ring at the entrance to the oesophagus to reduce the risk of food coming back up) 12 Gullet or oesophagus (tube connecting the pharynx to the stomach) 1 of 3 Swallowing phases Swallowing involves three phases: 1. -

Cricoid Pressure: Ritual Or Effective Measure?
R eview A rticle Singapore Med J 2012; 53(9) 620 Cricoid pressure: ritual or effective measure? Nivan Loganathan1, MB BCh BAO, Eugene Hern Choon Liu1, MD, FRCA ABSTRACT Cricoid pressure has been long used by clinicians to reduce the risk of aspiration during tracheal intubation. Historically, it is defined by Sellick as temporary occlusion of the upper end of the oesophagus by backward pressure of the cricoid cartilage against the bodies of the cervical vertebrae. The clinical relevance of cricoid pressure has been questioned despite its regular use in clinical practice. In this review, we address some of the controversies related to the use of cricoid pressure. Keywords: cricoid pressure, regurgitation Singapore Med J 2012; 53(9): 620–622 INTRODUCTION imaging showed that in 49% of patients in whom cricoid Cricoid pressure is a technique used worldwide to reduce pressure was applied, the oesophageal position was lateral to the risk of aspiration during tracheal intubation in sedated or the cricoid ring.(5) As oesophageal occlusion was thought to be anaesthetised patients. Cricoid pressure can be traced back to crucial, this study challenged the efficacy of cricoid pressure. the late 18th century when it was used to prevent gas inflation More recently, in magnetic resonance imaging studies, Rice et of the stomach during resuscitation from drowning.(1) Sellick al showed that cricoid pressure causes compression of the post- noted that cricoid pressure could both prevent regurgitation cricoid hypopharynx rather than the oesophagus itself. -

Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-Tailed Opossum (Monodelphis Domestica) and North American Opossum (Didelphis Virginiana)
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 12-2001 Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana) Lee Anne Cope University of Tennessee - Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Animal Sciences Commons Recommended Citation Cope, Lee Anne, "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana). " PhD diss., University of Tennessee, 2001. https://trace.tennessee.edu/utk_graddiss/2046 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Lee Anne Cope entitled "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana)." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Animal Science. Robert W. Henry, Major Professor We have read this dissertation and recommend its acceptance: Dr. R.B. Reed, Dr. C. Mendis-Handagama, Dr. J. Schumacher, Dr. S.E. Orosz Accepted for the Council: Carolyn R. -

Larynx 2017‐2018 Naaccr Webinar Series
NAACCR 2017-2018 Webinar Series 11/2/2017 COLLECTING CANCER DATA: LARYNX 2017‐2018 NAACCR WEBINAR SERIES Q&A • Please submit all questions concerning webinar content through the Q&A panel. • Reminder: • If you have participants watching this webinar at your site, please collect their names and emails. • We will be distributing a Q&A document in about one week. This document will fully answer questions asked during the webinar and will contain any corrections that we may discover after the webinar. 2 Larynx 1 NAACCR 2017-2018 Webinar Series 11/2/2017 Fabulous Prizes 3 AGENDA • Anatomy • Epi Moment • Quiz 1 • Staging • Treatment • Quiz 2 • Case Scenarios 4 Larynx 2 NAACCR 2017-2018 Webinar Series 11/2/2017 ANATOMY LARYNX 5 LARYNX ANATOMY • Voice Box • Passageway of air • Extends from C3 to C6 vertebrae 6 Larynx 3 NAACCR 2017-2018 Webinar Series 11/2/2017 LARYNX ANATOMY • Divided into 3 Sections • Supraglottis • area above vocal cords, contains epiglottis • arytenoids, aryepiglottic folds and false cords • Glottis • containing true vocal cords, anterior and posterior commissures • Subglottis • below the vocal cords 7 LARYNX ANATOMY • Epiglottis • Aryepiglottic Folds • Anterior and Posterior • False vocal cords Commissure • True vocal cords • Arytenoids 8 Larynx 4 NAACCR 2017-2018 Webinar Series 11/2/2017 LARYNX ANATOMY • Thyroid cartilage • Arytenoid cartilage • Adam’s apple • Influence position and tension of the • Thyrohyoid membrane vocal cords • Cricoid cartilage • Corniculate cartilage • Inferior wall of larynx • Horn shaped pieces located -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists.