Anal Cancer (Anus)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Park University Clery Annual Security Report
PA RK U N I V E R S I T Y CLERY ANNUAL SECURITY REPORT 2017 ARKANSAS • Little Rock AFB 2017 SPECIAL MESSAGE FROM PARK UNIVERSITY DIRECTOR OF CAMPUS SAFETY Each year, in compliance with the Jeanne Clery Disclosure of Campus Safety Policy and Campus Crime Statistics Act, Park University publishes the Park University Security and Fire Safety Report. This document, posted online at park.edu and distributed via hard copy upon request, provides local crime statistics, details the University’s regulations and procedures for emergency response, and lists on- and off- campus resources for safety assistance. Although all colleges and universities participating in federal financial aid programs are required to share this data with the public, we provide it with intention beyond simply obeying the rules and hope that doing so demonstrates Park’s commitment to the well-being of students, faculty and staff members, business tenants and visitors. The annual production of the Report is just one element of our larger, sustained strategy around security and safety. In 2017, we have taken measures to promote a safe and desirable college experience for all students, faculty and staff by implementing contingency plans for incidents such as active shooter and bomb threat through cooperative training with local police, fire and ambulance services. The Park University Department of Campus Safety is proud to help foster a safe University environment that is conducive to collaboration, development and growth for all who live, learn and work on Park’s campuses. Thank you for your interest in our processes and outcomes. Sincerely, Will London Director of Campus Safety, Park University [email protected] 1 Founded in 1875 in Parkville, Mo., a suburb of Kansas City, Park University has developed into a comprehensive, independent institution that is a national leader in higher education. -
2020 DEPARTMENT of PUBLIC SAFETY Annual Security Report
WEBSTER UNIVERSITY 2020 DEPARTMENT OF PUBLIC SAFETY Annual Security Report Little Rock Metro Campus QUICK REFERENCE RESOURCES Emergency Contacts Emergency 911 Little Rock Police Dept. (non-emergency) 501-371-4829 Webster University – Little Rock Metro 501-375-1511 Webster University Department of Public Safety 314-246-7430 (non-emergency) Sexual Offense Advocate (main campus) 314-649-8474 (24 hours a day) The Department of Public Safety and Sexual Offense Advocate are located on the main campus in Webster Groves, Missouri; however, staff members can assist callers remotely or make appropriate referrals to local resources. Webster Alert System This is the University’s free mass notification service which is used to alert all students, faculty & staff regarding important information regarding campus crimes, emergencies and other potentially life threatening events at their webster.edu email address. Users are strongly encouraged to add a personal email address and mobile number to their account by logging into Connections and clicking on the Webster Alerts banner. The following telephone numbers connect callers with personnel at the main campus; however, staff and administrators at the main campus can either assist callers at branch campuses remotely or make appropriate local referrals. University Title IX Coordinator University Title IX Coordinator 314-246-7780 Other Campus Resources Dean of Students Office 314-968-6980 Academic Resource Center 314-246-7620 Financial Aid Office 314-968-6992 Counseling Services 314-968-7030 Immigration/Visa Information 314-246-7860 Webster University 2020 Annual Security Report – LITTLE ROCK METRO 1 LITTLE ROCK METRO CAMPUS ANNUAL CRIME STATISTICS This section of the Annual Security Report explains what type of crimes institutions are directed to include under the Clery Act, as well as how the University obtains and tabulates these statistics each year. -

Proposed Amendment to Zoning Ordinance for Adult Oriented
Proposed Amendment to Zoning Ordinance Adult Oriented Business Authority and Jurisdiction The provisions of this article are adopted by the Town Board of Commissioners under the authority granted by the General Assembly of the State of North Carolina. From and after the effective date hereof, this article shall apply to every building, lot, tract, or parcel of land within the Town of Grifton and its extraterritorial jurisdiction. Purpose For the purpose of promoting the health, safety, morals and general welfare of the citizenry of the Town of Grifton, this article is adopted by the Board of Commissioners to regulate adult and sexually oriented businesses, as hereby defined, located in the Town of Grifton and its extraterritorial jurisdiction. Further the regulations of this article have been made with reasonable consideration among other things, as to the character of the town and its areas. Abrogation These regulations shall not repeal, impair, abrogate, or interfere with any existing easements, covenants, deed restrictions, setback requirements, rules, definitions, regulations previously adopted pursuant to law in any established zoning district in the Town of Grifton. However, where these regulations impose greater restrictions, the provisions of these regulations shall govern. Definitions Relating to Adult Oriented Businesses Adult Oriented Business. An adult arcade, adult bookstore, or adult video store, adult cabaret, adult motel, adult motion picture theater, adult theater, escort agency, nude model studio, sexual encounter center (including adult massage parlor and adult heath club), sexually oriented device business or any combination of the foregoing or any similar business. As used in this Ordinance the following definitions shall apply: Adult Arcade (also know as “peep show”). -

Ordinance Regulating Adult Establishments Sexually Oriented Businesses
PLANNING & DEVELOPMENT SERVICES ----------------------------------------- ORDINANCE NO. 2 ORDINANCE REGULATING ADULT ESTABLISHMENTS SEXUALLY ORIENTED BUSINESSES WHEREAS, the provisions of this Ordinance are adopted by the Pitt County Board of Commissioners under the authority granted by GS § 153A-(45-50); 153A-121; 153A-(134-135); and 160A-181.1;. and 160D-902. WHEREAS, the Board of Commissioners recognizes that important and substantial governmental inter- ests provide a constitutional basis for reasonable regulation of the time, place and manner under which adult and sexually oriented businesses operate; and WHEREAS, for the purpose of preventing harmful secondary impacts such as neighborhood blight, increases in crime and decreases in property value, this Ordinance is adopted by the Board of Commis- sioners to regulate adult and sexually oriented businesses, as hereby defined, located in the County. From and after the effective date of this Ordinance, this Ordinance shall apply to every building, lot, tract or parcel of land within unincorporated Pitt County, in all municipalities where the Pitt County Sheriff pro- vides law enforcement patrol, and in any incorporated municipality that by Resolution requests enforce- ment of this Ordinance within its jurisdiction; and WHEREAS, the Board of Commissioners has determined that persons seeking to operate sexually ori- ented businesses shall be required to observe specific location requirements before they commence business; and WHEREAS, the regulations contained in this Ordinance shall not repeal, impair, abrogate or interfere with any existing easements, covenants, deed restrictions, setback requirements, rules, definitions, or regula- tions previously adopted pursuant to law in any established zoning district in Pitt County. However, where these regulations impose greater restrictions, the provisions of these regulations shall govern. -

In the Beginning Was the Big Toe
In the Beginning was the Big Toe: Bataille, Base Materialism, Bipedalism Matthew Beaumont I In the beginning was the big toe. Or, to formulate it in terms of a base-materialist philosophy, being begins with the big toe. In an essay on the mouth from 1930, the renegade Surrealist philosopher Georges Bataille stated that “man does not have a simple architecture like beasts, and it is not even possible to say where he begins”.i As Roland Barthes understood, it is a statement of some philosophical importance. In “Outcomes of the Text”, Barthes noted that “Bataille raises the question of the beginning where it had never been raised: ‘Where does the human body begin?’”ii Bataille’s claim is that the mouth is the beginning, or “prow”, of animals. Implicitly, then, the anus, or perhaps the tail, is the end of animals. Bataille confronted this end, in the form of an ape’s protuberant anus, its “anal projection”, on a visit to London Zoo in July 1927 – an encounter that, because it seemed to him to violate the discreet seclusion of the human anus, proved at the same time horrific and epiphanic.iii Bataille insists that, in contrast to an ape’s body, a man or woman’s body does not have a beginning or an ending. Reading Bataille against Bataille, in this article I want to argue instead that, as a species, the human being begins with the big toe. In 1 1929, a year before he published his essay on the mouth, Bataille wrote an essay on the big toe in which he contended that, although the big toe is routinely regarded as base, it is paradoxically the most noble bit of the human body. -

The Veil of Forgetting
the veil of forgetting the veil of forgetting the peaks and potholes of 2016 formed into a fascicle by Don Shewey ACCENTS ACTIVISM ANTARCTICA ANUS ART AWE BAMBOO BLACK LIVES MATTER BOWS CANCER CHALLENGING CHARACTER CHUTE COMFORT COMPASSION CONCLUSIONS CONTAINMENT DIAGNOSIS EARTH ECLIPSE EGO ELDERS FORGIVENESS GARDEN GUNS HOME ICELAND IMAGINAL HYGIENE INITIATION INTEGRITY JAMES HOUGHTON JOKES KILLING LIFE LONELINESS LOVE MASK MASTURBATION MEMORY MINDSET NAKED NUMBING OLD PARANOIA PARENTING PASSION PHILANTHROPY PLEASURE PMS POLITICAL EFFECTIVENESS POWER PROFESSIONALISM PSYCHEDELICS QUEEN OF SOUL QUEER QUESTIONS REGRET REJECTION REPETITION SAUDI ARABIA SCIENCE SEX SHAMANISM SHAME SNEEZING SONGWRITING SPEAK STRESS SUFFERING SUPEREGO TEA PARTY THEATER TIME TRAVEL TRUMP TIME UGLY TRUTHS VALUES VIRTUES VISION VOTING WEIRD WORRY WRITING WYOMING XXX YEAR IN REVIEW ZEITGEIST ACCENTS I hear you’re a new father to a baby boy. Congratulations. What’s his name? Hudson. I guess you can see the river from your office. It was either Hudson or Window. It didn’t occur to me until recently actually that my son is going to have an American accent. Because I guess in my head that’s never how I’ve heard my child speak, and I think it’ll be odd that I’m going to sound different from him. And he’ll hear me have to change my voice for automated machines. You probably don’t have to do that. On the automated phone lines, all the time — “No. 4.” “I’m sorry, I didn’t understand that.” “No. 4.” “I don’t understand that,” and I have to say “No. 4” like a kind of a sedated John Wayne. -

Anatomy & Biology Catalogue
Anatomy & Biology R4Q100W41102015 Catalogue Altay Scientific Group Headquarters: Via Maremmana III, 7b 00030 San Cesareo (Rome) Italy Phone: + 39 06 94 55 01 Fax: + 39 06 94 55 00 15 [email protected] www.altayscientific.com Crafted for your world. Altay is committed to making our world a better place to live. About Altay Started as a family business more than 60 years ago, Altay has grown into a 21st century, international company with operations on 5 continents employing more than 500 people. But family traditions and values are still the basis of our work. We are ready to meet today’s market demands with the passion and dedication of the past, together with the technology and tools of tomorrow. Do you now that while buying Altay’s Altay Vision products you are selecting: Altay Scientific is a leading company in the global market for science education sold through a worldwide network of authorized dealer f HIGH QUALITY partners. © iStockphoto.com/smokingdrum Altay produces a full line of innovative and user friendly products based Altay’s anatomical models are made durable polyvinyl resin and upon the highest technology research and development married to hands painted by skilled craftsmen. This ensures durability as high quality, low cost production techniques and processes. The Altay brand stands for innovation, value and customer orientation. well as natural look. The global Altay organization remains committed to investing the f SCIENTIFIC PERFECTION necessary human and financial capital in the Altay Vision. Altay Mission f THREE YEAR GUARANTEE ON ALL ALTAY PRODUCTS The search for knowledge is a need that comes from human nature. -
Pleading Wizard
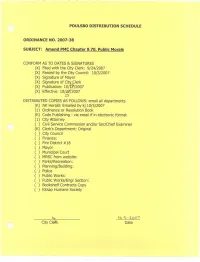
ORDINANCE NO. 2007-38 AN ORDINANCE OF THE CITY OF POULSBO, WASHINGTON, RELATING TO PUBLIC MORALS; AMENDING CHAPTER 9.70 TO BE KNOWN AS PUBIC MORALS, CRIMES RELATING TO; AND ADOPTING BY REFERENCE VARIOUS SECTIONS OF TITLES 9 AND 9A OF THE REVISED CODE OF WASHINGTON IN ORDER TO ESTABLISH CRIMES DESIGNATED BY THE STATE AS MISDEMEANORS AND GROSS MISDEMEANORS AS CRIMINAL OFFENSES UNDER THE CITY’S MUNICIPAL CODE; PROVIDING FOR SEVERABILITY AND ESTABLISHING AN EFFECTIVE DATE. WHEREAS, the City Council of the City of Poulsbo is concerned about the safety and welfare of its citizens and roadways; Now, Therefore, THE CITY COUNCIL OF THE CITY OF POULSBO DO ORDAIN AS FOLLOWS: Section 1. Chapter 9.70 of the Poulsbo Municipal Code is hereby amended to read as follows: 9.70 PUBLIC MORALS, CRIMES RELATING TO. Section 2. PMC 9.70.010 and Ordinance 97-33 Section 1 are hereby amended to read as follows: 9.70.010 Obscenity and pornography - statutes adopted by reference Pursuant to the authority contained in RCW 35A.12.140 the following sections of Chapter 9.68, RCW as enacted or hereinafter amended are hereby adopted by reference as if fully set forth herein including penalties. RCW 9.68.015 Obscene literature, shows, etc. – exemptions 9.68.030 Indecent articles, etc. 9.68.050 “Erotic material” – definitions 9.68.060 “Erotic material” – determination by court – labeling – penalties 9.68.070 Prosecution for violation of RCW 9.68.060 – defense 9.68.080 Unlawful acts 9.68.090 Civil liability of wholesaler or wholesaler-distributor 9.68.100 Exception to RCW 9.68.050 through 9.68.120 9.68.110 Motion picture operator or projectionist exempt, when 9.68.120 Provision of RCW 9.68.050 through 9.68.120 exclusive 9.68.130 “Sexually explicit material” – defined – unlawful display Section 3. -

I Syn-Theses, Or, the Mechanics of Oppression in Western Literary
i Syn-theses, or, The Mechanics of Oppression in Western Literary Criticism A Thesis by THOMAS ALBERT YOUNG Submitted to the School of Graduate Studies at Appalachian State University in partial fulfillment of the requirements for the degree of Master of Arts May, 2020 Department of English ii Syn-theses, or, The Mechanics of Oppression in Western Literary Criticism A Thesis by THOMAS ALBERT YOUNG May 2020 APPROVED BY: ______________________________ Carl Eby, Ph.D. Chairperson, Thesis Committee _______________________________ Kathryn Kirkpatrick, Ph.D. Member, Thesis Committee _______________________________ Joseph Bathanti Member, Thesis Committee _______________________________ Leo Flores, Ph.D. Chairperson, Department of English _______________________________ Mike McKenzie, Ph.D. Dean, Cratis D. Williams School of Graduate Studies iii Copyright by Thomas Albert Young, 2020 All Rights Reserved iv Abstract Syn-theses, or, The Mechanics of Oppression in Western Literary Criticism Thomas Albert Young B.A. Appalachian State University M.A. Appalachian State University Chairperson: Carl Eby, Ph.D. The intent of my life is to ensure that all we do, beyond personal enrichment, is oriented at the betterment of all people, or the widest array of population possible. As a result, this project endeavours towards rectification. At its heart, it endeavors to redress various forms of oppression-- racism, misogyny, and queerphobia--that pervade and frustrate the goals of Literary Criticism, literature, and literary studies. And, by force, as students, we are required to cite and reference back towards historical socialism. Yet, what if you are queer and the texts you must reckon with are homophobic? Should you be expected to accommodate, and then suggest why the text is homophobic? In that sense, your work is then to explain and defend your own existence and its validity. -

Offenses and Penalties
TITLE 26 OFFENSES AND PENALTIES CHAPTER 26.01 General Purposes 26.0101 The general purposes. The general purposes of this Title are to establish a system of prohibitions, penalties, and correctional measures to deal with conduct that unjustifiably and inexcusably causes or threatens harm to an individual or public interests for which tribal protection is appropriate. To this end, the provisions of this Title are intended, and shall be construed, to achieve the following objectives: 1. To ensure the public safety through: a. vindication of public norms by the imposition of merited punishment; b. the deterrent influence of the penalties hereinafter provided; c. the rehabilitation of those convicted of violations of this title; and d. such confinement as may be necessary to prevent likely recurrence of serious criminal behavior. 2. By definition and grading of offenses, to define the limits and systematize the exercise of discretion in punishment and to give fair warning of what is prohibited and of the consequences of violation. 3. To prescribe penalties which are proportionate to the seriousness of offenses and which permit recognition of differences in rehabilitation possibilities among individual offenders. 4. To safeguard conduct that is without guilt from condemnation as criminal and to condemn conduct that is with guilt as criminal. 5. To prevent arbitrary or oppressive treatment of persons accused or convicted of offenses. ADOPTED TMBC5619-04-94 AMENDED REMOVED PARAGRAPH 6 BY RESOLUTION TMBC1246-06-18. CHAPTER 26.02 Proof and Presumptions 26.0201 An accused is presumed innocent until proven guilty. 1. No person may be convicted of an offense unless each element of the offense is proved beyond a reasonable doubt. -

Liver, Pancreas and Duodenum Stomach and Associated Organs Of
K127 Liver, Pancreas and Duodenum This life size model, 2-part model, shows the liver with gallbladder, pancreas and K128 K122 partly dissected duodenum. It includes inferior vena cava, abdominal aorta and Pancreas, duodenum and pancreatic ducts. Mounted on stand. Stomach and Associated spleen Size: 12 x 12 x 31 cm Organs of the Upper Abdomen This life size model is an accurate repre- Weight: 0.7 kg This life size model has the following sentation of the pancreas, spleen and Ref.no. K127 features, 2-part stomach along with the duodenum. The pancreas is open to show pancreas, spleen and duodenum (shown in the entire pancreatic duct. The duodenum open section), gallbladder with bile ducts, is partially dissected to expose its internal abdominal aorta, vena cava, mesenteric and structure. Mounted on stand. iliac vessels. 2 sections of the liver-gallblad- Size: 16 x 15 x 23 cm der are interchangeable. Mounted on stand. Weight: approx. 0.4 kg Size: 20 x 16 x 31 cm, Weight: 1 kg Ref.no. K122 Ref.no.no. K128 New Diseases of Pancreas, Spleen, Gall bladder This full size model shows pancreatic cancer, the gallbladder with stones, a rup- tured spleen and duodenum with an ulcer. Ref.no. K295 K123 W42509 Gallbladder, Pancreas and Duodenum, Diseases Internal Organs, 2-part This life size model is a representation of The organs are shown partially opened, the most important diseases of the and the gall bladder is removable with part gallbladder, pancreas and duodenum. The of the liver. gallbladder, partially opened, shows the It depicts: stones located in various locations, • Pancreas K151 cholecystitis, polyposis and carcinoma. -

An Ordinance Amending the Greensboro Code of Ordinances with Respect to Zoning, Planning and Development
ATTACHMENT “A” (Revised 11/20/13) AMENDING CHAPTER 30 (LDO) AN ORDINANCE AMENDING THE GREENSBORO CODE OF ORDINANCES WITH RESPECT TO ZONING, PLANNING AND DEVELOPMENT (Editor’s Note: Added text shown with underlines and deleted text shown with strikethroughs) Section 1. That Table 8-1 within Section 30-8-1, Permitted Use Table, is hereby amended by deleting “Central Business (CB)” as a zoning district where Sexually Oriented Businesses are allowed. Section 2. That Subsection (N) of Section 30-8-10.4, Office, Retail and Commercial Uses, is hereby amended to read as follows: (N) Sexually Oriented Businesses 1) Use Description Sexually Oriented Businesses include: sex shops, adult arcades, adult sexually oriented media book stores or adult video stores, adult cabarets sexually oriented cabarets, adult massage parlors, adult motels, adult motion picture theater sexually oriented motion picture theaters, adult theaters, escort agencies, nude model studios, sexual encounter centers, or any combination of these uses. All sexually oriented business uses are considered principal uses. 2) Property Separation a) No sexually oriented business is permitted to be located within 1,200 feet of any other sexually oriented business b) No sexually oriented business is permitted to be located within 1,000 feet of a religious assembly use, public or private elementary or secondary school, child day care center or nursery school, public park, or residentially zoned property 3) Prohibition in Historic District Overlay No sexually oriented business is permitted to locate in the Old Greensborough National Register Historic District. 4) Prohibition of Sleeping Quarters Except for an adult motel, a No sexually oriented business is permitted to have sleeping quarters.