Autoregulatory CD8 T Cells Depend on Cognate Antigen Recognition and CD4/CD8 Myelin Determinants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Intrinsically Disordered Proteins of Myelin in Health and Disease
cells Review Flexible Players within the Sheaths: The Intrinsically Disordered Proteins of Myelin in Health and Disease Arne Raasakka 1 and Petri Kursula 1,2,* 1 Department of Biomedicine, University of Bergen, Jonas Lies vei 91, NO-5009 Bergen, Norway; [email protected] 2 Faculty of Biochemistry and Molecular Medicine & Biocenter Oulu, University of Oulu, Aapistie 7A, FI-90220 Oulu, Finland * Correspondence: [email protected] Received: 30 January 2020; Accepted: 16 February 2020; Published: 18 February 2020 Abstract: Myelin ensheathes selected axonal segments within the nervous system, resulting primarily in nerve impulse acceleration, as well as mechanical and trophic support for neurons. In the central and peripheral nervous systems, various proteins that contribute to the formation and stability of myelin are present, which also harbor pathophysiological roles in myelin disease. Many myelin proteins have common attributes, including small size, hydrophobic segments, multifunctionality, longevity, and regions of intrinsic disorder. With recent advances in protein biophysical characterization and bioinformatics, it has become evident that intrinsically disordered proteins (IDPs) are abundant in myelin, and their flexible nature enables multifunctionality. Here, we review known myelin IDPs, their conservation, molecular characteristics and functions, and their disease relevance, along with open questions and speculations. We place emphasis on classifying the molecular details of IDPs in myelin, and we correlate these with their various functions, including susceptibility to post-translational modifications, function in protein–protein and protein–membrane interactions, as well as their role as extended entropic chains. We discuss how myelin pathology can relate to IDPs and which molecular factors are potentially involved. Keywords: myelin; intrinsically disordered protein; multiple sclerosis; peripheral neuropathies; myelination; protein folding; protein–membrane interaction; protein–protein interaction 1. -

How Does Protein Zero Assemble Compact Myelin?
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 13 May 2020 doi:10.20944/preprints202005.0222.v1 Peer-reviewed version available at Cells 2020, 9, 1832; doi:10.3390/cells9081832 Perspective How Does Protein Zero Assemble Compact Myelin? Arne Raasakka 1,* and Petri Kursula 1,2 1 Department of Biomedicine, University of Bergen, Jonas Lies vei 91, NO-5009 Bergen, Norway 2 Faculty of Biochemistry and Molecular Medicine & Biocenter Oulu, University of Oulu, Aapistie 7A, FI-90220 Oulu, Finland; [email protected] * Correspondence: [email protected] Abstract: Myelin protein zero (P0), a type I transmembrane protein, is the most abundant protein in peripheral nervous system (PNS) myelin – the lipid-rich, periodic structure that concentrically encloses long axonal segments. Schwann cells, the myelinating glia of the PNS, express P0 throughout their development until the formation of mature myelin. In the intramyelinic compartment, the immunoglobulin-like domain of P0 bridges apposing membranes together via homophilic adhesion, forming a dense, macroscopic ultrastructure known as the intraperiod line. The C-terminal tail of P0 adheres apposing membranes together in the narrow cytoplasmic compartment of compact myelin, much like myelin basic protein (MBP). In mouse models, the absence of P0, unlike that of MBP or P2, severely disturbs the formation of myelin. Therefore, P0 is the executive molecule of PNS myelin maturation. How and when is P0 trafficked and modified to enable myelin compaction, and how disease mutations that give rise to incurable peripheral neuropathies alter the function of P0, are currently open questions. The potential mechanisms of P0 function in myelination are discussed, providing a foundation for the understanding of mature myelin development and how it derails in peripheral neuropathies. -

Pathological Relationships Involving Iron and Myelin May Constitute a Shared Mechanism Linking Various Rare and Common Brain Diseases
Rare Diseases ISSN: (Print) 2167-5511 (Online) Journal homepage: http://www.tandfonline.com/loi/krad20 Pathological relationships involving iron and myelin may constitute a shared mechanism linking various rare and common brain diseases Moones Heidari, Sam H. Gerami, Brianna Bassett, Ross M. Graham, Anita C.G. Chua, Ritambhara Aryal, Michael J. House, Joanna F. Collingwood, Conceição Bettencourt, Henry Houlden, Mina Ryten , John K. Olynyk, Debbie Trinder, Daniel M. Johnstone & Elizabeth A. Milward To cite this article: Moones Heidari, Sam H. Gerami, Brianna Bassett, Ross M. Graham, Anita C.G. Chua, Ritambhara Aryal, Michael J. House, Joanna F. Collingwood, Conceição Bettencourt, Henry Houlden, Mina Ryten , John K. Olynyk, Debbie Trinder, Daniel M. Johnstone & Elizabeth A. Milward (2016) Pathological relationships involving iron and myelin may constitute a shared mechanism linking various rare and common brain diseases, Rare Diseases, 4:1, e1198458, DOI: 10.1080/21675511.2016.1198458 To link to this article: http://dx.doi.org/10.1080/21675511.2016.1198458 © 2016 The Author(s). Published with View supplementary material license by Taylor & Francis Group, LLC© Moones Heidari, Sam H. Gerami, Brianna Bassett, Ross M. Graham, Anita C.G. Chua, Ritambhara Aryal, Michael J. House, Joanna Accepted author version posted online: 22 Submit your article to this journal JunF. Collingwood, 2016. Conceição Bettencourt, PublishedHenry Houlden, online: Mina 22 Jun Ryten, 2016. for the UK Brain Expression Consortium (UKBEC), John K. Olynyk, Debbie Trinder, Daniel M. Johnstone,Article views: and 541 Elizabeth A. Milward. View related articles View Crossmark data Citing articles: 2 View citing articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=krad20 Download by: [University of Newcastle, Australia] Date: 17 May 2017, At: 19:57 RARE DISEASES 2016, VOL. -

Myelination Is Delayed During Postnatal Brain Development in the Mdx Mouse Model of Duchenne Muscular Dystrophy Azeez Aranmolate, Nathaniel Tse and Holly Colognato*
Aranmolate et al. BMC Neurosci (2017) 18:63 DOI 10.1186/s12868-017-0381-0 BMC Neuroscience RESEARCH ARTICLE Open Access Myelination is delayed during postnatal brain development in the mdx mouse model of Duchenne muscular dystrophy Azeez Aranmolate, Nathaniel Tse and Holly Colognato* Abstract Background: In Duchenne muscular dystrophy (DMD), the loss of the dystrophin component of the dystrophin- glycoprotein complex (DGC) compromises plasma membrane integrity in skeletal muscle, resulting in extensive muscle degeneration. In addition, many DMD patients exhibit brain defcits in which the cellular etiology remains poorly understood. We recently found that dystroglycan, a receptor component of the DGC that binds intracellularly to dystrophin, regulates the development of oligodendrocytes, the myelinating glial cells of the brain. Results: We investigated whether dystrophin contributes to oligodendroglial function and brain myelination. We found that oligodendrocytes express up to three dystrophin isoforms, in conjunction with classic DGC components, which are developmentally regulated during diferentiation and in response to extracellular matrix engagement. We found that mdx mice, a model of DMD lacking expression of the largest dystrophin isoform, have delayed myelination and inappropriate oligodendrocyte progenitor proliferation in the cerebral cortex. When we prevented the expression of all oligodendroglial dystrophin isoforms in cultured oligodendrocytes using RNA interference, we found that later stages of oligodendrocyte maturation -

Can the Fact That Myelin Proteins Are Old and Break Down Explain the Origin of Multiple Sclerosis in Some People?
Journal of Clinical Medicine Review Can the Fact That Myelin Proteins Are Old and Break down Explain the Origin of Multiple Sclerosis in Some People? Roger J. W. Truscott * and Michael G. Friedrich Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW 2522, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-2-4298-3503; Fax: +61-2-4221-8130 Received: 11 July 2018; Accepted: 12 September 2018; Published: 14 September 2018 Abstract: Recent discoveries may change the way that multiple sclerosis (MS) is viewed, particularly with regard to the reasons for the untoward immune response. The fact that myelin proteins are long-lived, and that by the time we are adults, they are extensively degraded, alters our perspective on the reasons for the onset of autoimmunity and the origin of MS. For example, myelin basic protein (MBP) from every human brain past the age of 20 years, is so greatly modified, that it is effectively a different protein from the one that was laid down in childhood. Since only a subset of people with such degraded MBP develop MS, a focus on understanding the mechanism of immune responses to central nervous system (CNS) antigens and cerebral immune tolerance appear to be worthwhile avenues to explore. In accord with this, it will be productive to examine why all people, whose brains contain large quantities of a “foreign antigen”, do not develop MS. Importantly for the potential causation of MS, MBP from MS patients breaks down differently from the MBP in aged controls. If the novel structures formed in these MS-specific regions are particularly antigenic, it could help explain the origin of MS. -

LRP1 Regulates Peroxisome Biogenesis and Cholesterol
RESEARCH ARTICLE LRP1 regulates peroxisome biogenesis and cholesterol homeostasis in oligodendrocytes and is required for proper CNS myelin development and repair Jing-Ping Lin1, Yevgeniya A Mironova2, Peter Shrager3, Roman J Giger1,2,4,5* 1Department of Cell and Developmental Biology, University of Michigan School of Medicine, Ann Arbor, MI, United States; 2Cellular and Molecular Biology Graduate Program, University of Michigan Medical School, Ann Arbor, MI, United States; 3Department of Neuroscience, University of Rochester Medical Center, Rochester, NY, United States ; 4Department of Neurology, University of Michigan Medical School, Ann Arbor, MI, United States; 5Interdepartmental Neuroscience Graduate Program, University of Michigan Medical School, Ann Arbor, MI, United States Abstract Low-density lipoprotein receptor-related protein-1 (LRP1) is a large endocytic and signaling molecule broadly expressed by neurons and glia. In adult mice, global inducible (Lrp1flox/ flox;CAG-CreER) or oligodendrocyte (OL)-lineage specific ablation (Lrp1flox/flox;Pdgfra-CreER) of Lrp1 attenuates repair of damaged white matter. In oligodendrocyte progenitor cells (OPCs), Lrp1 is required for cholesterol homeostasis and differentiation into mature OLs. Lrp1-deficient OPC/ OLs show a strong increase in the sterol-regulatory element-binding protein-2 yet are unable to maintain normal cholesterol levels, suggesting more global metabolic deficits. Mechanistic studies revealed a decrease in peroxisomal biogenesis factor-2 and fewer peroxisomes in OL processes. / *For correspondence: Treatment of Lrp1À À OPCs with cholesterol or activation of peroxisome proliferator-activated [email protected] receptor-g with pioglitazone alone is not sufficient to promote differentiation; however, when combined, cholesterol and pioglitazone enhance OPC differentiation into mature OLs. Collectively, Competing interests: The our studies reveal a novel role for Lrp1 in peroxisome biogenesis, lipid homeostasis, and OPC authors declare that no competing interests exist. -

Impaired Expression of Tetraspanin 32 (TSPAN32) in Memory T Cells of Patients with Multiple Sclerosis
brain sciences Article Impaired Expression of Tetraspanin 32 (TSPAN32) in Memory T Cells of Patients with Multiple Sclerosis Maria Sofia Basile 1, Emanuela Mazzon 2 , Katia Mangano 1 , Manuela Pennisi 1, Maria Cristina Petralia 2, Salvo Danilo Lombardo 1 , Ferdinando Nicoletti 1 , Paolo Fagone 1,* and Eugenio Cavalli 2 1 Department of Biomedical and Biotechnological Sciences, University of Catania, Via S. Sofia 89, 95123 Catania, Italy; sofi[email protected] (M.S.B.); [email protected] (K.M.); [email protected] (M.P.); [email protected] (S.D.L.); [email protected] (F.N.) 2 IRCCS Centro Neurolesi “Bonino-Pulejo”, Via Provinciale Palermo, Contrada Casazza, 98124 Messina, Italy; [email protected] (E.M.); [email protected] (M.C.P.); [email protected] (E.C.) * Correspondence: [email protected] Received: 29 November 2019; Accepted: 14 January 2020; Published: 17 January 2020 Abstract: Tetraspanins are a conserved family of proteins involved in a number of biological processes. We have previously shown that Tetraspanin-32 (TSPAN32) is significantly downregulated upon activation of T helper cells via anti-CD3/CD28 stimulation. On the other hand, TSPAN32 is marginally modulated in activated Treg cells. A role for TSPAN32 in controlling the development of autoimmune responses is consistent with our observation that encephalitogenic T cells from myelin oligodendrocyte glycoprotein (MOG)-induced experimental autoimmune encephalomyelitis (EAE) mice exhibit significantly lower levels of TSPAN32 as compared to naïve T cells. In the present study, by making use of ex vivo and in silico analysis, we aimed to better characterize the pathophysiological and diagnostic/prognostic role of TSPAN32 in T cell immunity and in multiple sclerosis (MS). -

Identification of Three Forms of Human Myelin Basic Protein by Cdna Cloning
Proc. Nail. Acad. Sci. USA Vol. 83, pp. 4962-4966, July 1986 Neurobiology Identification of three forms of human myelin basic protein by cDNA cloning (myelin proteins/oligodendroglia/alternative splicing) JOHN KAMHOLZ*, FRANCESCA DE FERRAt, CARMIE PUCKETT*, AND ROBERT LAZZARINI* *Laboratory of Molecular Genetics, National Institute of Neurological and Communicative Disorders and Stroke, National Institutes of Health, 9000 Rockville Pike, Bethesda, MD 20892; and tThe Wistar Institute, 36th Street and Spruce, Philadelphia, PA 19104 Communicated by Roscoe 0. Brady, March 10, 1986 ABSTRACT We have isolated cDNA clones encoding three Unlike the case in the mouse, only a single MBP species separate forms of human myelin basic protein (MBP), 21.5, has been identified in human myelin. The human 18.5-kDa 18.5, and 17.2 kDa, and have determined the nucleotide MBP has been well characterized, and its amino acid se- sequence of each. The three forms share a common sequence quence has been determined directly (6). Although minor but differ by the inclusion of a 26-residue amino acid sequence bands, both larger (7) and smaller (8), are sometimes seen on near the N terminus of the 21.5-kDa protein or by the absence protein gels of human MBP, these forms have not been ofan 11-residue amino acid sequence near the C terminus ofthe isolated or characterized. 17.2-kDa protein. The sequences either added to or deleted We have examined the question ofmultiple forms ofhuman from the major 18.5-kDa MBP correspond exactly to exons 2 MBP by assembling a large collection of human MBP cDNA and 5 of the mouse MBP gene, suggesting that the human and clones and examining their structure by restriction endonu- mouse genes have similar exon structures. -

Obinutuzumab-Induced B Cell Depletion Reduces Spinal Cord Pathology in a CD20 Double Transgenic Mouse Model of Multiple Sclerosis
International Journal of Molecular Sciences Article Obinutuzumab-Induced B Cell Depletion Reduces Spinal Cord Pathology in a CD20 Double Transgenic Mouse Model of Multiple Sclerosis Thomas Breakell 1, Sabine Tacke 1, Verena Schropp 1, Henrik Zetterberg 2,3,4,5, Kaj Blennow 2,3, Eduard Urich 6 and Stefanie Kuerten 1,* 1 Institute of Anatomy and Cell Biology, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), 91054 Erlangen, Germany; [email protected] (T.B.); [email protected] (S.T.); [email protected] (V.S.) 2 Department of Psychiatry and Neurochemistry, Institute of Neuroscience & Physiology, the Sahlgrenska Academy at the University of Gothenburg, 43141 Mölndal, Sweden; [email protected] (H.Z.); [email protected] (K.B.) 3 Clinical Neurochemistry Laboratory, Sahlgrenska University Hospital, 43180 Mölndal, Sweden 4 Department of Neurodegenerative Disease, UCL Institute of Neurology, Queen Square, London WC1N 3BG, UK 5 UK Dementia Research Institute at UCL, London WC1E 6BT, UK 6 Roche Pharma Research and Early Development, Neuroscience, Roche Innovation Center, 4070 Basel, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +49-9131-8522264 Received: 26 August 2020; Accepted: 16 September 2020; Published: 18 September 2020 Abstract: B cell-depleting therapies have recently proven to be clinically highly successful in the treatment of multiple sclerosis (MS). This study aimed to determine the effects of the novel type II anti-human CD20 (huCD20) monoclonal antibody (mAb) obinutuzumab (OBZ) on spinal cord degeneration in a B cell-dependent mouse model of MS. Double transgenic huCD20xHIGR3 (CD20dbtg) mice, which express human CD20, were immunised with the myelin fusion protein MP4 to induce experimental autoimmune encephalomyelitis (EAE). -
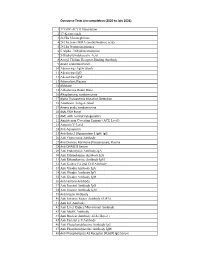
Outsource Tests List Compilation (2020 to July 2021) 1 17 OHP
Outsource Tests List compilation (2020 to July 2021) 1 17 OHP-ACTH Stimulation 2 17-Ketosteroids 3 24 Hrs Metanephrines 4 24 Hrs urine MMA (methylmalonic acid) 5 24 Hrs Normetanephrines 6 5 Alpha - Dihydrotestosterone 7 5-Hydroxyindoleacetic Acid 8 Acetyl Choline Receptor Binding Antibody 9 Acute Leukemia Panel 10 Adenovirus Ag(In Stool) 11 Adenovirus IgG 12 Adenovirus IgM 13 Adrenaline, Plasma 14 Aldolase 15 Aldosterone Renin Ratio 16 Alkaptonuria, random urine 17 Alpha Thalassemia Mutation Detection 18 Amebiasis Antigen ,Stool 19 Amino acids, random urine 20 AML FISH Panel 21 AML with normal cytogenetics 22 Angiotensin Coverting Enzyme (ACE Level) 23 Annexin V Level 24 Anti Aquaporin 25 Anti Beta 2 Glycoprotein 1 IgM. IgG 26 Anti Centromere Antibody 27 Anti Diuretic Hormone (Vasopressin), Plasma 28 Anti DNASE B Serum 29 Anti Endomysial Antibody-IgA 30 Anti Ethanolamine Antibody IgG 31 Anti Ethanolamine Antibody IgM 32 Anti Gastric Parietal Cell Antibody 33 Anti Gliadin Antibody IgA 34 Anti Gliadin Antibody IgG 35 Anti Gliadin Antibody IgM 36 Anti Histone Antibody 37 Anti Inositol Antibody IgG 38 Anti Inositol Antibody IgM 39 Anti Insulin Antibody 40 Anti Intrinsic Factor Antibody (AIFA) 41 Anti Jo1 Antibody 42 Anti Liver Kidney Microsomal Antibody 43 Anti MuSK Antibody 44 Anti Nuclear Antibody -IFA (Hep-2 ) 45 Anti Parietal cell Antibody 46 Anti Phosphatidylserine Antibody IgG 47 Anti Phosphatidylserine Antibody IgM 48 Anti Phospholipase A2 Receptor (PLA2R) IgG Serum 49 Anti phosphatidylcholine Antibody IgG 50 Anti phosphatidylcholine -

Neurofibromatosis Type 2 Tumor Suppressor Protein Is Expressed in Oligodendrocytes and Regulates Cell Proliferation and Process Formation
RESEARCH ARTICLE Neurofibromatosis type 2 tumor suppressor protein is expressed in oligodendrocytes and regulates cell proliferation and process formation Andrea Toledo1,2☯, Elena Grieger1☯, Khalad Karram3, Helen Morrison4, Stephan L. Baader1* a1111111111 1 Institute of Anatomy, Anatomy and Cell Biology, Bonn, Germany, 2 Laboratorio de Cultivo de Tejidos, SeccioÂn BiologõÂa Celular, Facultad de Ciencias, UdelaR, Montevideo, Uruguay, 3 Institute for Molecular a1111111111 Medicine, Johannes Gutenberg University Mainz, Mainz, Germany, 4 Leibniz Institute for Age Research, a1111111111 Fritz Lipmann Institute, Jena, Germany a1111111111 a1111111111 ☯ These authors contributed equally to this work. * [email protected] Abstract OPEN ACCESS Citation: Toledo A, Grieger E, Karram K, Morrison The neurofibromatosis type 2 (NF2) tumor suppressor protein Merlin functions as a negative H, Baader SL (2018) Neurofibromatosis type 2 regulator of cell growth and actin dynamics in different cell types amongst which Schwann tumor suppressor protein is expressed in cells have been extensively studied. In contrast, the presence and the role of Merlin in oligo- oligodendrocytes and regulates cell proliferation dendrocytes, the myelin forming cells within the CNS, have not been elucidated. In this and process formation. PLoS ONE 13(5): e0196726. https://doi.org/10.1371/journal. work, we demonstrate that Merlin immunoreactivity was broadly distributed in the white mat- pone.0196726 ter throughout the central nervous system. Following Merlin expression during development Editor: Fernando de Castro, Instituto Cajal-CSIC, in the cerebellum, Merlin could be detected in the cerebellar white matter tract at early post- SPAIN natal stages as shown by its co-localization with Olig2-positive cells as well as in adult brain Received: June 2, 2017 sections where it was aligned with myelin basic protein containing fibers. -

Oligodendrocytes Secrete Exosomes Containing Major Myelin and Stress-Protective Proteins: Trophic Support for Axons?
1446 DOI 10.1002/prca.200700522 Proteomics Clin. Appl. 2007, 1, 1446–1461 RESEARCH ARTICLE Oligodendrocytes secrete exosomes containing major myelin and stress-protective proteins: Trophic support for axons? Eva-Maria Krämer-Albers1, Niko Bretz1*, Stefan Tenzer2*, Christine Winterstein1*, Wiebke Möbius3, Hendrik Berger2, Klaus-Armin Nave3, Hansjörg Schild2 and Jacqueline Trotter1 1 Department of Biology, Unit of Molecular Cell Biology, University of Mainz, Germany 2 Institute for Immunology, University of Mainz, Germany 3 Department of Neurogenetics, Max Planck Institute of Experimental Medicine, Goettingen, Germany Oligodendrocytes synthesize the CNS myelin sheath by enwrapping axonal segments with Received: June 1, 2007 elongations of their plasma membrane. Spatial and temporal control of membrane traffic is a Revised: July 14, 2007 prerequisite for proper myelin formation. The major myelin proteolipid protein (PLP) accumu- Accepted: August 1, 2007 lates in late endosomal storage compartments and multivesicular bodies (MVBs). Fusion of MVBs with the plasma membrane results in the release of the intralumenal vesicles, termed exosomes, into the extracellular space. Here, we show that cultured oligodendrocytes secrete exosomes carrying major amounts of PLP and 2030-cyclic-nucleotide-phosphodiesterase (CNP). These exosomes migrated at the characteristic density of 1.1021.14 g/mL in sucrose density gradients. Treatment of primary oligodendrocytes with the calcium-ionophore ionomycin mark- edly increased the release of PLP-containing exosomes, indicating that oligodendroglial exosome secretion is regulated by cytosolic calcium levels. A proteomic analysis of the exosomal fraction isolated by sucrose density centrifugation revealed in addition to PLP and CNP, myelin basic protein (MBP) and myelin oligodendrocyte glycoprotein (MOG) as constituents of oligoden- droglial exosomes, together with a striking group of proteins with proposed functions in the relief of cell stress.