Enc 13 Emergency Responsiveness Policy And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Publications List
Doncaster & District Family History Society Publications List August 2020 Parishes & Townships in the Archdeaconry of Doncaster in 1914 Notes The Anglican Diocese of Sheffield was formed in 1914 and is divided into two Archdeaconries. The map shows the Parishes within the Archdeaconry of Doncaster at that time. This publication list shows Parishes and other Collections that Doncaster & District Family History Society has transcribed and published in the form of Portable Document Files (pdf). Downloads Each Parish file etc with a reference number can be downloaded from the Internet using: www.genfair.co.uk (look for the Society under suppliers) at a cost of £6 each. Postal Sales The files can also be supplied by post on a USB memory stick. The cost is £10 each. The price includes the memory stick, one file and postage & packing. (The memory stick can be reused once you have loaded the files onto your own computer). Orders and payment by cheque through: D&DFHS Postal Sales, 18 Newbury Way, Cusworth, Doncaster, DN5 8PY Additional files at £6 each can be included on a single USB memory stick (up to a total of 4 files depending on file sizes). Example: One USB memory stick with “Adlingfleet” Parish file Ref: 1091 = £10. 1st Additional file at £6: the above plus “Adwick le Street” Ref: 1112 = Total £16. 2nd Additional file at £6: “The Poor & the Law” Ref: 1125 = Total £22 Postage included. We can also arrange payment by BACs, but for card and non-sterling purchases use Genfair While our limited stocks last we will also supply files in the form of a CD at £6 each plus postage. -

To Registers of General Admission South Yorkshire Lunatic Asylum (Later Middlewood Hospital), 1872 - 1910 : Surnames L-R
Index to Registers of General Admission South Yorkshire Lunatic Asylum (Later Middlewood Hospital), 1872 - 1910 : Surnames L-R To order a copy of an entry (which will include more information than is in this index) please complete an order form (www.sheffield.gov.uk/libraries/archives‐and‐local‐studies/copying‐ services) and send with a sterling cheque for £8.00. Please quote the name of the patient, their number and the reference number. Surname First names Date of admission Age Occupation Abode Cause of insanity Date of discharge, death, etc No. Ref No. Laceby John 01 July 1879 39 None Killingholme Weak intellect 08 February 1882 1257 NHS3/5/1/3 Lacey James 23 July 1901 26 Labourer Handsworth Epilepsy 07 November 1918 5840 NHS3/5/1/14 Lack Frances Emily 06 May 1910 24 Sheffield 30 September 1910 8714 NHS3/5/1/21 Ladlow James 14 February 1894 25 Pit Laborer Barnsley Not known 10 December 1913 4203 NHS3/5/1/10 Laidler Emily 31 December 1879 36 Housewife Sheffield Religion 30 June 1887 1489 NHS3/5/1/3 Laines Sarah 01 July 1879 42 Servant Willingham Not known 07 February 1880 1375 NHS3/5/1/3 Laister Ethel Beatrice 30 September 1910 21 Sheffield 05 July 1911 8827 NHS3/5/1/21 Laister William 18 September 1899 40 Horsekeeper Sheffield Influenza 21 December 1899 5375 NHS3/5/1/13 Laister William 28 March 1905 43 Horse keeper Sheffield Not known 14 June 1905 6732 NHS3/5/1/17 Laister William 28 April 1906 44 Carter Sheffield Not known 03 November 1906 6968 NHS3/5/1/18 Laitner Sarah 04 April 1898 29 Furniture travellers wife Worksop Death of two -

Doncaster, Rotherham and District Motor Trades Group Training Association Limited Inspection Report
Doncaster, Rotherham and District Motor Trades Group Training Association Limited Inspection report Unique reference number: 51579 Name of lead inspector: John Grimmer HMI Last day of inspection: 13 May 2011 Type of provider: Independent learning provider Rands Lane Industrial Estate Armthorpe Address: Doncaster South Yorkshire DN3 3DY Telephone number: 01302 832831 Published date June 2011 Inspection Number 366036 Inspection Report: Doncaster, Rotherham and District Motor Trades GTA Ltd, 13 May 2011 2 of 18 Information about the provider 1. Doncaster, Rotherham and District Motor Trades Group Training Association Limited (Doncaster GTA) is a private training provider and a registered charity. Founded in 1972, it became a company limited by guarantee in 1985. It specialises in training for the motor trade and road haulage industries and has contracts with major international motor manufacturers. It contracts with Yorkshire and the Humber Skills Funding Agency for the provision of work- based learning in motor vehicle engineering and business administration. Doncaster GTA also offers commercial training for other international, national and local companies, including lift truck training, goods vehicle driving, dangerous goods and health and safety consultation. The commercial training accounts for approximately 35% of its income. 2. The company has two training centres, one at Armthorpe on the outskirts of Doncaster and the other in Sheffield. Both sites have a comprehensive range of specialist training workshops and classrooms for motor vehicle, business administration, and warehouse training. 3. Doncaster GTA has a board of directors from the local retail vehicle repair sector which oversees strategic planning and monitors the company’s performance. Doncaster GTA has 20 member companies, but deals with approximately 150 employers throughout the Doncaster, Rotherham and Sheffield area. -
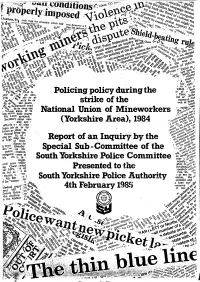
Policing-Policy-During-Strike-Report
' The Police Committee Special Sub-Committee at their meeting on 24 January 19.85 approved this report and recommended that it should be presented to the Police Committee for their approval. In doing so, they wish to place on record their appreciation and gratitude to all the members of the County Council's Department of Administration who have assisted and advised the Sub-Committee in their inquiry or who have been involved in the preparation of this report, in particular Anne Conaty (Assistant Solicitor), Len Cooksey (Committee Administrator), Elizabeth Griffiths (Secretary to the Deputy County Clerk) and David Hainsworth (Deputy County Clerk). (Councillor Dawson reserved his position on the report and the Sub-Committee agreed to consider a minority report from him). ----------------------- ~~- -1- • Frontispiece "There were many lessons to be learned from the steel strike and from the Police point of view the most valuable lesson was that to be derived from maintaining traditional Police methods of being firm but fair and resorting to minimum force by way of bodily contact and avoiding the use of weapons. My feelings on Police strategy in industrial disputes and also those of one of my predecessors, Sir Philip Knights, are encapsulated in our replies to questions asked of us when we appeared before the House of Commons Select Committee on Employment on Wednesday 27 February 1980. I said 'I would hope that despite all the problems that we have you will still allow us to have our discretion and you will not move towards the Army, CRS-type policing, or anything like that. -

~ 170 ~ 8. Bibliography
Peat exploitation on Thorne Moors. A case- study from the Yorkshire-Lincolnshire border 1626-1963, with integrated notes on Hatfield Moors Item Type Thesis Authors Limbert, Martin Rights <a rel="license" href="http://creativecommons.org/licenses/ by-nc-nd/3.0/"><img alt="Creative Commons License" style="border-width:0" src="http://i.creativecommons.org/l/by- nc-nd/3.0/88x31.png" /></a><br />The University of Bradford theses are licenced under a <a rel="license" href="http:// creativecommons.org/licenses/by-nc-nd/3.0/">Creative Commons Licence</a>. Download date 28/09/2021 03:56:39 Link to Item http://hdl.handle.net/10454/5454 8. BIBLIOGRAPHY Anon. (1867) Handbook for Travellers in Yorkshire. London: John Murray. Anon. [1876] The Life and Eccentricities of Lionel Scott Pilkington, alias Jack Hawley, of Hatfield, near Doncaster. Doncaster: Edward Dale, Free Press Office. Anon. (1885) Turf-bedding. Chambers’s Journal 2 (Fifth Series): 535-536. Anon. (1900) Peat as a Substitute for Coal. The Colliery Guardian, and Journal of the Coal and Iron Trades 80: 373. Anon. (1907) The Ziegler System of Peat Utilisation. Engineering 84: 671-675. Anon. [1946] The Process of Warping. In: Goole Rural District. The Official Handbook. Guide No. 121. London: Pyramid Press. Anon. (1949) Horticultural Peat. Sport and Country 187: 39-41. Anon. [1993] Thorne Landowners & Tenants 1741. Thorne Local History Society Occasional Papers No.13. [Appleton, E.V.] (1954) Report of the Scottish Peat Committee. 31 July 1953. House of Lords Papers and Bills No. 49-393. Scottish Home Department. Edinburgh: HMSO. Ashforth, P., Bendall, I. -

Armthorpe Welfare FC Sponsorship Brochure
Marra Falcons Stadium, Church Street, Armthorpe, Doncaster, DN3 3AG Members of the Toolstation NCEL st 1 Division, West Riding CFA & The Football Association #Upthewellie Formed in 1976, Armthorpe Welfare FC currently play our football in the Toolstation Northern Counties East Football League First Division and have been run by hard working volunteers for over 40 years. We are a family friendly club at the heart of our community and we rely upon the support of this community and local businesses to maintain our proud tradition of grass roots football. There are however huge financial costs involved in running a team at this level from league fees, referee’s fees and utility bills, to kit and equipment costs and essential ground and pitch maintenance. All of these costs are funded solely through many local businesses who sponsor our club in various ways. Without the support of these businesses, we would not be in existence, and we are very appreciative of those who help us. The league we compete in involves teams as far reaching as Bradford, Harrogate, Hull, Skegness and Nottingham, and more locally in Doncaster, Leeds, Sheffield, Barnsley, Scunthorpe and Wakefield, providing widespread exposure of your company to thousands of supporters. We also compete in the national Football Association competitions - the famous FA Cup and the FA Vase. In addition we compete in a County FA Cup contested by teams in the West Riding of Yorkshire, culminating in a final that is played at a football league ground. We have a number of sponsorship opportunities available to suit businesses and individuals alike, so why not show your support for the club whilst gaining some extra exposure for your business, or just for yourself? Pitchside Advertising Boards We have a great opportunity to advertise with the club via our pitch-side advertising boards. -

Sheffield to Cleethorpes
Torchbearer Street Route 39 Tuesday, 26 June 2012 Day Time Community Travelling On 39 07:40 Sheffield Leeds Road 39 sHeffield Leeds Road - Right Turn 39 Sheffield Worksop Road (B6085) - Right Turn 39 Sheffield Attercliffe Road (A6178) 39 Sheffield Attercliffe Common - Right Turn 39 Sheffield Coleridge Road - Left Turn 39 Sheffield Don Valley Bowl - Left Turn 39 Sheffield Terry Street - Right Turn 39 Sheffield Attercliffe Common (A6178) 39 Sheffield Sheffield Road (A6178) to Murco Service 39 CONVOY: Sheffield - Rotherham Station 39 08:51 Rotherham Sheffield Road from Marsh Street Junction 39 Rotherham Westgate 39 Rotherham High Street - Left Turn 39 Rotherham Church Street - Right Turn 39 Rotherham All Saints Square - Right Turn 39 Rotherham College Street - Left Turn 39 Rotherham Doncaster Gate 39 Rotherham Doncaster Gate - Right Turn 39 Rotherham Clifton Park 39 Rotherham Clifton Park- Right Turn 39 Rotherham Doncaster Road 39 Rotherham Doncaster Road- Left Turn 39 Rotherham Herringthorpe Valley Road (A6123)- Right Turn 39 09:25 Dalton Doncaster Road (A630) 39 09:32 Thrybergh Doncaster Road (A630) 39 Thrybergh Doncaster Road (A630) to Chestnut Court 39 CONVOY: Thrybergh - Conisbrough Junction 39 09:50 Conisbrough Old Road from Hill Top Road Junction 39 Conisbrough Church Street 39 Conisbrough Castle Street 39 Conisbrough Castle Hill 39 Conisbrough Castle Hill- Right Turn 39 Conisbrough Low Road (A6023)- Left Turn 39 Conisbrough Doncaster Road (A630) To National Speed 39 CONVOY: Conisbrough - Warmsworth Limit Signs 39 10:23 Warmsworth -

South Yorkshire
INDUSTRIAL HISTORY of SOUTH RKSHI E Association for Industrial Archaeology CONTENTS 1 INTRODUCTION 6 STEEL 26 10 TEXTILE 2 FARMING, FOOD AND The cementation process 26 Wool 53 DRINK, WOODLANDS Crucible steel 27 Cotton 54 Land drainage 4 Wire 29 Linen weaving 54 Farm Engine houses 4 The 19thC steel revolution 31 Artificial fibres 55 Corn milling 5 Alloy steels 32 Clothing 55 Water Corn Mills 5 Forging and rolling 33 11 OTHER MANUFACTUR- Windmills 6 Magnets 34 ING INDUSTRIES Steam corn mills 6 Don Valley & Sheffield maps 35 Chemicals 56 Other foods 6 South Yorkshire map 36-7 Upholstery 57 Maltings 7 7 ENGINEERING AND Tanning 57 Breweries 7 VEHICLES 38 Paper 57 Snuff 8 Engineering 38 Printing 58 Woodlands and timber 8 Ships and boats 40 12 GAS, ELECTRICITY, 3 COAL 9 Railway vehicles 40 SEWERAGE Coal settlements 14 Road vehicles 41 Gas 59 4 OTHER MINERALS AND 8 CUTLERY AND Electricity 59 MINERAL PRODUCTS 15 SILVERWARE 42 Water 60 Lime 15 Cutlery 42 Sewerage 61 Ruddle 16 Hand forges 42 13 TRANSPORT Bricks 16 Water power 43 Roads 62 Fireclay 16 Workshops 44 Canals 64 Pottery 17 Silverware 45 Tramroads 65 Glass 17 Other products 48 Railways 66 5 IRON 19 Handles and scales 48 Town Trams 68 Iron mining 19 9 EDGE TOOLS Other road transport 68 Foundries 22 Agricultural tools 49 14 MUSEUMS 69 Wrought iron and water power 23 Other Edge Tools and Files 50 Index 70 Further reading 71 USING THIS BOOK South Yorkshire has a long history of industry including water power, iron, steel, engineering, coal, textiles, and glass. -

Domesday Book Translation
Translation of Great Domesday Book Folio 379r WEST RIDING In the geld of the city of York are 84 carucates of land, which TRE paid, each of them, as much geld as 1 house in the city. Of these, the archbishop has 6 carucates [belonging] to the farm of his hall. In Osbaldwick, the archbishop 6 carucates. In Murton [in Osbaldwick], 4 carucates. In Stockton on the Forest, the archbishop 3 carucates. In the same place, 3 carucates. In Sandburn, 3 carucates. In Heworth, 3 carucates. In the same place, Count Alan 3 carucates. In Gate Fulford, Count Alan 10 carucates. In Clifton [near York], the archbishop 8½ carucates. In the same place, Count Alan 9½ carucates. In the same place, the archbishop 37 acres of meadow. In Rawcliffe, Seaxfrith had 2 carucates. In the same place, the king 1 carucate. In Overton, Count Alan 5 carucates. In Skelton [near York], the archbishop 3½ carucates. In the same place, the king 2 carucates and 6 bovates. In the same place, Count Alan 2 carucates and 6 bovates. In 'Mortona' [in Overton], Arnketil had 3 carucates. In Wiggington, the archbishop 3 carucates. Within the circuit of the city, 3 carucates. Thorfinnr and Thorkil held them. 'SKYRACK' WAPENTAKE In OTLEY , a manor, Pool, Guiseley, Hawksworth, and another Hawksworth [Thorpe, in Hawksworth], Baildon, Menston, Burley in Wharfedale [and] Ilkley, the archbishop 60 carucates and 6 bovates. Also in "GEREBURG" WAPENTAKE are these BEREWICKS of Otley: 'Stubham' [in Ilkley], Farnley [in Otley], Middleton [in Ilkley], Nether Timble, Denton, "Estone" [in Lindley], Clifton [near Newall] [and] 'Bikerton' [in Newall with Clifton]. -

NHS England Yorkshire & Humber Orthodontic Lots and Locations
NHS England Yorkshire & Humber Orthodontic Lots and Locations Total Number Postcodes Total No. of Locations within Postcodes Lot Name Servicing (including UOA's of UOA's (including but not exclusively) but not exclusively) Lots in Lot North Yorkshire & Humber Craven BD20, BD23, BD24 Crosshills, Settle, Skipton, Craven 6500 1 6500 Grassington Harrogate HG1, HG2, HG3, Harrogate, Knaresborough, Ripon, Harrogate 10318 1 10318 HG4, HG5, YO51, Boroughbridge, Marston Moor YO26 Ward Hambleton and DL6, DL7, DL8, Leeming, Leyburn, Thirsk, Hambleton and 8606 1 8606 Richmondshire DL9, DL10, DL11, Northallerton, Richmond, Richmondshire YO7, YO61 Easingwold Scarborough YO11, YO12, Scarborough, Scalby, Seamer Scarborough and and Ryedale YO13, YO14, Ward, East Ayton, Filey, 9682 1 9682 Ryedale YO17, YO18, Hunmanby, Malton, Pickering, YO62, YO21,YO60 Helmsley, Whitby Selby YO8,LS24, LS25, Selby, Sherburn in Elmet, Selby 6500 1 6500 Tadcaster York YO1, YO10, YO19, Acomb, Bishopthorpe, York 10376 1 10376 YO23, YO24, Dunnington, Haxby, Rawcliffe, YO26, YO30, YO32 East Riding - YO15, YO16,YO25, Bridlington, Flamborough, North East HU18, HU10, Holderness Ward, East Wolds and HU11, HU12, Coastal Ward, Hornsea, Mid East Riding 19699 2 9850 HU13, HU14, Holderness Ward, North HU16, HU17, Holderness Ward, Withernsea, HU18, HU19 Hessle, Beverley, Cottingham East Riding - YO25, YO41, Pocklington, Howdenshire Ward, West YO42, YO43, Goole, Hessle, Beverley, 9850 HU10, HU13, Cottingham, Driffield HU14, HU15, HU16, HU17, DN14 Hull East HU1, HU2, HU7, Branshome, Sutton -

South Yorkshire's Community Foundation
South Yorkshire’s Community Foundation Social Impact Report 2015 “Our contribution to our community” Introduction Welcome to South Yorkshire Community Foundation’s Impact Report. Year by year, for the last 29 years, South Yorkshire Community Foundation has continued to inspire community giving and support local communities to tackle important social issues. This report has been created to demonstrate “…the good we secure for ourselves is the real impact and social change, which is precarious and uncertain until it is secured for achieved through community giving and all of us and incorporated into our common community grants. life”. As an organisation we strongly believe in the Social inclusion, community cohesion and a importance of the community and aim to sense of togetherness has the power to alter improve the lives of those who are a part of the world in which we live in. it; through providing philanthropy services This is why we are devoted to raising and and raising funds from individuals, families, businesses, philanthropists, trusts and distributing funds to local projects and statutory bodies and using them to meet organisations who have our communities’ the needs of local people facing economic best interests at heart. hardship and other barriers to aspiration. The collective well-being of the South Yorkshire community is of importance to us. As Jane Addams once said I am proud to be able to present South Yorkshire Community Foundations social impact report, which introduces you to a number of inspiring stories and amazing people. We are publishing this report so that these achievements can be recognised and celebrated. -

Repeat Prescriptions
Auckley Surgery ________________________________________________________________________________________________________________ Dr Felcy Alex (MB. BS., MRCGP) 41 Ellers Lane Auckley Doncaster DN9 3HY Tel: 01302 770327 Fax: 01302 771302 Practice Information Leaflet Welcome to Auckley Surgery Our surgery serves patients in the areas of Auckley, Branton, Finningley, Blaxton, Rossington, Cantley, Bessacarr and Armthorpe. Our team includes 2 GPs, 2 Practice Nurses and Practice Manager, Secretary, Dispenser and Reception staff. Here is a current list of staff:- Dr F Alex MB. BS., MRCGP Dr E Ashdown BSc, DRCOG, MBChB, MRCGP Elizabeth Walsh Practice Manager Margaret Scamans Senior Practice Nurse Christine Seymour Practice Nurse/Nurse Prescriber Chris Kisby Secretary Linda Hale Dispensary Lynn Tilston Receptionist/Admin Caroline Gillon Receptionist/Dispensary Jacky Carmody Receptionist/Dispensary Maria Parkes Receptionist PRACTICE CHARTER Our Charter sets out the standards to which we are working. It is our commitment to provide a quality service and care to all our patients. This can only be achieved by working together and by having a clear understanding of each others needs. We respect the need for privacy and all records or information regarding each individual patient will be completely confidential. Please note that all patients are entitled to have access to their written and computerised health records within the limitations of the law, at the discretion of the Doctor. All patients have the right within the law to express a preference of their own choice of a general practitioner within the surgery in accordance with paragraph 13.8 of the GMS contract. PRACTICE LEAFLET: The practice leaflet is incorporated within the charter booklet. It outlines surgery times and explains in detail all services offered at the practice by ourselves and other attached staff i.e.