Anafranil (Clomipramine Hydrochloride) Tablets 1 Name of the Medicine 2 Qualitative and Quant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -

Serotonin's Role in Alcohol's Effects on the Brain
NEUROTRANSMITTER REVIEW IMPERATO, A., AND DI CHIARA, G. Preferential stimulation of dopamine release in the nucleus accumbens of freely moving rats by ethanol. Journal SEROTONIN’S ROLE IN ALCOHOL’S of Pharmacology and Experimental Therapeutics 239:219–228, 1986. EFFECTS ON THE BRAIN KITAI, S.T., AND SURMEIER, D.J. Cholinergic and dopaminergic modula- tion of potassium conductances in neostriatal neurons. Advances in David M. Lovinger, Ph.D. Neurology 60:40–52, 1993. LE MOINE, C.; NORMAND, E.; GUITTENY, A.F.; FOUQUE, B.; TEOULE, R.; AND BLOCH, B. Dopamine receptor gene expression by enkephalin Serotonin is an important brain chemical that acts as a neurons in rat forebrain. Proceedings of the National Academy of Sciences neurotransmitter to communicate information among USA 87:230–234, 1990. nerve cells. Serotonin’s actions have been linked to al- LE MOINE, C.; NORMAND, E.; AND BLOCH, B. Phenotypical character- cohol’s effects on the brain and to alcohol abuse. ization of the rat striatal neurons expressing the D1 dopamine receptor Alcoholics and experimental animals that consume gene. Proceedings of the National Academy of Sciences USA 88: large quantities of alcohol show evidence of differences 4205–4209, 1991. in brain serotonin levels compared with nonalcoholics. LYNESS, W.H., AND SMITH F.L. Influence of dopaminergic and sero- Both short- and long-term alcohol exposure also affect tonergic neurons on intravenous ethanol self-administration in the rat. the serotonin receptors that convert the chemical sig- Pharmacology and Biochemistry of Behavior 42:187–192, 1992. nal produced by serotonin into functional changes in the signal-receiving cell. -

Dosulepin Prescribing
SAFETY BULLETIN: DOSULEPIN PRESCRIBING In December 2007, the Medicines and Healthcare Regulatory Agency (MHRA) issued safety advice around prescribing of dosulepin, related to the narrow margin between therapeutic doses and potentially fatal doses. Nevertheless, dosulepin continues to be prescribed widely. Over eight years after the safety advice was published, prescribing of dosulepin in the Dorset area remains high. In the South West area, Dorset CCG was the highest prescriber of dosulepin for the 2015/16 financial year (3.238% of all antidepressant items). Of the 209 CCGs in the UK, Dorset is the fourteenth highest prescriber of dosulepin, and well above the national average of 2.111%. The following points summarise the reasons that dosulepin is not recommended for prescribing nationally, and in Dorset: Dosulepin has a small margin of safety between the (maximum) therapeutic dose and potentially fatal doses. The NICE guideline on depression in adults recommends that dosulepin should not be prescribed for adults with depression because evidence supporting its tolerability relative to other antidepressants is outweighed by the increased cardiac risk and toxicity in overdose. Dosulepin has also been used ‘off label’ in other indications such as fibromyalgia and neuropathic pain. However the evidence for use in in this way is weak, and is not recommended. The lethal dose of dosulepin is relatively low and can be potentiated by alcohol and other CNS depressants. Dosulepin overdose is associated with high mortality and can occur rapidly, even before hospital treatment can be received. Onset of toxicity occurs within 4-6 hours. Every year, up to 200 people in England and Wales fatally overdose with dosulepin. -

The Serotonergic System in Migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone
J Headache Pain (2001) 2:S43–S46 © Springer-Verlag 2001 MIGRAINE AND PATHOPHYSIOLOGY Massimo Leone The serotonergic system in migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone Abstract Serotonin (5-HT) and induce migraine attacks. Moreover serotonin receptors play an impor- different pharmacological preventive tant role in migraine pathophysiolo- therapies (pizotifen, cyproheptadine gy. Changes in platelet 5-HT content and methysergide) are antagonist of are not casually related, but they the same receptor class. On the other may reflect similar changes at a neu- side the activation of 5-HT1B-1D ronal level. Seven different classes receptors (triptans and ergotamines) of serotoninergic receptors are induce a vasocostriction, a block of known, nevertheless only 5-HT2B-2C neurogenic inflammation and pain M. Leone • A. Rigamonti • D. D’Amico and 5HT1B-1D are related to migraine transmission. L. Grazzi • S. Usai • G. Bussone (౧) syndrome. Pharmacological evi- C. Besta National Neurological Institute, Via Celoria 11, I-20133 Milan, Italy dences suggest that migraine is due Key words Serotonin • Migraine • e-mail: [email protected] to an hypersensitivity of 5-HT2B-2C Triptans • m-Chlorophenylpiperazine • Tel.: +39-02-2394264 receptors. m-Chlorophenylpiperazine Pathogenesis Fax: +39-02-70638067 (mCPP), a 5-HT2B-2C agonist, may The 5-HT receptor family is distinguished from all other 5- Introduction 1 HT receptors by the absence of introns in the genes; in addi- tion all are inhibitors of adenylate cyclase [1]. Serotonin (5-HT) and serotonin receptors play an important The 5-HT1A receptor has a high selective affinity for 8- role in migraine pathophysiology. -

Clomipramine | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Clomipramine This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Anafranil Brand Names: Canada Anafranil; MED ClomiPRAMINE; TARO-Clomipramine Warning Drugs like this one have raised the chance of suicidal thoughts or actions in children and young adults. The risk may be greater in people who have had these thoughts or actions in the past. All people who take this drug need to be watched closely. Call the doctor right away if signs like low mood (depression), nervousness, restlessness, grouchiness, panic attacks, or changes in mood or actions are new or worse. Call the doctor right away if any thoughts or actions of suicide occur. This drug is not approved for use in all children. Talk with the doctor to be sure that this drug is right for your child. What is this drug used for? It is used to treat obsessive-compulsive problems. It may be given to you for other reasons. Talk with the doctor. Clomipramine 1/8 What do I need to tell my doctor BEFORE I take this drug? If you have an allergy to clomipramine or any other part of this drug. If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you have had a recent heart attack. If you are taking any of these drugs: Linezolid or methylene blue. -

Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients Research Questions: 1. How many schizophrenia patients are prescribed recommended first-line second-generation treatments for schizophrenia? 2. How many schizophrenia patients switch to an injectable antipsychotic after stabilization on an oral antipsychotic? 3. How many schizophrenia patients are prescribed 2 or more concomitant antipsychotics? 4. Are claims for long-acting injectable antipsychotics primarily billed as pharmacy or physician administered claims? 5. Does adherence to antipsychotic therapy differ between patients with claims for different routes of administration (oral vs. long-acting injectable)? Conclusions: In total, 4663 schizophrenia patients met inclusion criteria, and approximately 14% of patients (n=685) were identified as treatment naïve without claims for antipsychotics in the year before their first antipsychotic prescription. Approximately 45% of patients identified as treatment naïve had a history of remote antipsychotic use, but it is unclear if antipsychotics were historically prescribed for schizophrenia. Oral second-generation antipsychotics which are recommended as first-line treatment in the MHCAG schizophrenia algorithm were prescribed as initial treatment in 37% of treatment naive patients and 28% of all schizophrenia patients. Recommended agents include risperidone, paliperidone, and aripiprazole. Utilization of parenteral antipsychotics was limited in patients with schizophrenia. Overall only 8% of patients switched from an oral to an injectable therapy within 6 months of their first claim. Approximately, 60% of all schizophrenia patients (n=2512) had claims for a single antipsychotic for at least 12 continuous weeks and may be eligible to transition to a long-acting injectable antipsychotic. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
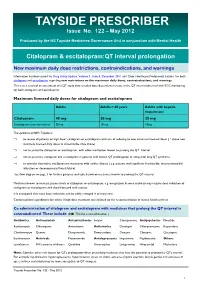
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

FDA Approved Drugs with Broad Anti-Coronaviral Activity Inhibit SARS-Cov-2 in Vitro
bioRxiv preprint doi: https://doi.org/10.1101/2020.03.25.008482; this version posted March 27, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. FDA approved drugs with broad anti-coronaviral activity inhibit SARS-CoV-2 in vitro Stuart Weston1, Rob Haupt1, James Logue1, Krystal Matthews1 and Matthew B. Frieman*1 1 - Department of Microbiology and Immunology, University of Maryland School of Medicine, 685 W. Baltimore St., Room 380, Baltimore, MD, 21201, USA *Corresponding author. Email: [email protected] Key words: SARS-CoV-2, nCoV-2019, COVID-19, drug repurposing, FDA approved drugs, antiviral therapeutics, pandemic, chloroquine, hydroxychloroquine AbstraCt SARS-CoV-2 emerged in China at the end of 2019 and has rapidly become a pandemic with over 400,000 recorded COVID-19 cases and greater than 19,000 recorded deaths by March 24th, 2020 (www.WHO.org) (1). There are no FDA approved antivirals or vaccines for any coronavirus, including SARS-CoV-2 (2). Current treatments for COVID-19 are limited to supportive therapies and off-label use of FDA approved drugs (3). Rapid development and human testing of potential antivirals is greatly needed. A potentially quicker way to test compounds with antiviral activity is through drug re-purposing (2, 4). Numerous drugs are already approved for use in humans and subsequently there is a good understanding of their safety profiles and potential side effects, making them easier to test in COVID-19 patients. -

NORPRAMIN® (Desipramine Hydrochloride Tablets USP)
NORPRAMIN® (desipramine hydrochloride tablets USP) Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of NORPRAMIN or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. NORPRAMIN is not approved for use in pediatric patients. (See WARNINGS: Clinical Worsening and Suicide Risk, PRECAUTIONS: Information for Patients, and PRECAUTIONS: Pediatric Use.) DESCRIPTION NORPRAMIN® (desipramine hydrochloride USP) is an antidepressant drug of the tricyclic type, and is chemically: 5H-Dibenz[bƒ]azepine-5-propanamine,10,11-dihydro-N-methyl-, monohydrochloride. 1 Reference ID: 3536021 Inactive Ingredients The following inactive ingredients are contained in all dosage strengths: acacia, calcium carbonate, corn starch, D&C Red No. 30 and D&C Yellow No. 10 (except 10 mg and 150 mg), FD&C Blue No. 1 (except 25 mg, 75 mg, and 100 mg), hydrogenated soy oil, iron oxide, light mineral oil, magnesium stearate, mannitol, polyethylene glycol 8000, pregelatinized corn starch, sodium benzoate (except 150 mg), sucrose, talc, titanium dioxide, and other ingredients. -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020