Mitochondrial Mutations and Genetic Factors Determining NAFLD Risk
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Mitochondrial DNA Mutations Cause Various Diseases
2013 Neurobiology of Disease in Children Symposium: Mitochondrial Disease, October 30, 2013 Defects of Mitochondrial DNA Replication William C. Copeland Laboratory of Molecular Genetics Mitochondrial DNA mutations cause various diseases * Alpers Disease * Leigh Disease or Syndrome * Barth syndrome * LHON * Beta-oxidation Defects * LIC (Lethal Infantile Cardiomyopathy) * Carnitine-Acyl-Carnitine * Luft Disease Deficiency * MAD * Carnitine Deficiency * MCAD * Co-Enzyme Q10 Deficiency * MELAS * Complex I Deficiency * MERRF * Complex II Deficiency * Mitochondrial Cytopathy * Complex III Deficiency * Mitochondrial DNA Depletion * Complex IV Deficiency * Mitochondrial Encephalopathy * Complex V Deficiency * Mitochondrial Myopathy * COX Deficiency * MNGIE * CPEO * NARP * CPT I Deficiency * Pearson Syndrome * CPT II Deficiency * Pyruvate Carboxylase Deficiency * Glutaric Aciduria Type II * Pyruvate Dehydrogenase Deficiency * KSS * Respiratory Chain * Lactic Acidosis * SCAD * LCAD * SCHAD * LCHAD * VLCAD Origins of mtDNA mutations Damage to DNA •Environmental factors •Endogenous oxidative stress Spontaneous errors •DNA replication •Translesion synthesis •DNA repair re-synthesis Mitochondrial DNA replication p32 - RNaseH 16 Human DNA Polymerases Polymerase Family Chromosome Mol. Wt. (kDa) Function/Comments α (alpha) B Xq21.3-q22.1 165 Initiates replication β (beta) X 8p12-p11 39 BER, other functions γ (gamma) A 15q25 140 Mitochondrial replication & repair δ (delta) B 19q13.3-.4 125 Replication, BER, NER, MMR ε (epsilon) B 12q24.3 255 Replication, checkpoint -

The Mtdna Replication-Related Genes TFAM and POLG Are Associated with Leprosy in Han Chinese from Southwest China Journal of De
Journal of Dermatological Science 88 (2017) 349–356 Contents lists available at ScienceDirect Journal of Dermatological Science journa l homepage: www.jdsjournal.com The mtDNA replication-related genes TFAM and POLG are associated with leprosy in Han Chinese from Southwest China a a,d a a a b Dong Wang , Guo-Dong Li , Yu Fan , Deng-Feng Zhang , Rui Bi , Xiu-Feng Yu , b c a,d, Heng Long , Yu-Ye Li , Yong-Gang Yao * a Key Laboratory of Animal Models and Human Disease Mechanisms of the Chinese Academy of Sciences & Yunnan Province, Kunming Institute of Zoology, Kunming, Yunnan, 650223, China b Wenshan Institute of Dermatology, Wenshan, Yunnan, 663000, China c Department of Dermatology, The First Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, 650032, China d Kunming College of Life Science, University of Chinese Academy of Sciences, Kunming, Yunnan 650201, China A R T I C L E I N F O A B S T R A C T Article history: Background: The pathogen Mycobacterium leprae of leprosy is heavily dependent on the host energy Received 2 June 2017 metabolites and nutritional products for survival. Previously we and others have identified associations Received in revised form 7 September 2017 of several mitochondrion-related genes and mitochondrial DNA (mtDNA) copy number alterations with Accepted 13 September 2017 leprosy and/or its subtype. We hypothesized that genetic variants of mtDNA replication-related genes would affect leprosy. Keywords: Objective: We aimed to identify genetic associations between the mtDNA replication-related genes TFAM, Leprosy POLG and leprosy. TFAM Methods: Genetic association study was performed in 2898 individuals from two independent sample POLG fi eQTL sets in Yunnan Province, China. -

Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

The Role of Mitochondrial DNA Mutations in Mammalian Aging Gregory C
Review The Role of Mitochondrial DNA Mutations in Mammalian Aging Gregory C. Kujoth, Patrick C. Bradshaw, Suraiya Haroon, Tomas A. Prolla* ABSTRACT humans is likely to carry these disease-associated mutations. Thus, it is unlikely that these mutations have deleterious itochondrial DNA (mtDNA) accumulates both consequences in normal aging. Studies performed in the base-substitution mutations and deletions with Attardi laboratory have established that some specific base- M aging in several tissues in mammals. Here, we substitution mutations can reach high levels in fibroblast cells examine the evidence supporting a causative role for mtDNA derived from aged individuals [2] and also in skeletal muscle mutations in mammalian aging. We describe and compare [3]. The reason why these specific mutations accumulate in human diseases and mouse models associated with mtDNA is unclear, but they are tissue-specific and occur in mitochondrial genome instability. We also discuss potential mtDNA control sites for replication. Interestingly, the same mechanisms for the generation of these mutations and the group has found a C150T transition mutation that occurs in means by which they may mediate their pathological most or all mtDNA molecules (i.e., a homoplasmic mutation) consequences. Strategies for slowing the accumulation and is present in leukocytes from approximately 17% of attenuating the effects of mtDNA mutations are discussed. individuals aged 99–106 years old. This mutation is associated with a new replication origin position, suggesting that it may Introduction confer a survival advantage in humans [4]. With the development of high-throughput sequencing The mitochondrial theory of aging is based on the premise methods, an unbiased large-scale examination of either that reactive oxygen species (ROS), generated throughout the selected regions or the entire mtDNA sequence has become lifespan of an organism, damage mitochondrial feasible. -

EGL Test Description
2460 Mountain Industrial Boulevard | Tucker, Georgia 30084 Phone: 470-378-2200 or 855-831-7447 | Fax: 470-378-2250 eglgenetics.com Inherited Metabolic Disorders Panel: Sequencing and CNV Analysis Test Code: MM310 Turnaround time: 6 weeks CPT Codes: 81404 x1, 81406 x1, 81405 x1 Condition Description Inherited metabolic disorders refer to diseases caused by defects in genes that are involved in the body’s metabolism. These usually involve the production, conversion, or use of energy. Traditionally, inherited metabolic conditions were broadly classified as disorders of carbohydrate metabolism, amino acid metabolism, organic acid metabolism, or lysosomal storage diseases. This test analyses genes involved in complex metabolic processes in the body including but not limited to the above four categories. Reference: OMIM. Genes ACAD9, ACADL, ACADM, ACADS, ACADVL, ACSF3, AGA, AGL, ALDH5A1, ARSA, ASL, ASS1, ATPAF2, AUH, BCKDHA, BCKDHB, CD320, CLN3, CLN5, CLN6, CLN8, CPS1, CPT1A, CPT2, CYP27A1, DBT, DLD, ENO3, ETFA, ETFB, ETFDH, G6PC, GAA, GALC, GALNS, GBA, GBE1, GLA, GLB1, GM2A, GNPTAB, GYS1, GYS2, HADHA, HADHB, HGSNAT, HMGCL, HMGCS2, HYAL1, IDS, IDUA, IVD, LIPA, LMBRD1, LPIN1, MAN2B1, MANBA, MCCC1, MCCC2, MCEE, MCOLN1, MFSD8, MLYCD, MMAA, MMAB, MMACHC, MMADHC, MMUT, MTR, MTRR, NAGA, NAGLU, NAGS, NEU1, NPC1, NPC2, OPA3, OTC, PC, PCCA, PCCB, PFKM, POLG, PPT1, PYGL, PYGM, SERAC1, SGSH, SLC17A5, SLC22A5, SLC25A13, SLC25A15, SLC25A20, SLC37A4, SLC7A7, SMPD1, SUCLG1, SUMF1, TAZ, TMEM70, TPP1 Indications This test is indicated for: Confirmation of a clinical diagnosis of inherited metabolic disorders. Methodology Next Generation Sequencing: In-solution hybridization of all coding exons is performed on the patient's genomic DNA. Although some deep intronic regions may also be analyzed, this assay is not meant to interrogate most promoter regions, deep intronic regions, or other regulatory elements, and does not detect single or multi-exon deletions or duplications. -

Mechanisms of Mitochondrial DNA Deletion Formation Nadee Nissanka1, Michal Minczuk2, and Carlos T. Moraes1 1Department of Neurol
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Apollo Mechanisms of Mitochondrial DNA Deletion Formation Nadee Nissanka1, Michal Minczuk2, and Carlos T. Moraes1 1Department of Neurology, University of Miami Miller School of Medicine 33136, USA; 2Medical Research Council (MRC) Mitochondrial Biology Unit, University of Cambridge, Cambridge, UK; To whom correspondence should be addressed: Carlos T. Moraes, 1420 NW 9th Avenue, Rm.229, Miami, FL 33136; Tel: 305-243- 5858; Fax: 305-243-6955; Email: [email protected] Keywords: mitochondrial DNA, double-strand breaks, mitochondrial DNA deletions, replication Abstract Mitochondrial DNA (mtDNA) encodes a subset of genes which are essential for oxidative phosphorylation. Deletions in the mtDNA can ablate a number of these genes, and result in mitochondrial dysfunction which is associated with bona-fide mitochondrial disorders. Although mtDNA deletions are thought to occur as a result of replication errors or following double-strand breaks, the exact mechanism(s) behind deletion formation have yet to be determined. In this review we discuss the current knowledge about the fate of mtDNA following double-strand breaks, including the molecular players which mediate the degradation of linear mtDNA fragments, and possible mechanisms of re- circularization. We propose that mtDNA deletions formed from replication errors versus following double-strand breaks can be mediated by separate pathways. Mitochondrial DNA The human mitochondrial DNA (mtDNA) is a 16,569 bp circular, double-stranded, supercoiled molecule which was first discovered in 1963 [1]. The mtDNA molecule encodes 37 different genes which are essential for oxidative phosphorylation (OXPHOS) and mitochondrial protein synthesis [2]. -

New Mesh Headings for 2018 Single Column After Cutover
New MeSH Headings for 2018 Listed in alphabetical order with Heading, Scope Note, Annotation (AN), and Tree Locations 2-Hydroxypropyl-beta-cyclodextrin Derivative of beta-cyclodextrin that is used as an excipient for steroid drugs and as a lipid chelator. Tree locations: beta-Cyclodextrins D04.345.103.333.500 D09.301.915.400.375.333.500 D09.698.365.855.400.375.333.500 AAA Domain An approximately 250 amino acid domain common to AAA ATPases and AAA Proteins. It consists of a highly conserved N-terminal P-Loop ATPase subdomain with an alpha-beta-alpha conformation, and a less-conserved C- terminal subdomain with an all alpha conformation. The N-terminal subdomain includes Walker A and Walker B motifs which function in ATP binding and hydrolysis. Tree locations: Amino Acid Motifs G02.111.570.820.709.275.500.913 AAA Proteins A large, highly conserved and functionally diverse superfamily of NTPases and nucleotide-binding proteins that are characterized by a conserved 200 to 250 amino acid nucleotide-binding and catalytic domain, the AAA+ module. They assemble into hexameric ring complexes that function in the energy-dependent remodeling of macromolecules. Members include ATPASES ASSOCIATED WITH DIVERSE CELLULAR ACTIVITIES. Tree locations: Acid Anhydride Hydrolases D08.811.277.040.013 Carrier Proteins D12.776.157.025 Abuse-Deterrent Formulations Drug formulations or delivery systems intended to discourage the abuse of CONTROLLED SUBSTANCES. These may include physical barriers to prevent chewing or crushing the drug; chemical barriers that prevent extraction of psychoactive ingredients; agonist-antagonist combinations to reduce euphoria associated with abuse; aversion, where controlled substances are combined with others that will produce an unpleasant effect if the patient manipulates the dosage form or exceeds the recommended dose; delivery systems that are resistant to abuse such as implants; or combinations of these methods. -

Human Mitochondrial RNA Polymerase Primes Lagging-Strand DNA Synthesis in Vitro
Human mitochondrial RNA polymerase primes lagging-strand DNA synthesis in vitro Sjoerd Wanrooij*†, Javier Miralles Fuste´ *, Ge´ raldine Farge*, Yonghong Shi*†, Claes M. Gustafsson*†‡, and Maria Falkenberg*†‡ *Division of Metabolic Diseases, Karolinska Institutet, Novum, SE-141 86 Stockholm, Sweden; and †Department of Medical Biochemistry and Cell Biology, Go¨teborg University, Box 440, SE-405 30 Go¨teborg, Sweden Communicated by I. Robert Lehman, Stanford University School of Medicine, Stanford, CA, June 4, 2008 (received for review March 14, 2008) The mitochondrial transcription machinery synthesizes the RNA strand promoters (LSP) generates transcripts of almost genomic primers required for initiation of leading-strand DNA synthesis in length, which are processed to yield the individual mRNA and mammalian mitochondria. RNA primers are also required for ini- tRNA molecules (10, 11). LSP-dependent transcription also tiation of lagging-strand DNA synthesis, but the responsible en- generates the primers needed at OH (12), and RNA attached to zyme has so far remained elusive. Here, we present a series of the newly synthesized H strand has been detected in both mouse observations that suggests that mitochondrial RNA polymerase and human cells (13). Primer formation may include an RNase (POLRMT) can act as lagging-strand primase in mammalian cells. MRP-dependent cleavage of the transcribed L-strand RNA at POLRMT is highly processive on double-stranded DNA, but synthe- the initiation sites of DNA replication (14). Alternatively, spe- sizes RNA primers with a length of 25 to 75 nt on a single-stranded cific mtDNA sequences may direct premature transcription template. The short RNA primers synthesized by POLRMT are used termination and primer formation near OH (15). -
Polymerase Gamma (POLG) Related Disorders Genetic Testing
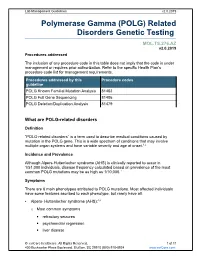
Lab Management Guidelines v2.0.2019 Polymerase Gamma (POLG) Related Disorders Genetic Testing MOL.TS.276.AZ v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline POLG Known Familial Mutation Analysis 81403 POLG Full Gene Sequencing 81406 POLG Deletion/Duplication Analysis 81479 What are POLG-related disorders Definition “POLG-related disorders” is a term used to describe medical conditions caused by mutation in the POLG gene. This is a wide spectrum of conditions that may involve multiple organ systems and have variable severity and age at onset.1,2 Incidence and Prevalence Although Alpers-Huttenlocher syndrome (AHS) is clinically reported to occur in 1/51,000 individuals, disease frequency calculated based on prevalence of the most common POLG mutations may be as high as 1/10,000.1 Symptoms There are 6 main phenotypes attributed to POLG mutations. Most affected individuals have some features ascribed to each phenotype, but rarely have all. Alpers- Huttenlocher syndrome (AHS):3,4 o Most common symptoms . refractory seizures . psychomotor regression . liver disease © eviCore healthcare. All Rights Reserved. 1 of 11 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines v2.0.2019 o Orther possible symptoms . migraine with visual auras . cortical blindness . hypotonia . ataxia . extrapyramidal movements . peripheral neuropathy . progressive spastic paraparesis . renal tubular acidosis . hearing loss . cyclic vomiting . pancreatitis o Development is often normal until disease onset, which is typically before 4 years of age. -

Spatial Sorting Enables Comprehensive Characterization of Liver Zonation
ARTICLES https://doi.org/10.1038/s42255-019-0109-9 Spatial sorting enables comprehensive characterization of liver zonation Shani Ben-Moshe1,3, Yonatan Shapira1,3, Andreas E. Moor 1,2, Rita Manco1, Tamar Veg1, Keren Bahar Halpern1 and Shalev Itzkovitz 1* The mammalian liver is composed of repeating hexagonal units termed lobules. Spatially resolved single-cell transcriptomics has revealed that about half of hepatocyte genes are differentially expressed across the lobule, yet technical limitations have impeded reconstructing similar global spatial maps of other hepatocyte features. Here, we show how zonated surface markers can be used to sort hepatocytes from defined lobule zones with high spatial resolution. We apply transcriptomics, microRNA (miRNA) array measurements and mass spectrometry proteomics to reconstruct spatial atlases of multiple zon- ated features. We demonstrate that protein zonation largely overlaps with messenger RNA zonation, with the periportal HNF4α as an exception. We identify zonation of miRNAs, such as miR-122, and inverse zonation of miRNAs and their hepa- tocyte target genes, highlighting potential regulation of gene expression levels through zonated mRNA degradation. Among the targets, we find the pericentral Wingless-related integration site (Wnt) receptors Fzd7 and Fzd8 and the periportal Wnt inhibitors Tcf7l1 and Ctnnbip1. Our approach facilitates reconstructing spatial atlases of multiple cellular features in the liver and other structured tissues. he mammalian liver is a structured organ, consisting of measurements would broaden our understanding of the regulation repeating hexagonally shaped units termed ‘lobules’ (Fig. 1a). of liver zonation and could be used to model liver metabolic func- In mice, each lobule consists of around 9–12 concentric lay- tion more precisely. -

Gene Expression Profiling of Differentiated Thyroid Neoplasms: Diagnostic and Clinical Implications
6586 Vol. 10, 6586–6597, October 1, 2004 Clinical Cancer Research Gene Expression Profiling of Differentiated Thyroid Neoplasms: Diagnostic and Clinical Implications Sylvie Chevillard,1 Nicolas Ugolin,1 entiation, adhesion, immune response, and proliferation as- Philippe Vielh,2 Katherine Ory,1 Ce´line Levalois,1 sociated pathways. Quantitative real-time reverse transcrip- Danielle Elliott,4 Gary L. Clayman,3 and tion-PCR analysis of selected genes corroborated the 4 microarray expression results. Adel K. El-Naggar Conclusions: Our study show the following: (1) differ- 1 Laboratoire de Cance´rologie Expe´rimentale, Commissariat a´ ences in gene expression between tumor and nontumor bear- L’Energie Atomique, Direction des Sciences du Vivant, De´partement ing normal thyroid tissue can be identified, (2) a set of genes du Radiobiologie et Radiopathologie, Fontenay-aux-Roses Cedex France; 2De´partement de Pathologie, Institut Gustave Roussy, differentiate follicular neoplasm from follicular variant of Villejuif Cedex, France; Departments of 3Head and Neck Surgery and papillary carcinoma, (3) follicular adenoma and carcinoma 4Pathology, The University of Texas M.D. Anderson Cancer Center, share many of the differentiated genes, and (4) gene expres- Houston, Texas sion differences identify conventional papillary carcinoma from the follicular variant. ABSTRACT Purpose: The purpose of this research was to identify INTRODUCTION novel genes that can be targeted as diagnostic and clinical Differentiated thyroid epithelial tumors represent a spec- markers of differentiated thyroid tumors. trum of morphologically and biologically diverse lesions. The Experimental Design: Gene expression analysis using follicular-derived neoplasms (adenoma, carcinoma, and the fol- microarray platform was performed on 6 pathologically licular variant of papillary carcinoma) manifest overlapping normal thyroid samples and 12 primary follicular and pap- cytomorphologic features and not infrequently pose diagnostic illary thyroid neoplasms.