Internal Medicine/Reproduction Proceedings 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PIS the E-BARQ Questionnaire Will Take Approximately 20
05/10/2020 Qualtrics Survey Software English PIS The E-BARQ questionnaire will take approximately 20 - 30 minutes to complete. E-BARQ is voluntary and your information is confidential. If you answer all of the questions, you will receive a Share-&-Compare graph on completion. This graph will show you where your horse compares to the population on 14 different categories, including Trainability, Rideability, Social Confidence and so on. Please respond to all questions to receive your graph (which can be found on your E-BARQ dashboard (under the E-BARQ Results tab) , immediately on completion). Please click here to download the E-BARQ personal information statement. I have read and agreed to the Personal Information Statement and Terms and Conditions of the E-BARQ project. Yes No (this option will remove you from E-BARQ) https://sydney.qualtrics.com/Q/EditSection/Blocks/Ajax/GetSurveyPrintPreview?ContextSurveyID=SV_3dVyqziNawK514h&ContextLibraryID=U… 1/85 05/10/2020 Qualtrics Survey Software Your email address registered: ${e://Field/user} Is this your FIRST time completing an E-BARQ questionnaire? Select 'No' if you already have an E-BARQ Dashboard (have completed an E-BARQ for another horse). Yes No, I have completed an E-BARQ previously 1st E-BARQ Demographics Are you? In which country do you reside? https://sydney.qualtrics.com/Q/EditSection/Blocks/Ajax/GetSurveyPrintPreview?ContextSurveyID=SV_3dVyqziNawK514h&ContextLibraryID=U… 2/85 05/10/2020 Qualtrics Survey Software What is your age? Are you RIGHT or LEFT handed? Demographics Your horse's name: ${e://Field/horsename} Your horse's E-BARQ ID: ${e://Field/ebarqid} You are welcome to complete one E-BARQ for each horse that you own but this survey will refer only to the horse named here. -

List of Horse Breeds 1 List of Horse Breeds
List of horse breeds 1 List of horse breeds This page is a list of horse and pony breeds, and also includes terms used to describe types of horse that are not breeds but are commonly mistaken for breeds. While there is no scientifically accepted definition of the term "breed,"[1] a breed is defined generally as having distinct true-breeding characteristics over a number of generations; its members may be called "purebred". In most cases, bloodlines of horse breeds are recorded with a breed registry. However, in horses, the concept is somewhat flexible, as open stud books are created for developing horse breeds that are not yet fully true-breeding. Registries also are considered the authority as to whether a given breed is listed as Light or saddle horse breeds a "horse" or a "pony". There are also a number of "color breed", sport horse, and gaited horse registries for horses with various phenotypes or other traits, which admit any animal fitting a given set of physical characteristics, even if there is little or no evidence of the trait being a true-breeding characteristic. Other recording entities or specialty organizations may recognize horses from multiple breeds, thus, for the purposes of this article, such animals are classified as a "type" rather than a "breed". The breeds and types listed here are those that already have a Wikipedia article. For a more extensive list, see the List of all horse breeds in DAD-IS. Heavy or draft horse breeds For additional information, see horse breed, horse breeding and the individual articles listed below. -

Electronic Supplementary Material - Appendices
1 Electronic Supplementary Material - Appendices 2 Appendix 1. Full breed list, listed alphabetically. Breeds searched (* denotes those identified with inherited disorders) # Breed # Breed # Breed # Breed 1 Ab Abyssinian 31 BF Black Forest 61 Dul Dülmen Pony 91 HP Highland Pony* 2 Ak Akhal Teke 32 Boe Boer 62 DD Dutch Draft 92 Hok Hokkaido 3 Al Albanian 33 Bre Breton* 63 DW Dutch Warmblood 93 Hol Holsteiner* 4 Alt Altai 34 Buc Buckskin 64 EB East Bulgarian 94 Huc Hucul 5 ACD American Cream Draft 35 Bud Budyonny 65 Egy Egyptian 95 HW Hungarian Warmblood 6 ACW American Creme and White 36 By Byelorussian Harness 66 EP Eriskay Pony 96 Ice Icelandic* 7 AWP American Walking Pony 37 Cam Camargue* 67 EN Estonian Native 97 Io Iomud 8 And Andalusian* 38 Camp Campolina 68 ExP Exmoor Pony 98 ID Irish Draught 9 Anv Andravida 39 Can Canadian 69 Fae Faeroes Pony 99 Jin Jinzhou 10 A-K Anglo-Kabarda 40 Car Carthusian 70 Fa Falabella* 100 Jut Jutland 11 Ap Appaloosa* 41 Cas Caspian 71 FP Fell Pony* 101 Kab Kabarda 12 Arp Araappaloosa 42 Cay Cayuse 72 Fin Finnhorse* 102 Kar Karabair 13 A Arabian / Arab* 43 Ch Cheju 73 Fl Fleuve 103 Kara Karabakh 14 Ard Ardennes 44 CC Chilean Corralero 74 Fo Fouta 104 Kaz Kazakh 15 AC Argentine Criollo 45 CP Chincoteague Pony 75 Fr Frederiksborg 105 KPB Kerry Bog Pony 16 Ast Asturian 46 CB Cleveland Bay 76 Fb Freiberger* 106 KM Kiger Mustang 17 AB Australian Brumby 47 Cly Clydesdale* 77 FS French Saddlebred 107 KP Kirdi Pony 18 ASH Australian Stock Horse 48 CN Cob Normand* 78 FT French Trotter 108 KF Kisber Felver 19 Az Azteca -

Headshaking Common Problems by Dr John Kohnke Bvsc RDA Fact Sheet 33
C33 Headshaking Common Problems By Dr John Kohnke BVSc RDA Fact Sheet 33 Headshaking can be a difficult problem to diagnose and manage. around the globe have been able to shed some light on this type of Research has shown that the incidence is increasing in horses headshaking in horses. Researchers in the UK suggested in 2000 between 6 and 12 years of age. that the behaviour is due to increased sensitivity in the trigeminal nerve which provides sensation to the upper face, nose and muzzle Headshaking was first described almost 200 years ago. It is areas. Local anaesthesia of the rear nasal branch (maxillary) of the characterised by an uncontrollable, often repetitive vertical and trigeminal nerve in the studies resulted in an 80-100% reduction horizontal (head nodding) or rotary movement of the head and in clinical signs in most headshakers. The researchers also found neck, often without any obvious external cause or stimuli. Some that fitting a nasal filtering mask to slow the air entering the nostrils horses also rub their face and nostrils, often on the front legs or on and inhalation of particulate matter can reduce the signs of fences. A number of affected horses might also snort regularly and headshaking by 90-100% in most headshakers. However, when the these horses often have mild nasal discharge. Some horses exhibit mask is removed, the symptoms often return. This supports the only mild or intermittent symptoms, others develop a frequent, theory that there is a trigger zone in the rear nasal cavity. violent headshaking habit with the appearance of distress. -

Published in ” Natural Horse 3, 44-47, 2001 Volume 3, Issue 6
Published in ” Natural Horse 3, 44-47, 2001 Volume 3, Issue 6 – Equissentials Photo: (bitless bridle?) TITLE: Who Needs Bits? With Dr. W. Robert Cook In today's horse world, we have a delightful trend toward keeping it natural while at the same time 'unnaturally' riding these powerful animals that once roamed free. Their natural instincts remain, but their amiable natures allow us to harness their power and enjoy the pleasure of their company. Riding or driving these magnificent creatures involves the risk of causing them harm by using, for example, ill-fitting saddles and harness. The knowledge we have gained from research, however, has enabled us to choose our equipment more wisely, with the horse's best interests in mind. Another area of equipment that has been researched is the bridle, or more particularly, the bit. The snaffle bit has come to be accepted as kind, with shank and port bits being regarded as unkind. But do we need a bit at all? When we have the likes of Pat Parelli and Robin Brueckmann achieving Olympic level riding without even a bridle, who needs bits? Furthermore, do bits actually cause harm? Veterinarian and researcher Dr. W. Robert Cook has uncovered some very interesting findings regarding the effects of the bit on the horse's mouth and also on the whole of the horse. What Dr. Cook has found is that a bit is actually detrimental, in various ways, from subtle to profound. His discoveries have led to the use of a new design of bitless bridle, which has been developed according to his specifications, to act upon the whole of the head, without causing the horse either pain or physiological confusion. -
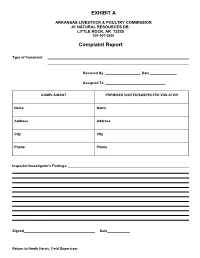
Complaint Report
EXHIBIT A ARKANSAS LIVESTOCK & POULTRY COMMISSION #1 NATURAL RESOURCES DR. LITTLE ROCK, AR 72205 501-907-2400 Complaint Report Type of Complaint Received By Date Assigned To COMPLAINANT PREMISES VISITED/SUSPECTED VIOLATOR Name Name Address Address City City Phone Phone Inspector/Investigator's Findings: Signed Date Return to Heath Harris, Field Supervisor DP-7/DP-46 SPECIAL MATERIALS & MARKETPLACE SAMPLE REPORT ARKANSAS STATE PLANT BOARD Pesticide Division #1 Natural Resources Drive Little Rock, Arkansas 72205 Insp. # Case # Lab # DATE: Sampled: Received: Reported: Sampled At Address GPS Coordinates: N W This block to be used for Marketplace Samples only Manufacturer Address City/State/Zip Brand Name: EPA Reg. #: EPA Est. #: Lot #: Container Type: # on Hand Wt./Size #Sampled Circle appropriate description: [Non-Slurry Liquid] [Slurry Liquid] [Dust] [Granular] [Other] Other Sample Soil Vegetation (describe) Description: (Place check in Water Clothing (describe) appropriate square) Use Dilution Other (describe) Formulation Dilution Rate as mixed Analysis Requested: (Use common pesticide name) Guarantee in Tank (if use dilution) Chain of Custody Date Received by (Received for Lab) Inspector Name Inspector (Print) Signature Check box if Dealer desires copy of completed analysis 9 ARKANSAS LIVESTOCK AND POULTRY COMMISSION #1 Natural Resources Drive Little Rock, Arkansas 72205 (501) 225-1598 REPORT ON FLEA MARKETS OR SALES CHECKED Poultry to be tested for pullorum typhoid are: exotic chickens, upland birds (chickens, pheasants, pea fowl, and backyard chickens). Must be identified with a leg band, wing band, or tattoo. Exemptions are those from a certified free NPIP flock or 90-day certificate test for pullorum typhoid. Water fowl need not test for pullorum typhoid unless they originate from out of state. -

Arabic-New Microsoft Word Document
294 KUSTANAI (Kustanaiskaya) The Kustanai was developed in the steppes of western Kazakhstan at the collective-farm and state-farm studs. The breeding nucleus is concentrated at Kustanai and Maikulski studs. Its development dates from 1887 to 1951. The first date is the year of establishment of the state-owned stud, the Turgai; it was followed by the Kustanai in 1888 and the Orenburg in 1890. The last is the date of official recognition of the Kustanai breed. The new breed was developed by crossing native Kazakh steppe horses with Don, Strelets, Astrakhan (improved Kalmyk) and halfbred Thoroughbred stallions. Nevertheless, at the onset the crossbreeding was unsuccessful. Only after the nucleus of local brood mares, improved by pure breeding and regular creep-feeding, was formed at Kustanai stud did crossbreeding with Thoroughbreds yield a positive result. In the 1920s they began to develop a new breed at Kustanai stud. The work was continued in the 1930s with two systems of management. The first involved keeping in stables and on pastures, winter grazing in good weather, abundant hay and concentrate 295 feeding, hand mating and weaning of the foals at 6-8 months. The other involved improved taboon keeping, year-round grazing and keeping in sheds in bad weather, free mating, hay and concentrate creep-feeding. The first method was employed at Kustanai and Troitski studs and the second at the Maikulski and other studs. The breeding work was directed at developing simultaneously two types - saddle and steppe. The saddle type included horses with a high proportion of Thoroughbred blood, while the steppe type consisted of Thoroughbred- Don-Kazakh and other crossbreds bred inter se. -

Trigeminal-Mediated Headshaking in Horses: Prevalence, Impact, and Management Strategies
Roberts, V. (2019). Trigeminal-mediated headshaking in horses: prevalence, impact, and management strategies. Veterinary Medicine: Research and Reports, 10. https://doi.org/10.2147/VMRR.S163805 Publisher's PDF, also known as Version of record License (if available): CC BY Link to published version (if available): 10.2147/VMRR.S163805 Link to publication record in Explore Bristol Research PDF-document This is the final published version of the article (version of record). It first appeared online via Dovepress at https://www.dovepress.com/veterinary-medicine-research-and-reports-journal. Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/red/research-policy/pure/user-guides/ebr-terms/ Journal name: Veterinary Medicine: Research and Reports Article Designation: Review Year: 2019 Volume: 10 Veterinary Medicine: Research and Reports Dovepress Running head verso: Roberts Running head recto: Trigeminal-mediated headshaking in horses open access to scientific and medical research DOI: http://dx.doi.org/10.2147/VMRR.S163805 Open Access Full Text Article REVIEW Trigeminal-mediated headshaking in horses: prevalence, impact, and management strategies Veronica Roberts Abstract: Trigeminal-mediated headshaking is a little-understood neuropathic facial pain con- dition of the horse. The condition may affect around 1% of the equine population to a degree of Bristol Vet School, Faculty of Health Sciences, University of Bristol, severity sufficient to require veterinary attention. As a pain condition, this represents a significant Langford, North Somerset BS40 5HB, welfare issue. -

Frequently Asked Questions
Page 1 of 7 Email: [email protected] Website: www.bitlessbridle.com THE BITLESS BRIDLE FREQUENTLY ASKED QUESTIONS The following pages provide brief answers to the most frequently asked questions but for more details please visit our website at www.bitlessbridle.com What is special about The Bitless Bridle and how does it work? It works on an entirely new concept compared with other bridles, including all other bitless bridles; i.e., the Hackamores, bosals and sidepulls. The current bitless bridles work primarily by potentially painful pressure on the nose, bringing about poll flexion. A bit also controls primarily by poll flexion but brings this about through potentially painful pressure on the mouth. In contrast, The Bitless Bridle is special because of the way it works. It provides control by applying gentle and painless pressure, distributed to the whole of the head. In other words, there is pressure across the poll, behind the ears, down the side of the face, behind the chin and across the nose. It does not depend for its control primarily on poll flexion. Whereas the bit exerts focal pressure on the mouth, The Bitless Bridle distributes its pressure over a wide area (one or both sides of the head, depending on whether you are steering or stopping) and over less sensitive tissues (skin and mainly underlying muscle). It does this through two loops, one over the poll and one over the nose. Essentially, it gives the rider an inoffensive and benevolent headlock, as compared with the bit's potentially offensive and painful control of the mouth. -

Information Resources on the Care and Welfare of Horses
NATIONAL AGRICULTURAL LIBRARY ARCHIVED FILE Archived files are provided for reference purposes only. This file was current when produced, but is no longer maintained and may now be outdated. Content may not appear in full or in its original format. All links external to the document have been deactivated. For additional information, see http://pubs.nal.usda.gov. United States Information Resources on the Care and Department of Agriculture Welfare of Horses AWIC Resource Series No. 36 Agricultural Research November 2006 Service Updates Housing, Husbandry, and Welfare of Horses, 1994 National Agricultural Library Animal Welfare Information Center Compiled and edited by: Cristin Swords Animal Welfare Information Center National Agricultural Library U.S. Department of Agriculture Published by: U. S. Department of Agriculture Agricultural Research Service National Agricultural Library Animal Welfare Information Center Beltsville, Maryland 20705 Web site: http://awic.nal.usda.gov Published in cooperation with the Virginia-Maryland Regional College of Veterinary Medicine Web Policies and Important Links Contents Forward About this Document Request Library Materials Horse Welfare by D. Mills, University of Lincoln Equine Welfare Issues in the United States: An Introduction by C.L. Stull, University of California, Davis Bibliography Anesthesia and Analgesia Behavior Environmental Enrichment Housing Law and Legislation Nutrition and Feeding Feeding Methods Feeding Restrictions Age Specific Nutrition Concentrates Roughages Vitamins and Supplements Pasture PMU Ranching Safety Training Transportation Web Resources Forward This information resource came to fruition through the diligence of a student employee at the Animal Welfare Information Center. The document contains a comprehensive bibliography and extensive selection of web site resources. Two papers introducing horse care and welfare issues are also included. -

This Is a Cross-Reference List for Entering Your Horses at NAN. It Will
This is a cross-reference list for entering your horses at NAN. It will tell you how a breed is classified for NAN so that you can easily find the correct division in which to show your horse. If your breed is designated "other pure," with no division indicated, the NAN committee will use body type and suitability to determine in what division it belongs. Note: For the purposes of NAN, NAMHSA considers breeds that routinely fall at 14.2 hands high or less to be ponies. Stock Breeds American White Horse/Creme Horse (United States) American Mustang (not Spanish) Appaloosa (United States) Appendix Quarter Horse (United States) Australian Stock Horse (Australia) Australian Brumby (Australia) Bashkir Curly (United States, Other) Paint (United States) Quarter Horse (United States) Light Breeds Abyssinian (Ethiopia) Andravida (Greece) Arabian (Arabian Peninsula) Barb (not Spanish) Bulichi (Pakistan) Calabrese (Italy) Canadian Horse (Canada) Djerma (Niger/West Africa) Dongola (West Africa) Hirzai (Pakistan) Iomud (Turkmenistan) Karabair (Uzbekistan) Kathiawari (India) Maremmano (Italy) Marwari (India) Morgan (United States) Moroccan Barb (North Africa) Murghese (Italy) Persian Arabian (Iran) Qatgani (Afghanistan) San Fratello (Italy) Turkoman (Turkmenistan) Unmol (Punjab States/India) Ventasso (Italy) Gaited Breeds Aegidienberger (Germany) American Saddlebred (United States) Boer (aka Boerperd) (South Africa) Deliboz (Azerbaijan) Kentucky Saddle Horse (United States) McCurdy Plantation Horse (United States) Missouri Fox Trotter (United States) -

Horse Breeds - Volume 2
Horse breeds - Volume 2 A Wikipedia Compilation by Michael A. Linton Contents Articles Danish Warmblood 1 Danube Delta horse 3 Dølehest 4 Dutch harness horse 7 Dutch Heavy Draft 10 Dutch Warmblood 12 East Bulgarian 15 Estonian Draft 16 Estonian horse 17 Falabella 19 Finnhorse 22 Fjord horse 42 Florida Cracker Horse 47 Fouta 50 Frederiksborg horse 51 Freiberger 53 French Trotter 55 Friesian cross 57 Friesian horse 59 Friesian Sporthorse 64 Furioso-North Star 66 Galiceno 68 Galician Pony 70 Gelderland horse 71 Georgian Grande Horse 74 Giara horse 76 Gidran 78 Groningen horse 79 Gypsy horse 82 Hackney Horse 94 Haflinger 97 Hanoverian horse 106 Heck horse 113 Heihe horse 115 Henson horse 116 Hirzai 117 Hispano-Bretón 118 Hispano-Árabe 119 Holsteiner horse 120 Hungarian Warmblood 129 Icelandic horse 130 Indian Half-Bred 136 Iomud 137 Irish Draught 138 Irish Sport Horse 141 Italian Heavy Draft 143 Italian Trotter 145 Jaca Navarra 146 Jutland horse 147 Kabarda horse 150 Kaimanawa horse 153 Karabair 156 Karabakh horse 158 Kathiawari 161 Kazakh horse 163 Kentucky Mountain Saddle Horse 165 Kiger Mustang 168 Kinsky horse 171 Kisber Felver 173 Kladruber 175 Knabstrupper 178 Konik 180 Kustanair 183 References Article Sources and Contributors 185 Image Sources, Licenses and Contributors 188 Article Licenses License 192 Danish Warmblood 1 Danish Warmblood Danish Warmblood Danish warmblood Alternative names Dansk Varmblod Country of origin Denmark Horse (Equus ferus caballus) The Danish Warmblood (Dansk Varmblod) is the modern sport horse breed of Denmark. Initially established in the mid-20th century, the breed was developed by crossing native Danish mares with elite stallions from established European bloodlines.