Clinical Features and Outcomes of 197 Adult Discharged Patients with COVID-19 in Yichang, Hubei Fating Zhou1,2*, Xiaogang Yu1,2, Xiaowei Tong, Rong Zhang1,2 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Landscape Analysis of Geographical Names in Hubei Province, China
Entropy 2014, 16, 6313-6337; doi:10.3390/e16126313 OPEN ACCESS entropy ISSN 1099-4300 www.mdpi.com/journal/entropy Article Landscape Analysis of Geographical Names in Hubei Province, China Xixi Chen 1, Tao Hu 1, Fu Ren 1,2,*, Deng Chen 1, Lan Li 1 and Nan Gao 1 1 School of Resource and Environment Science, Wuhan University, Luoyu Road 129, Wuhan 430079, China; E-Mails: [email protected] (X.C.); [email protected] (T.H.); [email protected] (D.C.); [email protected] (L.L.); [email protected] (N.G.) 2 Key Laboratory of Geographical Information System, Ministry of Education, Wuhan University, Luoyu Road 129, Wuhan 430079, China * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel: +86-27-87664557; Fax: +86-27-68778893. External Editor: Hwa-Lung Yu Received: 20 July 2014; in revised form: 31 October 2014 / Accepted: 26 November 2014 / Published: 1 December 2014 Abstract: Hubei Province is the hub of communications in central China, which directly determines its strategic position in the country’s development. Additionally, Hubei Province is well-known for its diverse landforms, including mountains, hills, mounds and plains. This area is called “The Province of Thousand Lakes” due to the abundance of water resources. Geographical names are exclusive names given to physical or anthropogenic geographic entities at specific spatial locations and are important signs by which humans understand natural and human activities. In this study, geographic information systems (GIS) technology is adopted to establish a geodatabase of geographical names with particular characteristics in Hubei Province and extract certain geomorphologic and environmental factors. -

Download Article
Advances in Economics, Business and Management Research, volume 70 International Conference on Economy, Management and Entrepreneurship(ICOEME 2018) Research on the Path of Deep Fusion and Integration Development of Wuhan and Ezhou Lijiang Zhao Chengxiu Teng School of Public Administration School of Public Administration Zhongnan University of Economics and Law Zhongnan University of Economics and Law Wuhan, China 430073 Wuhan, China 430073 Abstract—The integration development of Wuhan and urban integration of Wuhan and Hubei, rely on and Ezhou is a strategic task in Hubei Province. It is of great undertake Wuhan. Ezhou City takes the initiative to revise significance to enhance the primacy of provincial capital, form the overall urban and rural plan. Ezhou’s transportation a new pattern of productivity allocation, drive the development infrastructure is connected to the traffic artery of Wuhan in of provincial economy and upgrade the competitiveness of an all-around and three-dimensional way. At present, there provincial-level administrative regions. This paper discusses are 3 interconnected expressways including Shanghai- the path of deep integration development of Wuhan and Ezhou Chengdu expressway, Wuhan-Ezhou expressway and from the aspects of history, geography, politics and economy, Wugang expressway. In terms of market access, Wuhan East and puts forward some suggestions on relevant management Lake Development Zone and Ezhou Gedian Development principles and policies. Zone try out market access cooperation, and enterprises Keywords—urban regional cooperation; integration registered in Ezhou can be named with “Wuhan”. development; path III. THE SPACE FOR IMPROVEMENT IN THE INTEGRATION I. INTRODUCTION DEVELOPMENT OF WUHAN AND EZHOU Exploring the path of leapfrog development in inland The degree of integration development of Wuhan and areas is a common issue for the vast areas (that is to say, 500 Ezhou is lower than that of central urban area of Wuhan, and kilometers from the coastline) of China’s hinterland. -

A Simple Model to Assess Wuhan Lock-Down Effect and Region Efforts
A simple model to assess Wuhan lock-down effect and region efforts during COVID-19 epidemic in China Mainland Zheming Yuan#, Yi Xiao#, Zhijun Dai, Jianjun Huang & Yuan Chen* Hunan Engineering & Technology Research Centre for Agricultural Big Data Analysis & Decision-making, Hunan Agricultural University, Changsha, Hunan, 410128, China. #These authors contributed equally to this work. * Correspondence and requests for materials should be addressed to Y.C. (email: [email protected]) (Submitted: 29 February 2020 – Published online: 2 March 2020) DISCLAIMER This paper was submitted to the Bulletin of the World Health Organization and was posted to the COVID-19 open site, according to the protocol for public health emergencies for international concern as described in Vasee Moorthy et al. (http://dx.doi.org/10.2471/BLT.20.251561). The information herein is available for unrestricted use, distribution and reproduction in any medium, provided that the original work is properly cited as indicated by the Creative Commons Attribution 3.0 Intergovernmental Organizations licence (CC BY IGO 3.0). RECOMMENDED CITATION Yuan Z, Xiao Y, Dai Z, Huang J & Chen Y. A simple model to assess Wuhan lock-down effect and region efforts during COVID-19 epidemic in China Mainland [Preprint]. Bull World Health Organ. E-pub: 02 March 2020. doi: http://dx.doi.org/10.2471/BLT.20.254045 Abstract: Since COVID-19 emerged in early December, 2019 in Wuhan and swept across China Mainland, a series of large-scale public health interventions, especially Wuhan lock-down combined with nationwide traffic restrictions and Stay At Home Movement, have been taken by the government to control the epidemic. -

Verification of Wind Field Retrieval of Doppler Radar Velocity-Azimuth
5.8 VERIFICATION OF WIND FIELD RETRIEVAL OF DOPPLER RADAR VELOCITY-AZIMUTH PROCESSING METHOD Zheng Yongguang1 Liu Shuyuan1 Bai Jie2 Tao Zuyu1 (1 Department of Atmospheric Sciences, School of Physics, Peking University, Beijing 100871, P. R. China; 2 Beijing Aviation Meteorological Institute, Beijing 100085, P. R. China) 1 PRINCIPLE OF VAP METHOD direction and the radar beam. The VAP (Velocity-Azimuth Processing) method was put forward for retrieving the horizontal wind field from single Doppler radar data by Tao Zuyu (1992). Assume that the horizontal wind vectors are uniform in L a very small azimuth interval (i. e., the local uniformity of wind field) and neglect the vertical fall speed of the r L’ particles of low elevation scan, the formula of horizontal wind retrieval based on the distribution of Doppler velocity profiles with azimuth are as follows Figure 1 A schematic diagram of the relation (see Fig. 1): between the wind vectors and the radial velocities on Wind speed: local uniform wind assumption. v − v v = hr1 hr 2 , 2sinα sin ∆θ Because spatial and temporal resolutions of the Wind direction: Doppler radar data are higher than all of other winds v − v observations, it is difficult to obtain the detail tanα = − hr1 hr 2 cot ∆θ = an vhr1 + vhr 2 information of wind field for objectively evaluating the results derived by VAP method. To prove the validity of α = arctan an, vhr1 − vhr 2 > 0,vhr1 + vhr 2 > 0 the meso-β-scale characteristics on the retrieved wind α = arctan an +π , vhr1 − vhr 2 > 0,vhr1 + vhr 2 < 0 fields by VAP method, Choi et. -

Comparison of the Effect Of
COMMENTARY Comment on “Comparison of the effect of ultrasound-guided thoracic paravertebral nerve block and intercostal nerve block for video- assisted thoracic surgery under spontaneous- ventilating anesthesia” Xuesong Liu1 Biyou Zheng1 Chenhong Huang1 Qiongya Wu1 Leyun Zhan1 1. Department of Anesthesiology, the People’s Hospital of China Three Gorges University, Hubei 443000 China http://dx.doi.org/10.1590/1806-9282.66.7.1009 Dear Editor, We read with great interest the study by Zheng example, the type of surgery. It is difficult to reach et al.1 in which they demonstrated that ultra - the conclusion that the frequency of vascular punc- sound-guided thoracic paravertebral nerve block was ture was different between the two groups. Vascular superior to ultrasound-guided intercostal nerve block puncture was noted in four patients in the intercostal during video-assisted thoracic surgery for pulmonary nerve block group and in one patient in the thoracic lobectomy under spontaneous-ventilating anesthe- paravertebral nerve block group for chronic pain. sia. In our opinion, there are some issues that should Thus, a study involving a larger sample should be con- be addressed. ducted to confirm the merit of thoracic paravertebral To begin with, this study was prospective. The nerve block. authors enrolled 50 patients for investigating the methods; however, 100 patients were included in the results section. Thus, the sample size should be con- REFERENCE firmed. Additionally, how many patients were lost 1. Zheng Y, Wang H, Ma X, Cheng Z, Cao W, Shao D. Comparison effect of during follow-up in this prospective study? ultrasound-guided thoracic paravertebral nerve block and intercostal nerve block for video-assisted thoracic surgery under spontaneous-ventilating Many factors may influence the results, for anesthesia. -
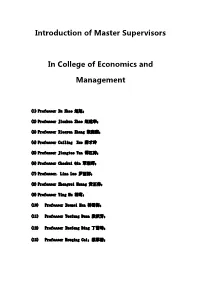
Introduction of Master Supervisors In
Introduction of Master Supervisors In College of Economics and Management (1) Professor Xu Zhao 赵旭; (2) Professor Jianhua Zhao 赵建华; (3) Professor Xiaoyan Zhang 张晓燕; (4) Professor Cailing Xue 薛才玲 (5) Professor Jiangtao Tan 谭江涛; (6) Professor Chaohui Qin 覃朝晖; (7) Professor. Lina Luo 罗丽娜; (8) Professor Zhengwei Huang 黄正伟; (9) Professor Ying Hu 胡莺; (10) Professor Xuemei Han 韩雪梅; (11) Professor Yuefang Duan 段跃芳; (12) Professor Xuefeng Ding 丁雪峰; (13) Professor Houqing Cai;蔡厚清; Curriculum Vitae Associate Professor Xu ZHAO PERSONAL & CONTACT DETAILS Name Xu ZHAO Academic Title PhD Management Science and Engineering Master of Management Bachelor of Engineering Postal Address College of Economics and Management,No.8 Daxue Road, Yichang City, Hubei Province, P.R. China 443002 Office Address Room G1602, G building , College of Economics and Management, China Three Gorges University Date/place of birth: August, 1982/ Yichang City, Hubei Province, P.R. China Telephone (Office): +86 - 717 -639 9458,mobile phone +86 18671785266 E-mail: [email protected] TERTIARY EDUCATION September 2010 – Huazhong University of Science and Technology, Wuhan, P.R. June 2014 China PhD February 2005 – China Three Gorges University, Yichang, P.R. China July 2008 Master of Management September 2000 – WUHAN University, Wuhan, P.R. China July 2004 Bachelor of Engineering Associate Professor XU ZHAO EMPLOYMENT July 2014 – Present College of Economics and Management ,China Three Gorges University. o Associate Professor at the College of Economics and Management o Research fellow of Research Centre for Reservoir Resettlement—the Key Humanities and Social Sciences Research Base of Hubei Province, China. o Teach the following subjects: Management Research Method, logistics system simulation, Computational Social Science, Social Network Analysis. -

CHN33885 – Three Gorges Dam – Protests – Bilharzia
Refugee Review Tribunal AUSTRALIA RRT RESEARCH RESPONSE Research Response Number: CHN33885 Country: China Date: 16 October 2008 Keywords: China – CHN33885 – Three Gorges Dam – Protests – Bilharzia This response was prepared by the Research & Information Services Section of the Refugee Review Tribunal (RRT) after researching publicly accessible information currently available to the RRT within time constraints. This response is not, and does not purport to be, conclusive as to the merit of any particular claim to refugee status or asylum. This research response may not, under any circumstance, be cited in a decision or any other document. Anyone wishing to use this information may only cite the primary source material contained herein. Questions 1.What is the measurement “mu”? 2. Information about the Three Gorges Dam, and forced acquisition of land, including compensation payable to displaced migrants. 3. Information about the worm parasite – Bilharzia. 4. Information about Hong Yunzhou, Tan Guotai, Chen Yichun, Zhou Zhirong and Fu Xiancai. 5. Is there any record of protests re the displaced migrants? RESPONSE 1.What is the measurement “mu”? A mu is a land measure equal to 0.067 hectares. Thus 100,000 mu is 6,700 hectares (‘China quintuples arable land use tax’ 2006, China Daily, 6 December http://www.chinadaily.com.cn/china/2007-12/06/content_6303895.htm – Accessed 16 April 2008 – Attachment 1). 2. Information about the Three Gorges Dam, and forced acquisition of land, including compensation payable to displaced migrants. The Three Gorges Dam, located in Hubei Province, is the world’s largest dam and will be fully operational in 2009. -

Research on Sustainable Land Use Based on Production–Living–Ecological Function: a Case Study of Hubei Province, China
sustainability Article Research on Sustainable Land Use Based on Production–Living–Ecological Function: A Case Study of Hubei Province, China Chao Wei 1, Qiaowen Lin 2, Li Yu 3,* , Hongwei Zhang 3 , Sheng Ye 3 and Di Zhang 3 1 School of Public Administration, Hubei University, Wuhan 430062, China; [email protected] 2 School of Management and Economics, China University of Geosciences, Wuhan 430074, China; [email protected] 3 School of Public Administration, China University of Geosciences, Wuhan 430074, China; [email protected] (H.Z.); [email protected] (S.Y.); [email protected] (D.Z.) * Correspondence: [email protected]; Tel.: +86-185-7163-2717 Abstract: After decades of rapid development, there exists insufficient and contradictory land use in the world, and social, economic and ecological sustainable development is facing severe challenges. Balanced land use functions (LUFs) can promote sustainable land use and reduces land pressures from limited land resources. In this study, we propose a new conceptual index system using the entropy weight method, regional center of gravity theory, coupling coordination degree model and obstacle factor identification model for LUFs assessment and spatial-temporal analysis. This framework was applied to 17 cities in central China’s Hubei Province using 39 indicators in terms of production–living–ecology analysis during 1996–2016. The result shows that (1) LUFs showed an overall upward trend during the study period, while the way of promotion varied with different dimensions. Production function (PF) experienced a continuous enhancement during the study period. Living function (LF) was similar in this aspect, but showed a faster rising tendency. -

46050-002: Hubei Huanggang Urban Environment Improvement Project
Environmental Impact Assessment (2nd Addendum) September 2018 PRC: Hubei Huanggang Urban Environment Improvement Project Prepared by Huanggang Municipal Government for the Asian Development Bank. {This is a revised version of the draft originally posted in January 2014 available on https://www.adb.org/projects/documents/hubei-huanggang-integrated-urban-environment- improvement-project-eia.} CURRENCY EQUIVALENTS (as of 31 August 2018) Currency unit – yuan (CNY) CNY1.00 = $0.14602 $1.00 = CNY6.84 In this report, $ refers to US dollars. ABBREVIATIONS ADB Asian Development Bank CN Cyanide CNY Chinese yuan EA Executing agency EHS Environmental Health System EIA Environmental impact assessment EIR Environmental impact report EIT Environmental impact table EMP Environmental management plan EMS Environmental monitoring station FSR Feasibility study report HEPB Huanggang Environmental Protection Bureau HMG Huanggang Municipal Government LIEC Loan implementation environmental consultant NO2 Nitrogen dioxide PMO Project management office SO2 Sulfur dioxide TN Total Nitrogen TP Total Phosphorus WWTP Wastewater treatment plant WEIGHTS AND MEASURES ha hectare hr hour kg/d kilogram per day km kilometer km2 square kilometer km/hr kilometer per hour L liter m meter m/s meter per second m2 square meter m3 cubic meter m3/d cubic meter per day cubic meter per m3/s second mg/kg milligram per kilogram mg/L milligram per liter NOTE In the report, ―$ refers to US dollars. This addendum to the environmental impact assessment is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section on ADB’s website. -

Study on Intangible Cultural Heritage Brands from the Perspective Of
International Conference on Education Technology, Management and Humanities Science (ETMHS 2015) Study on Intangible Cultural Heritage Brands from the Perspective of Ecological Protection Haimeng Li School of music, Hubei Normal University, Huangshi, 435002, China Keywords: ecological protection, intangible cultural heritage, brands Abstract: China has abundant intangible cultural heritage resources. However, economic development brings pressure to ecological environment, changes of which have direct influence on the protection of intangible cultural heritage. At current stage, due to lack of strong consciousness of intangible cultural heritage protection in many regions in China, a part of intangible cultural heritage is in imminent danger. Establishment of intangible cultural heritage brands means inheritance and development of intangible cultural heritage, and is also a way of intangible cultural heritage protection. This paper mainly studies on intangible cultural heritage brands from the perspective of ecological protection with an example of protection of intangible cultural heritage in Southeastern Hubei Province. As intangible cultural heritage has tourism value, various countries begin to attach importance to tourism development of intangible cultural heritage. However, unreasonable development is caused for many factors, which cannot inherit or develop intangible cultural heritage but lead to frequent problems in its protection. Establishment of intangible cultural heritage brands is an important way of intangible cultural development -

Table of Codes for Each Court of Each Level
Table of Codes for Each Court of Each Level Corresponding Type Chinese Court Region Court Name Administrative Name Code Code Area Supreme People’s Court 最高人民法院 最高法 Higher People's Court of 北京市高级人民 Beijing 京 110000 1 Beijing Municipality 法院 Municipality No. 1 Intermediate People's 北京市第一中级 京 01 2 Court of Beijing Municipality 人民法院 Shijingshan Shijingshan District People’s 北京市石景山区 京 0107 110107 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Haidian District of Haidian District People’s 北京市海淀区人 京 0108 110108 Beijing 1 Court of Beijing Municipality 民法院 Municipality Mentougou Mentougou District People’s 北京市门头沟区 京 0109 110109 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Changping Changping District People’s 北京市昌平区人 京 0114 110114 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Yanqing County People’s 延庆县人民法院 京 0229 110229 Yanqing County 1 Court No. 2 Intermediate People's 北京市第二中级 京 02 2 Court of Beijing Municipality 人民法院 Dongcheng Dongcheng District People’s 北京市东城区人 京 0101 110101 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Xicheng District Xicheng District People’s 北京市西城区人 京 0102 110102 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Fengtai District of Fengtai District People’s 北京市丰台区人 京 0106 110106 Beijing 1 Court of Beijing Municipality 民法院 Municipality 1 Fangshan District Fangshan District People’s 北京市房山区人 京 0111 110111 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Daxing District of Daxing District People’s 北京市大兴区人 京 0115 -

Are China's Water Resources for Agriculture Sustainable? Evidence from Hubei Province
sustainability Article Are China’s Water Resources for Agriculture Sustainable? Evidence from Hubei Province Hao Jin and Shuai Huang * School of Public Economics and Administration, Shanghai University of Finance and Economics, Shanghai 200433, China; [email protected] * Correspondence: [email protected]; Tel.: +86-21-65903686 Abstract: We assessed the sustainability of agricultural water resources in Hubei Province, a typical agricultural province in central China, for a decade (2008–2018). Since traditional evaluation models often consider only the distance between the evaluation point and the positive or negative ideal solution, we introduce gray correlation analysis and construct a new sustainability evaluation model. Our research results show that only one city had excellent sustainable development capacity of agricultural water resources, and the evaluation value of eight cities fluctuated by around 0.5 (the median of the evaluation result), while the sustainable development capacity of agricultural water resources in other cities was relatively poor. Our findings not only reflect the differences in the natural conditions of water resources among various cities in Hubei, but also the impact of the cities’ policies to ensure efficient agricultural water use for sustainable development. The indicators and methods Citation: Jin, H.; Huang, S. Are in this research are not difficult to obtain in most countries and regions of the world. Therefore, the China’s Water Resources for indicator system we have established by this research could be used to study the sustainability of Agriculture Sustainable? Evidence agricultural water resources in other countries, regions, or cities. from Hubei Province. Sustainability 2021, 13, 3510. https://doi.org/ Keywords: water resources; agricultural water resources; sustainability; gray correlation analysis; 10.3390/su13063510 evaluation model Academic Editors: Daniela Malcangio, Alan Cuthbertson, Juan 1.