Alcoholic Ketoacidosis L C Mcguire, a M Cruickshank, P T Munro
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alcohol Intoxication Withdrawal Adult
Provincial Clinical Knowledge Topic Alcohol Intoxication Withdrawal, Adult Emergency Department V 1.5 © 2018, Alberta Health Services. This work is licensed under the Creative Commons Attribution-Non-Commercial-No Derivatives 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/. Disclaimer: This material is intended for use by clinicians only and is provided on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness for a particular purpose of such information. This material is not a substitute for the advice of a qualified health professional. Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions, demands or suits arising from such use. Document History Version Date Description of Revision Completed By / Revised By 1.1 July 2015 Completed document (2013) reformatted into Dr. Bullard / Carla new topic template Milligan 1.2 January Minor edits in the Rationale section and form 1 Dr. Bullard / Sarah 2016 info in general care section as well as addition Searle of CIWA-Ar Scoring Reference tool to appendix 1.3 May 2016 Minor edits made to working group Sarah Searle membership list 1.4 June Removed link to Center for Addiction and Dr. Bullard / Sarah 2017 Mental Health assessment and documentation Searle form on pg. 35. Documentation requirements will continue as per local practice at this time. -

Diabetic Ketoacidosis and Hyperosmolar BMJ: First Published As 10.1136/Bmj.L1114 on 29 May 2019
STATE OF THE ART REVIEW Diabetic ketoacidosis and hyperosmolar BMJ: first published as 10.1136/bmj.l1114 on 29 May 2019. Downloaded from hyperglycemic syndrome: review of acute decompensated diabetes in adult patients Esra Karslioglu French,1 Amy C Donihi,2 Mary T Korytkowski1 1Division of Endocrinology and Metabolism, Department of ABSTRACT Medicine, University of Pittsburgh, Pittsburgh, PA, USA Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome (HHS) are life threatening 2University of Pittsburgh School of complications that occur in patients with diabetes. In addition to timely identification of the Pharmacy, Pittsburgh, PA, USA Correspondence to: M Korytkowski precipitating cause, the first step in acute management of these disorders includes aggressive [email protected] administration of intravenous fluids with appropriate replacement of electrolytes (primarily Cite this as: BMJ 2019;365:l1114 doi: 10.1136/bmj.l1114 potassium). In patients with diabetic ketoacidosis, this is always followed by administration Series explanation: State of the of insulin, usually via an intravenous insulin infusion that is continued until resolution of Art Reviews are commissioned on the basis of their relevance to ketonemia, but potentially via the subcutaneous route in mild cases. Careful monitoring academics and specialists in the US and internationally. For this reason by experienced physicians is needed during treatment for diabetic ketoacidosis and HHS. they are written predominantly by Common pitfalls in management include premature termination of intravenous insulin US authors therapy and insufficient timing or dosing of subcutaneous insulin before discontinuation of intravenous insulin. This review covers recommendations for acute management of diabetic ketoacidosis and HHS, the complications associated with these disorders, and methods for http://www.bmj.com/ preventing recurrence. -

Persistent Lactic Acidosis - Think Beyond Sepsis Emily Pallister1* and Thogulava Kannan2
ISSN: 2377-4630 Pallister and Kannan. Int J Anesthetic Anesthesiol 2019, 6:094 DOI: 10.23937/2377-4630/1410094 Volume 6 | Issue 3 International Journal of Open Access Anesthetics and Anesthesiology CASE REPORT Persistent Lactic Acidosis - Think beyond Sepsis Emily Pallister1* and Thogulava Kannan2 1 Check for ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, UK updates 2Consultant Anaesthetist, George Eliot Hospital, Nuneaton, UK *Corresponding author: Emily Pallister, ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, Coventry, UK Introduction • Differential diagnoses for hyperlactatemia beyond sepsis. A 79-year-old patient with type 2 diabetes mellitus was admitted to the Intensive Care Unit for manage- • Remember to check ketones in patients taking ment of Acute Kidney Injury refractory to fluid resusci- Metformin who present with renal impairment. tation. She had felt unwell for three days with poor oral • Recovery can be protracted despite haemofiltration. intake. Admission bloods showed severe lactic acidosis and Acute Kidney Injury (AKI). • Suspect digoxin toxicity in patients on warfarin with acute kidney injury, who develop cardiac manifes- The patient was initially managed with fluid resus- tations. citation in A&E, but there was no improvement in her acid/base balance or AKI. The Intensive Care team were Case Description asked to review the patient and she was subsequently The patient presented to the Emergency Depart- admitted to ICU for planned haemofiltration. ment with a 3 day history of feeling unwell with poor This case presented multiple complex concurrent oral intake. On examination, her heart rate was 48 with issues. Despite haemofiltration, acidosis persisted for blood pressure 139/32. -

The Effects of Ethanol on Ketone Body Metabolism of Fasted Rats Henry S
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1975 The effects of ethanol on ketone body metabolism of fasted rats Henry S. Cabin Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Cabin, Henry S., "The effects of ethanol on ketone body metabolism of fasted rats" (1975). Yale Medicine Thesis Digital Library. 2432. http://elischolar.library.yale.edu/ymtdl/2432 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. YALE MEDICAL LIBRARY YALE MEDICAL LIBRARY Digitized by the Internet Archive in 2017 with funding from The National Endowment for the Humanities and the Arcadia Fund https://archive.org/details/effectsofethanolOOcabi The Effects of Ethanol on Ketone Body Metabolism of Fasted Rats by Henry S, Cabin B.A. University of Pennsylvania, 1971 Presented in partial fulfillment of the requirements for the degree of Doctor of Medicine, Yale University School of Medicine -March, 1975- ACKNOWLEDGEMENTS To Dr. Felig- who.has guided me through this research project from its inception, and for whom I have the highest esteem as a teacher, physician and human being. To Rosa, Bill and Andrea- without whose support and assistance this project would never have come to fruition. -

Alcoholic Ketoacidosis
Alcoholic Ketoacidosis: Mind The Gap, Give Them What They Need Brendan Innes BS, Stephanie Carreiro MD University of Massachusetts Medical School, Department of Emergency Medicine Introduction Differential Diagnosis Case Discussion Pancreatitis, Alcohol induced gastritis, Alcohol withdrawal, Diagnostic Criteria for Alcoholic Ketoacidosis2,3 • Patients with alcohol use disorder commonly present to the ED Alcohol induced hepatitis, Acute Kidney Injury, Sepsis, Binge drinking ending in nausea, vomiting, and decreased intake critically ill due to a myriad of underlying pathologies. Metabolic abnormality (Alcoholic ketoacidosis), Acute coronary syndrome, Pulmonary embolism Wide anion gap metabolic acidosis without alternate explanation • Alcoholic ketoacidosis (AKA) should be considered in anyone Clinical Data Positive serum/urine ketones with prolonged and/or binge consumption of alcohol. Low, normal, or slightly elevated serum glucose Anion Gap 36 130 83 27 Urinalysis Core Emergency Medicine Principles • Diagnosis and proper treatment results in rapid correction of 167 Lactate 1.9 5 11 1.9 Protein 2+ • Treatment for AKA requires glucose administration, thiamine underlying metabolic derangements often followed by rapid Salicylate, ethylene glycol, Ketones 3+ supplementation, and volume repletion. methanol not detected Urobilinogen + • D5 NS IV until rehydrated, D5 1/2NS for maintenance. clinical improvement. 16.6 Digoxin: 0.3 ng/mL 17.2 241 RBCs 5/hpf • Thiamine 100 mg IV before glucose. • Failure to make the diagnosis can result in shock, hypokalemia, 49.3 PT/INR: >120/>11 Hyaline casts 21 • Supplement electrolytes PRN. VBG: pH 7.34, pCO2 25 • Continue treatment until anion gap closes, oral intake tolerated. 90% PMNs /hpf hypoglycemia, and acidosis. • Consider other causes of anion gap if gap does not close with Neutrophils 15.6x103/µL BNP: 66 pc/mL UTox: caffeine Trop: 0.1 ng/mL treatment Lipase: 13 U/L Case Description EKG: sinus tach • Consider sodium bicarbonate if despite treatment pH < 7.0. -

Diabetic Ketoacidosis
PRIMER Diabetic ketoacidosis Ketan K. Dhatariya1,2, Nicole S. Glaser3, Ethel Codner4 and Guillermo E. Umpierrez5 ✉ Abstract | Diabetic ketoacidosis (DKA) is the most common acute hyperglycaemic emergency in people with diabetes mellitus. A diagnosis of DKA is confirmed when all of the three criteria are present — ‘D’, either elevated blood glucose levels or a family history of diabetes mellitus; ‘K’, the presence of high urinary or blood ketoacids; and ‘A’, a high anion gap metabolic acidosis. Early diagnosis and management are paramount to improve patient outcomes. The mainstays of treatment include restoration of circulating volume, insulin therapy , electrolyte replacement and treatment of any underlying precipitating event. Without optimal treatment, DKA remains a condition with appreciable, although largely preventable, morbidity and mortality. In this Primer, we discuss the epidemiology , pathogenesis, risk factors and diagnosis of DKA and provide practical recommendations for the management of DKA in adults and children. Circulatory volume Diabetic ketoacidosis (DKA) is the most common acute acid decarboxylase and protein tyrosine phosphatase depletion hyperglycaemic emergency in people with diabetes mel- autoantibodies, as those who present with hyperosmo- A reduction in intravascular litus. DKA is the consequence of an absolute (that is, lar hyperglycaemic state (HHS), and their β-cell func- and/or extracellular fluid total absence of) or relative (that is, levels insufficient tion recovers with restoration of insulin secretion quickly volume, such that there may 2 be an inability to adequately to supress ketone production) lack of insulin and con- after treatment . Thus, individuals with ketosis-prone perfuse tissue. comitant elevation of counter-regulatory hormones, T2DM can often go back to oral glucose-lowering medi- usually resulting in the triad of hyperglycaemia, met- cation without the need for continuing insulin therapy. -

1 Effects of a Ketone-Caffeine Supplement on Cycling And
Effects of A Ketone-Caffeine Supplement On Cycling and Cognitive Performance in Chronic Keto-Adapted Participants THESIS Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Madison Lee Bowling Graduate Program in Kinesiology The Ohio State University 2018 Thesis Committee Dr. Jeff Volek Dr. William Kraemer Dr. Carl Maresh 1 Copyrighted by Madison Lee Bowling 2018 2 Abstract As research begins to broaden our understanding of the effects of low carbohydrate, high fat ketogenic diets to different populations, it is crucial to utilize evidence associated with the metabolic and physiological adaptation of chronic implementation. Specific populations are finding that nutritional ketosis may prove advantageous to athletic or cognitive performance. Nutritional ketosis may be identified by an elevated plasma ketone concentration within the blood range 0.5 to 5 mmol/L that results from a chronic implementation of a ketogenic diet. Recently, science shows that ketones contribute to a vast range of therapeutic and performance benefits associated with nutritional ketosis, as a result, exogenous ketone supplements have become commercially available which have proven to induce acute nutritional ketosis without restriction of carbohydrate intake. We previously showed that a supplement containing ketone salts and caffeine significantly increased performance in a non-keto adapted population. To date, there are no reports of whether ketone supplements have an ergogenic effect in an already keto-adapted population. The primary purpose of this study was to determine the performance and metabolic effects of a supplement containing ketone salts and caffeine in a group of people habituated to a ketogenic diet. -
Unit 4 Acid-Base Homeostasis
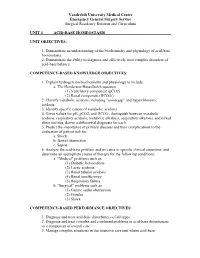
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 4 ACID-BASE HOMEOSTASIS UNIT OBJECTIVES: 1. Demonstrate an understanding of the biochemistry and physiology of acid-base homeostasis. 2. Demonstrate the ability to diagnose and effectively treat complex disorders of acid-base balance. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Explain hydrogen ion biochemistry and physiology to include: a. The Henderson-Hasselbalch equation (1) Ventilatory component (pCO2) (2) Renal component (HCO3-) 2. Classify metabolic acidosis, including "anion gap" and hyperchloremic acidosis. 3. Identify specific causes of metabolic acidosis. 4. Given values for pH, pCO2, and HCO3-, distinguish between metabolic acidosis, respiratory acidosis, metabolic alkalosis, respiratory alkalosis, and mixed abnormalities; derive a differential diagnosis for each. 5. Predict the importance of primary diseases and their complications to the evaluation of patient risk for: a. Shock b. Bowel obstruction c. Sepsis 6. Analyze the acid-base problem and its cause in specific clinical situations, and determine an appropriate course of therapy for the following conditions: a. "Medical" problems such as: (1) Diabetic ketoacidosis (2) Lactic acidosis (3) Renal tubular acidosis (4) Renal insufficiency (5) Respiratory failure b. "Surgical" problems such as: (1) Gastric outlet obstruction (2) Fistulas (3) Shock COMPETENCY-BASED PERFORMANCE OBJECTIVES: 1. Diagnose and treat acid-base disturbances of all types. 2. Diagnose and treat complex and combined problems in acid-base disturbances as a component of overall care. 3. Manage complex situations in the intensive care unit where acid-base Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum abnormalities coexist with other metabolic derangements, including: a. -

Lecture-1 Keto Acidosis, Bovine Ketosis, Ovine Pregnancy Toxemia
Lecture-1 Keto acidosis Ketoacidosis is a metabolic acidosis due to an excessive blood concentration of ketone bodies (acetone, acetoacetate and beta-hydroxybutyrate). Ketone bodies are released into the blood from the liver when hepatic lipid metabolism has changed to a state of increased ketogenesis. The abnormal accumulation of ketones in the body occurs due to excessive breakdown of fats in deficiency or inadequate use of carbohydrates. It is characterized by ketonuria, loss of potassium in the urine, and a fruity odor of acetone on the breath. Untreated, ketosis may progress to ketoacidosis, coma, and death. This condition is seen in starvation, occasionally in pregnancy if the intake of protein and carbohydrates is inadequate, and most frequently in diabetes mellitus. Different Types of Ketoacidosis Diabetes Keto Acidosis (DKA): Due to lack of insulin glucose uptake and metabolism by cells is decrased.Fatty acid catabolism increased in resulting in excess production of ketone bodies. Starvation Ketosis: Starvation leads to hypoglycemia as there is little or no absorption of glucose from intestine and also due to depletion of liver glycogen. In Fatty acid oxidation leads to excess ketone body. Bovine Ketosis Introduction Bovine ketosis occurs in the high producing dairy cows during the early stages of lactation, when the milk production is generally the highest. Abnormally high levels of the ketone bodies, acetone, acetoacetic and beta-hydroxy butyric acid and also iso- propanol appear in blood, urine and in milk. The alterations are accompanied by loss of appetite , weight loss, decrease in milk production and nervous disturbances. Hypoglycemia (starvation) is a common finding in bovine ketosis and in ovine pregnancy toxemia. -

Diabetic Ketoalkalosis in Children and Adults
Original Article Diabetic Ketoalkalosis in Children and Adults Emily A. Huggins, MD, Shawn A. Chillag, MD, Ali A. Rizvi, MD, Robert R. Moran, PhD, and Martin W. Durkin, MD, MPH and DR are calculated because the pH and bicarbonate may be near Objectives: Diabetic ketoacidosis (DKA) with metabolic alkalosis normal or even elevated. In addition to having interesting biochemical (diabetic ketoalkalosis [DKALK]) in adults has been described in the features as a complex acid-base disorder, DKALK can pose diagnostic literature, but not in the pediatric population. The discordance in the and/or therapeutic challenges. change in the anion gap (AG) and the bicarbonate is depicted by an Key Words: delta ratio, diabetic ketoacidosis, diabetic ketoalkalosis, elevated delta ratio (DR; rise in AG/drop in bicarbonate), which is metabolic alkalosis normally approximately 1. The primary aim of this study was to de- termine whether DKALK occurs in the pediatric population, as has been seen previously in the adult population. The secondary aim was iabetic ketoacidosis (DKA), a common and serious dis- to determine the factors that may be associated with DKALK. Dorder that almost always results in hospitalization, is de- Methods: A retrospective analysis of adult and pediatric cases with a fined by the presence of hyperglycemia, reduced pH, metabolic 1 primary or secondary discharge diagnosis of DKA between May 2008 and acidosis, elevated anion gap (AG), and serum or urine ketones. August 2010 at a large urban hospital was performed. DKALK was as- In some situations, a metabolic alkalosis coexists with DKA sumedtobepresentiftheDRwas91.2 or in cases of elevated bicarbonate. -

Alcohol Withdrawal
Alcohol withdrawal TERMINOLOGY CLINICAL CLARIFICATION • Alcohol withdrawal may occur after cessation or reduction of heavy and prolonged alcohol use; manifestations are characterized by autonomic hyperactivity and central nervous system excitation 1, 2 • Severe symptom manifestations (eg, seizures, delirium tremens) may develop in up to 5% of patients 3 CLASSIFICATION • Based on severity ○ Minor alcohol withdrawal syndrome 4, 5 – Manifestations occur early, within the first 48 hours after last drink or decrease in consumption 6 □ Manifestations develop about 6 hours after last drink or decrease in consumption and usually peak about 24 to 36 hours; resolution occurs in 2 to 7 days 7 if withdrawal does not progress to major alcohol withdrawal syndrome 4 – Characterized by mild autonomic hyperactivity (eg, tachycardia, hypertension, diaphoresis, hyperreflexia), mild tremor, anxiety, irritability, sleep disturbances (eg, insomnia, vivid dreams), gastrointestinal symptoms (eg, anorexia, nausea, vomiting), headache, and craving alcohol 4 ○ Major alcohol withdrawal syndrome 5, 4 – Progression and worsening of withdrawal manifestations, usually after about 24 hours from the onset of initial manifestations 4 □ Manifestations often peak around 50 hours before gradual resolution or may continue to progress to severe (complicated) withdrawal, particularly without treatment 4 – Characterized by moderate to severe autonomic hyperactivity (eg, tachycardia, hypertension, diaphoresis, hyperreflexia, fever); marked tremor; pronounced anxiety, insomnia, -

Diabetic Ketoacidosis: Evaluation and Treatment DYANNE P
Diabetic Ketoacidosis: Evaluation and Treatment DYANNE P. WESTERBERG, DO, Cooper Medical School of Rowan University, Camden, New Jersey Diabetic ketoacidosis is characterized by a serum glucose level greater than 250 mg per dL, a pH less than 7.3, a serum bicarbonate level less than 18 mEq per L, an elevated serum ketone level, and dehydration. Insulin deficiency is the main precipitating factor. Diabetic ketoacidosis can occur in persons of all ages, with 14 percent of cases occurring in persons older than 70 years, 23 percent in persons 51 to 70 years of age, 27 percent in persons 30 to 50 years of age, and 36 percent in persons younger than 30 years. The case fatality rate is 1 to 5 percent. About one-third of all cases are in persons without a history of diabetes mellitus. Common symptoms include polyuria with polydipsia (98 percent), weight loss (81 percent), fatigue (62 percent), dyspnea (57 percent), vomiting (46 percent), preceding febrile illness (40 percent), abdominal pain (32 percent), and polyphagia (23 percent). Measurement of A1C, blood urea nitro- gen, creatinine, serum glucose, electrolytes, pH, and serum ketones; complete blood count; urinalysis; electrocar- diography; and calculation of anion gap and osmolar gap can differentiate diabetic ketoacidosis from hyperosmolar hyperglycemic state, gastroenteritis, starvation ketosis, and other metabolic syndromes, and can assist in diagnosing comorbid conditions. Appropriate treatment includes administering intravenous fluids and insulin, and monitoring glucose and electrolyte levels. Cerebral edema is a rare but severe complication that occurs predominantly in chil- dren. Physicians should recognize the signs of diabetic ketoacidosis for prompt diagnosis, and identify early symp- toms to prevent it.