What Is the Public Health System?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Racial and Ethnic Disparities in Health Care, Updated 2010
RACIAL AND ETHNIC DISPARITIES IN HEALTH CARE, UPDATED 2010 American College of Physicians A Position Paper 2010 Racial and Ethnic Disparities in Health Care A Summary of a Position Paper Approved by the ACP Board of Regents, April 2010 What Are the Sources of Racial and Ethnic Disparities in Health Care? The Institute of Medicine defines disparities as “racial or ethnic differences in the quality of health care that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.” Racial and ethnic minorities tend to receive poorer quality care compared with nonminorities, even when access-related factors, such as insurance status and income, are controlled. The sources of racial and ethnic health care disparities include differences in geography, lack of access to adequate health coverage, communication difficulties between patient and provider, cultural barriers, provider stereotyping, and lack of access to providers. In addition, disparities in the health care system contribute to the overall disparities in health status that affect racial and ethnic minorities. Why is it Important to Correct These Disparities? The problem of racial and ethnic health care disparities is highlighted in various statistics: • Minorities have less access to health care than whites. The level of uninsurance for Hispanics is 34% compared with 13% among whites. • Native Americans and Native Alaskans more often lack prenatal care in the first trimester. • Nationally, minority women are more likely to avoid a doctor’s visit due to cost. • Racial and ethnic minority Medicare beneficiaries diagnosed with dementia are 30% less likely than whites to use antidementia medications. -

The French Health Care System
The french health care system The french health care system VICTOR RODWIN PROFESSOR OF HEALTH POLICY AND MANAGEMENT WAGNER SCHOOL OF PUBLIC SERVICE, NEW YORK UNIVERSITY NEW YORK, USA ABSTRACT: The French health care system is a model of national health insurance (NHI) that provides health care coverage to all legal residents. It is an example of public social security and private health care financing, combined with a public-private mix in the provision of health care services. The French health care system reflects three underlying political values: liberalism, pluralism and solidarity. This article provides a brief overview of how French NHI evolved since World War II; its financing health care organization and coverage; and most importantly, its overall performance. ntroduction. Evolution, coverage, financing and organization The French health care system is a model of national health Evolution: French NHI evolved in stages and in response to Iinsurance (NHI) that provides health care coverage to all legal demands for extension of coverage. Following its original passage, residents. It is not an example of socialized medicine, e.g. Cuba. in 1928, the NHI program covered salaried workers in industry and It is not an example of a national health service, as in the United commerce whose wages were under a low ceiling (Galant, 1955). Kingdom, nor is it an instance of a government-run health care In 1945, NHI was extended to all industrial and commercial workers system like the United States Veterans Health Administration. and their families, irrespective of wage levels. The extension of French NHI, in contrast, is an example of public, social security and coverage took the rest of the century to complete. -

Different Perspectives for Assigning Weights to Determinants of Health
COUNTY HEALTH RANKINGS WORKING PAPER DIFFERENT PERSPECTIVES FOR ASSIGNING WEIGHTS TO DETERMINANTS OF HEALTH Bridget C. Booske Jessica K. Athens David A. Kindig Hyojun Park Patrick L. Remington FEBRUARY 2010 Table of Contents Summary .............................................................................................................................................................. 1 Historical Perspective ........................................................................................................................................ 2 Review of the Literature ................................................................................................................................... 4 Weighting Schemes Used by Other Rankings ............................................................................................... 5 Analytic Approach ............................................................................................................................................. 6 Pragmatic Approach .......................................................................................................................................... 8 References ........................................................................................................................................................... 9 Appendix 1: Weighting in Other Rankings .................................................................................................. 11 Appendix 2: Analysis of 2010 County Health Rankings Dataset ............................................................ -

Environmental Health
Environmental "ealth In Minnesota '·' ! .\ " ' Strengthening Pabllc Healtll Leadership In Environmental Health Il Il I j fml Minnesota · lIDJ Department of Health lli&ilhl ~==~-:.i:.ltft -------- Janaary199J '.~ • - " . Environmental Health In Minnesota Strengthening Public Health Leadership In Environmental Health A Report of the Environmental Health Work Group of the State Community Health Services Advisory Committee Approved December 4, 1992 Published by the ., ,f Minnesota Department of Health Environmental Health In Minnesota Strengthening Public Health Leadership In Environmental Health Table of Contents Introduction . i Work Group charge and membership . ii Part I Background and Recommendations . 1 Contributions of Public Health In Environmental Health and Protection . 3 State Roles In Environmental Health . 6 Local Roles In Environmental Health . 7 Recommendations . 10 Part II Framework For Deciding How to Organize Environmental Services . 13 Keeping a Public Health Perspective In Environmental Health and Protection . 23 Part Ill Profile of Environmental Health In Minnesota . 25 Profile of State Environmental Health . 25 Profile of Local Environmental Health . 26 Current Organization of Local Environmental Health Programs . 31 Part IV Related Documents MACHA Position Paper Current Roles and Challenges of Local Health Departments In Environmental Health, NACHO Directory of State Environmental Health Programs (published separately) Cover art by Kathy Marschall Minnesota Department of Health ) Community Health Seroices Division \ ' ···~ )' Environmental Health In Minnesota + i Introduction Environmental heal.th has been an integral part of the public health mission for over a century. With the rest of public health, environmental health shares a basis In science and a focus on protecting and promoting the health of the public. In the past twenty years an explosion of environmental laws has given greater visibility to . -

Page 1 the Public Health Benefits of Sanitation Interventions
The Public Health Benefits of Sanitation Interventions EPAR Brief No. 104 Jacob Lipson, Professor Leigh Anderson & Professor Susan Bolton Prepared for the Water & Sanitation Team of the Bill & Melinda Gates Foundation Evans School Policy Analysis and Research (EPAR) Professor Leigh Anderson, PI and Lead Faculty Associate Professor Mary Kay Gugerty, Lead Faculty December 10, 2010 Introduction Limited sanitation infrastructure, poor hygienic practices, and unsafe drinking water negatively affect the health of millions of people in the developing world. Using sanitation interventions to interrupt disease pathways can significantly improve public health.1 Sanitation interventions primarily benefit public health by reducing the prevalence of enteric pathogenic illnesses, which cause diarrhea. Health benefits are realized and accrue to the direct recipients of sanitation interventions and also to their neighbors and others in their communities. In a report to the United Nations Development Programme (UNDP), Hutton et al. (2006) estimate that the cost- benefit ratio of sanitation interventions in all developing countries worldwide is 11.2.2 This literature review summarizes the risks of inadequate sanitation to public health and presents the empirical evidence on the public health benefits of complete, intermediate and multiple factor sanitation interventions. The sanitation literature frequently uses inconsistent terminology to describe sanitation infrastructure, technologies and intervention types. Where feasible, we report study results using the original terminology of the authors, while also using consistent terminology to facilitate comparisons across studies. In this review and in much of the literature, sanitation interventions are defined as improvements which provide public or household fecal disposal facilities, and/or improve community fecal disposal and treatment methods.3,4 Sanitation interventions are distinct from water interventions, which focus on increasing access to clean water or improving water quality at drinking water sources or points of use. -

Hand Hygiene: Clean Hands for Healthcare Personnel
Core Concepts for Hand Hygiene: Clean Hands for Healthcare Personnel 1 Presenter Russ Olmsted, MPH, CIC Director, Infection Prevention & Control Trinity Health, Livonia, MI Contributions by Heather M. Gilmartin, NP, PhD, CIC Denver VA Medical Center University of Colorado Laraine Washer, MD University of Michigan Health System 2 Learning Objectives • Outline the importance of effective hand hygiene for protection of healthcare personnel and patients • Describe proper hand hygiene techniques, including when various techniques should be used 3 Why is Hand Hygiene Important? • The microbes that cause healthcare-associated infections (HAIs) can be transmitted on the hands of healthcare personnel • Hand hygiene is one of the MOST important ways to prevent the spread of infection 1 out of every 25 patients has • Too often healthcare personnel do a healthcare-associated not clean their hands infection – In fact, missed opportunities for hand hygiene can be as high as 50% (Chassin MR, Jt Comm J Qual Patient Saf, 2015; Yanke E, Am J Infect Control, 2015; Magill SS, N Engl J Med, 2014) 4 Environmental Surfaces Can Look Clean but… • Bacteria can survive for days on patient care equipment and other surfaces like bed rails, IV pumps, etc. • It is important to use hand hygiene after touching these surfaces and at exit, even if you only touched environmental surfaces Boyce JM, Am J Infect Control, 2002; WHO Guidelines on Hand Hygiene in Health Care, WHO, 2009 5 Hands Make Multidrug-Resistant Organisms (MDROs) and Other Microbes Mobile (Image from CDC, Vital Signs: MMWR, 2016) 6 When Should You Clean Your Hands? 1. Before touching a patient 2. -
What the Public Thinks About Menatl Health and Mental Illness
What the Public Thinks about Mental Health and ~entaleI1lness A paper presented by Shirley A. Star, Senior Study Director National Opinion Research Center, University of Chicago to the Annual Meeting The National Association for Mental Health, Inc. November 19, 1952 For the past two and a half years, the National Opinion Research Center has been engaged upon a pioneering study of the-American public's thinking in the field of mental health, under the joint sponsorship of the National Association for Mental Health and the National Institute of Mental Health, It is a vast and ambitious project, and I'm afraid that the title which has been assigned to my remarks about .the study is going to prove to be misleading in at least two ways. In the first place, and this must be obvious, both the title given me and the scope of the study cover Ear more ground than I could possibly present in the course of one afternoon. About all I can do today is hit a few of the high spots in public thinking and emphasize beforehand that the study aims to be inclusive. You can pretty well assume that it contains some information on just about any question in the area you might raise, even though I don't refer to many of them. So, as they say in the more enterprising shops--"If you don't see what you want, ask for it," In the second place, and this is more serious, I am in the em- barrassing position of having to stand here this afternoon and honestly- -2- admit that I don1t -know what the public thinks as yet. -

Fundamentals of Public Health Nutrition (3 Credit Hours) Fall: 2018 Delivery Format: E-Learning in Canvas
University of Florida College of Public Health & Health Professions Syllabus PHC 6521: Fundamentals of Public Health Nutrition (3 credit hours) Fall: 2018 Delivery Format: E-Learning in Canvas Instructor Name: Dr. von Castel Room Number: FSHN 227 Phone Number: 352 Email Address: [email protected] *****PLEASE USE THIS NOT CANVAS Office Hours: by appointment via phone,conferences (in canvas) or Lync(Microsoft) Preferred Course Communications: email through ufl.edu Prerequisites None PURPOSE AND OUTCOME Public health nutrition involves the promotion of health through nutrition and the prevention of nutrition related disease in a population. It focuses on improving the food choices, dietary intake, and nutritional status at the community, regional, or national level. The public health nutrition professional works to assess nutritional problems and needs by considering environmental causes, identifying intervention points, developing policies and programs to intervene at those points, implementing the policies or programs, and evaluating the effectiveness of the intervention. Course Overview This course will provide an introduction to Public Health Nutrition and the role of the Public Health Nutrition professional. Emphasis will be on definition, identification and prevention of nutrition related disease, as well as improving health of a population by improving nutrition. Malnutrition will be discussed on a societal, economic, and environmental level. It will include the basics of nutritional biochemistry as it relates to malnutrition of a community and targeted intervention. Finally, it will review existing programs and policies, including strengths, weaknesses and areas for modification or new interventions. Relation to Program Outcomes MPH Competencies covered 1. Monitor health status to identify and solve community health problems 2. -

Chapter 9: Monitoring, Surveillance, and Investigation of Health Threats
Chapter 9: Monitoring, surveillance, and investigation of health threats SUMMARY POINTS · Monitoring, surveillance and investigation of health threats are vital capabilities for an effective health system. The International Health Regulations (2005) require countries to maintain an integrated, national system for public health surveillance and response, and set out the core capabilities that countries are required to achieve. · Systematic monitoring of serious infectious diseases and other conditions is typically achieved through notifiable diseases legislation based on clinical observation and laboratory confirmation. Clinical and laboratory-based surveillance also provides the basis for systematic collection of vital statistics (births, deaths, causes of death), and may extend to the reporting and analysis of risk factors for noncommunicable diseases and injuries. Systematic collection of these data informs the allocation of resources and facilitates evaluation of community-based and population-level prevention strategies. · Clinical and laboratory surveillance are passive systems that may be enhanced by sentinel surveillance and/or community-based surveillance strategies that rely on a wider range of people, including non-medical personnel. Suspected cases identified in this way must be treated with respect, protected from discrimination, with diagnosis confirmed by qualified health workers at the earliest opportunity. · A significant degree of stigma may attach to some diseases, such as HIV, sexually transmitted infections and diabetes. Notifiable diseases legislation should require the protection of personal information, and clearly define any exceptions. Concerns about discrimination and breach of privacy may be addressed by requiring certain diseases to be reported on an anonymous or de- identified basis. · In some countries, legislation or regulations may be used to establish or enhance a comprehensive public health surveillance system. -
Core Principles to Reframe Mental and Behavioral Health Policy 2
Getty Images / Maskot Core Principles to Reframe Mental and Behavioral Health Policy January 2021 Historic and modern-day policies rooted in discrimination and oppression have created and widened harmful inequities impacting many communities of color. Effectively and equitably addressing mental health requires intervening at systemic and policy levels to dismantle the structures that produce negative outcomes like generational poverty, intergenerational and cultural trauma, racism, sexism, and ableism. Changing social, economic, and physical environments alongside key mental and behavioral health supports through immediate relief and longer-term fixes impact individual and community mental health and wellbeing. An individual’s mental health is impacted by and informs nearly every aspect of their life, identity, and community. CLASP looks at how one’s social, economic, and physical environment impact individual and community views of mental health and wellbeing. To improve mental health outcomes, we must think about an individual and family’s economic security, family support, and their community’s built environment. CLASP recognizes the influence of intergenerational and cultural trauma on communities and believes that all mental and behavioral health practices should be trauma-informed and healing- centered. Policymakers must significantly reform and reimagine systems that support the wellbeing of people with low incomes. This includes, but is not exclusive to: • Universal health coverage, as noted in our health care principles; • Recognizing -
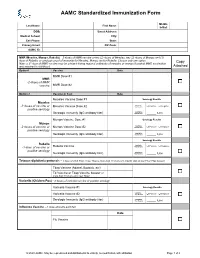
AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC. -

COVID-19 Vaccination Requirement (Proclamation 21-14.1) for Health Care Providers, Workers and Settings
Updated September 2021 DOH 505-160 COVID-19 Vaccination Requirement (Proclamation 21-14.1) for health care providers, workers and settings Link to proclamation: 21-14.1 - COVID-19 Vax Washington General Proclamation Questions What does Proclamation 21-14.1 do? Proclamation 21-14.1, issued by Governor Inslee on August 20, 2021, made numerous changes to Proclamation 21-14, issued by Governor Inslee on August 9, 2021, but left the same core requirements in place. As before, the proclamation requires health care providers, defined broadly to include not only licensed health care providers but also all employees, contractors, and volunteers who work in a health care setting, to be fully vaccinated against COVID-19 by October 18, 2021. It also requires operators of health care settings to verify the vaccination status of: a) Every employee, volunteer, and contractor who works in the health care setting, whether or not they are licensed or providing health care services, and b) Every employee, volunteer, and contractor who provides health care services for the health care setting operator. On what legal grounds can this be imposed? In response to the emerging COVID-19 threat, Governor Inslee declared a state of emergency on February 29, 2020, using his broad emergency authority under chapter 43.06 RCW. More specifically, under RCW 43.06.220, after a state of emergency has been declared, the governor may prohibit any activity that they believe should be prohibited to help preserve and maintain life, health, property or the public peace. Under an emergency such as this, the governor’s paramount duty is to protect the health and safety of our communities.