Clinic Review of Pd Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Download Network
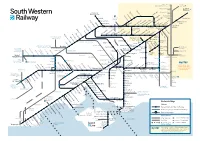
Milton Keynes, London Birmingham and the North Victoria Watford Junction London Brentford Waterloo Syon Lane Windsor & Shepherd’s Bush Eton Riverside Isleworth Hounslow Kew Bridge Kensington (Olympia) Datchet Heathrow Chiswick Vauxhall Airport Virginia Water Sunnymeads Egham Barnes Bridge Queenstown Wraysbury Road Longcross Sunningdale Whitton TwickenhamSt. MargaretsRichmondNorth Sheen BarnesPutneyWandsworthTown Clapham Junction Staines Ashford Feltham Mortlake Wimbledon Martins Heron Strawberry Earlsfield Ascot Hill Croydon Tramlink Raynes Park Bracknell Winnersh Triangle Wokingham SheppertonUpper HallifordSunbury Kempton HamptonPark Fulwell Teddington Hampton KingstonWick Norbiton New Oxford, Birmingham Winnersh and the North Hampton Court Malden Thames Ditton Berrylands Chertsey Surbiton Malden Motspur Reading to Gatwick Airport Chessington Earley Bagshot Esher TolworthManor Park Hersham Crowthorne Addlestone Walton-on- Bath, Bristol, South Wales Reading Thames North and the West Country Camberley Hinchley Worcester Beckenham Oldfield Park Wood Park Junction South Wales, Keynsham Trowbridge Byfleet & Bradford- Westbury Brookwood Birmingham Bath Spaon-Avon Newbury Sandhurst New Haw Weybridge Stoneleigh and the North Reading West Frimley Elmers End Claygate Farnborough Chessington Ewell West Byfleet South New Bristol Mortimer Blackwater West Woking West East Addington Temple Meads Bramley (Main) Oxshott Croydon Croydon Frome Epsom Taunton, Farnborough North Exeter and the Warminster Worplesdon West Country Bristol Airport Bruton Templecombe -

Solent Connectivity May 2020
Solent Connectivity May 2020 Continuous Modular Strategic Planning Page | 1 Page | 2 Table of Contents 1.0 Executive Summary .......................................................................................................................................... 6 2.0 The Solent CMSP Study ................................................................................................................................... 10 2.1 Scope and Geography....................................................................................................................... 10 2.2 Fit with wider rail industry strategy ................................................................................................. 11 2.3 Governance and process .................................................................................................................. 12 3.0 Context and Strategic Questions ............................................................................................................ 15 3.1 Strategic Questions .......................................................................................................................... 15 3.2 Economic context ............................................................................................................................. 16 3.3 Travel patterns and changes over time ............................................................................................ 18 3.4 Dual-city region aspirations and city to city connectivity ................................................................ -

Widley Widley
Widley Widley 1.0 PARISH Southwick & Widley (formerley Widley, then Cosham) 2.0 HUNDRED Portsdown 3.0 NGR 465900 107400 4.0 GEOLOGY London Clay; Alluvium to north, Reading Beds to south. 5.0 SITE CONTEXT (Map 2) 5.1 Widley, as a settlement, is almost impossible to identify. There is no longer a parish church and there are no principal buildings with the exception of the C18 Fort Widley, which is adjacent to the northern margin of the B2177. The fort is situated on the east / west ridge of Portsdown (100m AOD) and from this lofty perch it looks down upon Portsmouth to the south. North of Fort Widley the land drops gradually away to the heartland of the former Widley parish. This is a landscape of scattered farmsteads with irregular plantations of mixed woodland beyond, perhaps indicative that this was once a part of the medieval Forest of Bere. 5.2 The recent history of the parish of Widley has been chequered. In 1894, it was amalgamated with Wymering and Cosham to form the parish of Cosham (VCH 3: 171). Subsequently, the greater part Widley parish has been joined with Southwick to become the parish of Southwick and Widley in Winchester City District. 6.0 PLAN TYPE & DESCRIPTION (Maps 3, 4, & 5) Church and farm 6.1.1 Map 1 shows Widley as an odd-shaped parish unit squeezed between Wymering (west) and Cosham (east). The greater part of the C19 parish stretched northwards from the ridge of Portsdown whilst a relatively narrow strip of land gave access to the sea and the littoral marshes. -

Specifications Or Materials
Affinity Suttonat DRAYTON PARK HELPING PEOPLE Two and three bedroom houses PUT D OWN ROOTS and apa rtments for sale on a shared ownership basis SPECIFICA TION I Quality fitted kitchen I Stainless steel oven, hob and hood I Fridge freezer I Washer/dryer I Downstairs cloakroom (to houses) I Carpets I Private rear garden (to some) I Dedicated parking space I 10 year NHBC warranty AFFOR DAB LE Affinity Sutton is delighted to offer these brand new homes at Drayton Park, Cosham for sale on a shared ownership (part buy/part ren t) basis. This innovative scheme helps people who are unable to buy a property outright. You buy a share (2 5- 75%) and pay a reduced rent on the remaining share. At a later stage you can buy more shares until you own 100% of the property. This is an affordable way to buy, being often cheaper then renting privately. Affinity Suttonat DRAYTON PARK HELPING PEOPLE Lower Drayton Lane, Cosham, PUT D OWN ROOTS Portsmouth, Hampshire, PO6 2LB LOCATION t Road Havant Road Havan Albert Road Central Road Hilary Avenue Dysart Av e enue n a a e L n n a L o t t t e y d r e a a u r r t o Kn o S D o R w C sle Lonsdale Avenue y r h Ro n a e g d o i i w R t H o o se O a t COSHAM bury ld Mano L r S d Aven Way a ue o Grove Road R n r e h t r d Hawthor a n o Cre N o sen Cosham R t Park h Cha t tswo u rth Drayton Park o Ave m nue rts Highbu Po ry G rove d a o R n o A27 t l a W A27 Sc oad ott litary R Ro Mi ad A27 Located at Lower Drayton, Cosham and adjacent to Drayton Park, this popular suburb of Portsmouth benefits from good transports links and local amenities. -

The Postal History of Waterlooville Including Cosham, Widley, Purbrook, Denmead, Hambledon, Cowplain, Lovedean, Horndean and Chalton
The Postal History of Waterlooville including Cosham, Widley, Purbrook, Denmead, Hambledon, Cowplain, Lovedean, Horndean and Chalton by Mike Hill July 2015 £5 Tourist Map of 1991 showing the locations of Post Offices in the Waterlooville area. 2 Havant Borough History Booklet No. 52 To view, comment, and order all booklets visit: www.hhbkt.com Read also Booklet No. 38: A History of the Post Office in the Havant Area Edited by Ralph Cousins 3 4 The Postal History of Waterlooville including Cosham, Widley, Purbrook, Denmead, Hambledon, Cowplain, Lovedean, Horndean and Chalton Mike Hill Introduction The Waterlooville Philatelic Society was formed at the time of the great stamp collecting boom of the early 1970s and as a founder member I discovered that there was little information about the postal history of the local area since the founding of the village in 1815 some 200 years ago. Thus I was encouraged to start out on a journey of exploration into the history of postal services in the local area, a journey which has given me many hours of enjoyment. What I have achieved has been helped enormously by those of the Waterlooville Philatelic Society notably the late Eric Whyley and Mike English, and also the late Geoffrey Salter of the Waterlooville Library. Much of my research was published in the Journal of the Hampshire Postal History Society of which I was editor for a number of years. I must also thank David Coxon whose father took over from George Pook as postmaster in the early fifties for his memories and Paul Costen [www.costen.co.uk] who allowed me access to his scanned collection of postcards to search for Post Offices. -
AQUIND Limited AQUIND INTERCONNECTOR Consultation Report – Appendix 1.4C Statutory Consultation - List of Consultees Consulted Under Section 42(1)(D) PA 2008
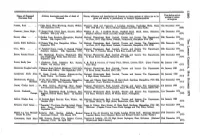
AQUIND Limited AQUIND INTERCONNECTOR Consultation Report – Appendix 1.4C Statutory Consultation - List of Consultees Consulted under Section 42(1)(d) PA 2008 The Planning Act 2008 The Infrastructure Planning (Applications: Prescribed Forms and Procedure) Regulations 2009 – Regulation 5(2)(q) Document Ref: 5.1.4C PINS Ref.: EN020022 AQUIND Limited AQUIND Limited AQUIND INTERCONNECTOR Consultation Report – Appendix 1.4 C Statutory Consultation - List of Consultees Consulted under Section 42(1)(d) PA 2008 PINS REF.: EN020022 DOCUMENT: 5.1.4C DATE: 14 NOVEMBER 2019 WSP WSP House 70 Chancery Lane London WC2A 1AF +44 20 7314 5000 www.wsp.com AQUIND Limited Contact Name Address Line 1 Address Line 2 Address Line 3 Address Line 4 Address Line 5 Town County Postcode InternationalPostcode Country Julie Elliott 9, The Gardens Waterlooville PO7 4RR United Kingdom EI Group plc 3 Monkspath Hall Road Shirley Solihull B90 4SJ United Kingdom Highways England Company Limited Care Of The Company Secretary Bridge House 1 Walnut Tree Close Guildford Surrey GU1 4LZ United Kingdom Southern Gas Networks plc St Lawrence House Station Approach Horley Surrey RH6 9HJ United Kingdom Hampshire County Council The Castle Castle Avenue Hants Winchester SO23 8UJ United Kingdom Shell U.K. Limited Shell Centre York Road London SE1 7NA United Kingdom E & L Berg Limited 236 Grays Inn Road London WC1X 8HB United Kingdom Asda Stores Limited Asda House Southbank Great Wilson Street Leeds LS11 5AD United Kingdom Portsmouth City Council c/o Tristan Samuels Director of Regeneration -

Portsmouth Mainline and Island Line
PORTSMOUTH MAINLINE AND ISLAND LINE On 19 May 2019, South Western Railway will be introducing changes to its timetable, adding over 300 train services per week across the network. Many of these service enhancements are based on consultations that were undertaken with stakeholders. We are very pleased to see these improvements come to fruition. The highlights for the Portsmouth direct line are: • Additional peak hour services on the Portsmouth direct line • Additional services between Waterloo and Hedge End, Botley, Fareham • Additional late evening weekday services to / from Waterloo and Haslemere / Portsmouth • Additional Sunday afternoon fast Waterloo – Portsmouth and Southsea services in both directions (routed via Cobham) • Doubling of the frequency of services at Godalming • New Farnham to Guildford service • The Island Line summer Sunday service of two trains per hour will continue throughout the winter • The detailed changes to the Portsmouth direct and Island Line services have been grouped below as follows: • New, extended or reduced services • Changes to stopping patterns (some of these are incorporated in 1. above) New Extended or Reduced Services Mondays to Fridays Additional AM peak services • 05.12 Portsmouth Harbour to Waterloo (06.51) additional service calling at Portsmouth & Southsea (05.17), Fratton (05.21), Havant (05.30), Petersfield (05.44), Haslemere (05.57), Godalming (06.07), Guildford (06.15), Worplesdon (06.20), Woking (06.27) • 05.45 Waterloo to Portsmouth Harbour (07.51) additional service calling at Clapham -
Surname First) Notices of Claims O Deceased Given and Names, in Parentheses, of Personal Representatives to Be Given
O Name of Deceased Address, description and date of death of Names, addresses and descriptions of Persons to whom notices of claims are to be Date before which oo (Surname first) notices of claims O Deceased given and names, in parentheses, of Personal Representatives to be given PACKER, Rosa 7 Elgin Road, West Worthing, Sussex, Widow. Thomson Snell and Passmore, 3 Lonsdale Gardens, Tunbridge Wells, Kent, 31st December 1979 16th September 1979. TNI 1NX (Ref. 51). (Harry Michael Aspinall and Peter John Snell.) (028) GORMLEY, James Hugh... 27 Bengal Road, Ilford, Essex, Security Officer Whisker & Co., 3 Oakfield House, Oakfield Road, Ilford, Essex, Solicitors. 19th December 1979 (Retired). 20th July 1979. (Stephen Bernard Thirsk and John Joseph Roberts.) (029) SWAIN, Aline 8 Garden Lane, Southsea, Hampshire, Married National Westminster Bank Limited, Trustee and Income Tax Department, 20th December 1979 Women. 10th August 1979. 1st Floor, 69-73 High Street, Cosham, Portsmouth, Hampshire PO6 SDH (721) LUKER, Edith Kathleen... 22 Dennis Way, Liss, Hampshire, Widow. 7th National Westminster Bank Limited, Trustee and Income Tax Department, 20th December 1979 W September 1979. 1st Floor, 69-73 High Street, Cosham, Portsmouth, Hampshire, PO6 3DH. (722) GILL, Mary 31 Parkfield Grove, Leeds 11, Retired Clerical National Westminster Bank Limited, Trustee and Income Tax Department, 20th December 1979 Assistant, Spinster. 25th September 1979. P.O. Box 17, Priestley House, 3 Park Row, Leeds LSI SLA. (723) EASON, Ronald Ernest ... The Hcathrings, Rivacres, Whitchurch Hill, National Westminster Bank Limited, Trustee and Income Tax Department, 20th December 1979 i near Pangbourne, Berks, Sales Director. 26th SA Broad Street, Reading, Berkshire, RG1 2BH. -

Public Transport Information Map Bus • Coach • Ferry • Train
Public transport information map Bus • Coach • Ferry • Train VALID FROM FEBRUARY 2017 To Waterlooville To Waterlooville T E 8 K C E I N H a m H 20 p A T s D L P I A E G h Widley H 7 Fort Southwick O T E N S O i R R O N O U W H H T PAR K H I r K A ENUE O V W D O I U L Crookhorn C O To South Downs K E S N R E Y College e C R O O M A D D I LE L A L N D AD A L O N E R W E E 8 O TH LEG L O Portsdown A L C L A L JAMES CALLAG K H N AN DRIV E E OW E THE BR N M27 M Fort Widley A OTORWA L Y 18 POR City of TSDOWN Paulsgrove HI Fort Purbrook N LL Portsmouth R OVE MO RO 20 ANSON GR L NDSB AD O NUE A UR Golf Course VE H I Y LI H A LL R ME GROVE Portsdown K 7 N ROAD SLE O 18 LTO Y A O R G CA D CRE SO N ST SCENT U O E R I O UR TH S H L W R N EO I A R MINSTER BLAKEMERE I D W ROAD C CK R R E E C W S P O R COLERIDG E C H T S D O I O E L W E L N O E R HAR 2.3 R H I D N L L 18 O E L D S O R E T Portsdown D O L TON N R A R OA . -

Portsmouth Pharmacies Providing Emergency Hormonal Contraception
Portsmouth Pharmacies Providing Emergency Hormonal Contraception (EHC) Bobat Pharmacy 92 Tangier Rd, Portsmouth PO3 6HU 02392 663945 Berry’s Chemist 145 Sultan Road, Portsmouth PO2 7AT 02392 822022 Boots the Chemist 194-204 Commercial Road, Portsmouth PO1 1HB 02392 825245 Boots the Chemist 25 London Road, North End, Portsmouth PO2 0BQ 02392 663911 Boots the Chemist 31-33 Palmerston Road, Southsea, Portsmouth PO5 3QQ 02392 821046 Boots the Chemist 48 High Street, Cosham, Portsmouth PO6 3AG 02392 375118 Boots the Chemist Unit 85a and b, Gunwharf Quays, Portsmouth PO1 3TZ 02392 750223 City Pharmacy 113 London Road, North End, Portsmouth PO2 0BN 02392 663836 Copnor Pharmacy 336 Copnor Road, Portsmouth PO3 5EL 02392 662511 Drayton Pharmacy 264B Havant Rd, Drayton, Portsmouth PO6 1PA 02393 070624 Everetts Chemist 58-60 High Street, Cosham PO6 3AG 02392 375979 Goldchem Pharmacy 147-147a Albert Road, Southsea, Portsmouth PO4 0JW 02392 731680 Lalys Chemist 162-166 Fawcett Road, Southsea, Portsmouth PO4 0DW 02392 781400 Lalys Chemist 3-5 Kingston Road, Portsmouth PO1 5RX 02392 831112 Lalys Chemist 6 London Road, Portsmouth PO2 0LH 02392 666625 Lalys Chemist 1 Guildhall Walk, Portsmouth PO1 2RY 02392 297293 Lloyds Pharmacy 122 Highlands Road, Southsea, Portsmouth PO4 9NQ 02392 830926 Lloyds Pharmacy 145-147 Somers Road, Southsea, Portsmouth PO5 4PT 02392 831911 Lloyds Pharmacy 52 High Street, Cosham, Portsmouth PO6 3AG 02392 383429 Lloyds Pharmacy 67 Milton Road, Copnor, Portsmouth PO3 6AN 02392 816993 8e Fratton Way, Pompey Centre, Fratton, Portsmouth -

'Petersfield House' 5 Boundary Way, Cosham
‘PETERSFIELD HOUSE’ 5 BOUNDARY WAY, COSHAM, PORTSMOUTH, HAMPSHIRE ‘PETERSFIELD HOUSE’ ‘Petersfield House’ is not what you would expect when step over the threshold of this detached family home, it retains many of the original features including, high curved ceilings, light, well proportioned and spacious rooms with a welcoming atmosphere, however the internal accommodation has been sympathetically and sensitively updated to provide a contemporary style with an open layout on the ground floor but yet retaining the traditional four bedrooms and bathroom upstairs. The accommodation is arranged over two floors and provides over 2,040 sq ft of living space which includes an impressive single storey extension which incorporates a dining room / family room and ‘Alno’ fully fitted quality kitchen, there is a separate cloakroom, large hallway, study / home office and interlinking drawing room as well as a garage on the first floor with four bedrooms and a bathroom on the first floor. The family/dining room opens up via bi-folding doors onto a split level rear garden with a southerly aspect and to the front are views over rooftops of neighbouring properties towards woodland and fields in the distance. Located in a cul-de-sac of only fourteen similar aged properties and being within the catchment for both Springfield and Court Lane Schools early internal viewing of this truly impressive family home is strongly recommended in order to appreciate both the accommodation and location on offer. WALK THROUGH ACCOMMODATION ENTRANCE: STUDY / HOME OFFICE -

Train Passes – Termly Prices & How to Order a College Train Pass 2020/2021
Train Passes – Termly Prices & How to Order a College Train Pass 2020/2021 South Western Railway are offering full-time HSDC students discounted train passes for the below train stations. In addition to this discount, the College will reduce the cost of the train pass further. The final cost of the train pass is as detailed in the tables below. Your train pass can be used 7 days a week, between the two stations you have requested. Your pass can be used in half terms, but not main holidays. The passes are valid on any Train Operating Company that operates on the route specified on the ticket. The Department of Transport have also launched a railcard for 16-17 year olds. The railcard costs £30 and offers up to 50% off rail fares. HSDC recognise that some train passes will still be cheaper through the College, however, we would still encourage students to investigate the 16-17 railcard scheme before purchasing a college train pass. For more information on the 16-17 railcard scheme, please see: https://www.16-17saver.co.uk/ College Train Passes: If you pay for a train pass by 3rdAugust 2020, we guarantee that we will order your train pass and it will be ready for collection at the start of term. We will still process applications after this date but during this busy period, your train pass may take a few weeks to arrive at college. Please keep checking in the Student Travel & Support Office to see if it has arrived. You are liable to pay your own travel costs until your train pass arrives.