NCCN Guidelines ®
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thromboprophylaxis for Venous Thromboembolism UHL Guideline
Guidelines for Pharmacological and Mechanical Thromboprophylaxis for venous thromboembolism. Approved By: Policy and Guideline Committee Date Approved: 12 February 2016 Trust Reference: B9/2016 Version: V4 – 16 August 2019 Policy and Guideline Committee Supersedes: V3 February 2016 Author / Originator(s): Simon Rudge, Venous Thrombosis Nurse Name of Responsible Thrombosis Prevention Committee Committee/Individual: Review Date: August 2022 CONTENTS Section Page 1. Introduction 3 2. Policy Scope 5 VTE Risk Assessment and Pharmacological and Mechanical venous 3. 6 thromboprophylaxis 4. Patient information 8 5. Mechanical thromboprophylaxis. Application and management guide 9 6. Nursing care 12 7. References 12 8. Legal Liability Guideline Statement 12 Appendix 1 Derogation from NICE NG89: VTE risk assessment of 16 & 17yr olds 13 Appendix 2a/2a1/2b/2c VTE risk assessment tools 14-18 Appendix 3 NICE CG92 algorithm for VTE thromboprophylaxis in medical patients 19 Appendix 4 Consensus of risk factors for VTE in surgical patients 20 Appendix 5 UHL and East Midlands approved List of cohort Day Case procedures 21 Appendix 6 Thromboprophylaxis administration guide: Dalteparin 22 Appendix 7 Derogation from NICE NG89: minimum of 7 days low molecular weight 23 heparin for acutely unwell medical patients Appendix 8 Indications for mechanical thromboprophylaxis algorithm 24 Appendix 8a Indications for mechanical thromboprophylaxis with intermittent 25 pneumatic compression devices algorithm Appendix 9 Quick reference guide of NICE NG89 26 Summary of key changes: Addition of procedure specific recommendations from NG89. Inclusion of discharge recommendations. Inclusion of statement regarding medicines of animal origin. Inclusion of training requirements Inclusion of statements of derogation from NG89 Addition of quick reference guide of NG89. -

Hemosil ® Liquid Anti-Xa
H E M O S I L® LIQUID ANTI-XA Measuring heparin and apixaban: Simple, fast, 24/7 • Liquid formulation, ready-to-use • One-stage, chromogenic anti-Xa assay • Universal calibration for unfractionated heparin (UFH) and low molecular weight heparin (LMWH) • Drug specific calibrators and controls for measurement of apixaban Measuring heparin and apixaban Unfractionated and low molecular weight heparin Heparin is a highly sulfated polysaccharide Laboratory monitoring is extremely important to characterized by a wide molecular weight range and assess the appropriate level of anticoagulation in potent anticoagulant activity. It exists either as UFH patients receiving UFH. Anti-Xa is recommended for or as depolymerized LMWH. UFH and LMWH have measuring both UFH and LMWH. a rapid anticoagulant effect and are used in the prevention and treatment of venous thrombosis and Anti-Xa testing for measuring UFH helps improve acute coronary syndrome. quality of care and patient experience while reducing costs, when compared with APTT testing.1 UFH and LMWH anticoagulant activity occurs when The advantages include: a complex with antithrombin (AT) is formed, • Higher precision potentiating its anticoagulant activity up to • Lower levels of discordant results1,2,4 1,000-fold, which inactivates both thrombin (FIIa) • Faster time to achieve therapeutic levels1,3,4 and Factor Xa (FXa). UFH acts through both FIIa 1,3,4,5 and FXa inhibition, while LMWH is a more efficient • Fewer tests and dosage changes catalyst for FXa inhibition. Direct Xa inhibitors Anticoagulation for patients with venous DOACs do not require routine monitoring. However, thromboembolism (VTE) previously included there are specific instances when an understanding heparin, heparin derivatives and/or oral vitamin K of the DOAC concentration in a patient sample may antagonists. -
The Management of Anticoagulants Using the Chart: – Low Molecular Weight Heparins (I.E
WA Adult Anticoagulation Medication Chart Overview This presentation will provide an overview of: • The layout of the WA Anticoagulation Medication Chart (WA AMC) • The management of anticoagulants using the chart: – Low Molecular Weight Heparins (i.e. enoxaparin) – Unfractionated heparin (UFH) – Warfarin – Direct oral anticoagulants (DOACs) Anticoagulants – High Risk Medications • Anticoagulants are consistently identified as causing preventable harm to patients. • Top 20 medications involved in medication errors (July 2016 - June 2017) 1. Paracetamol 11. Buprenorphine 2. Enoxaparin 12. Targin (Oxycodone / naloxone) 3. Novorapid Insulin 13. Warfarin 4. Tramadol 14. Diazepam 5. Heparin 15. Tapentadol 6. Fentanyl 16. Metformin 7. Piperacillin & Tazobactam 17. Clonazepam 8. Oxycodone 18. Frusemide 9. Lantus Insulin 19. Hydromorphone 10. Vancomycin 20. Quetiapine • When used in error or omitted, they can cause life-threatening or fatal bleeding or thrombosis. Those most commonly prescribed anticoagulants are: –unfractionated heparin –low-molecular weight heparin (LMWH) • enoxaparin sodium (Clexane®) • dalteparin sodium (Fragmin®) and – warfarin. Direct oral anticoagulants are also available and are being prescribed more frequently: –dabigatran (Pradaxa®) –rivaroxaban (Xarelto®) –apixaban (Eliquis®). Factors that increase the potential for error and harm include: • Low margin for error – over-dose → bleeding – under-dose or omission → thrombosis • Wide variation in individual patient response – multiple indications – wide range and complexity of dosage – frequent dose adjustment/monitoring – interaction with other medicines, herbals, over-the-counter products, food and alcohol. Benefits of the WA Anticoagulant Medication Chart • Provides one chart for all anticoagulant prescriptions to reduce the risk of duplicate prescribing. • Point of care guidelines for initiation, monitoring and reversal of anticoagulants. • Enables the effective achievement of therapeutic levels. -

Dalteparin Sodium Injection) in Children with Venous Thromboembolism with Or Without Malignancies
FRAG-A001-201 (A6301094) Final Protocol Amendment 9, 18 October 2016 CLINICAL STUDY PROTOCOL A THREE MONTH PROSPECTIVE OPEN LABEL STUDY OF THERAPY WITH FRAGMIN® (DALTEPARIN SODIUM INJECTION) IN CHILDREN WITH VENOUS THROMBOEMBOLISM WITH OR WITHOUT MALIGNANCIES Compound: PN180524 Compound Name : Dalteparin Sodium Injection (Fragmin®) United States (US) Investigational New IND 79,617 Drug (IND) Number: European Clinical Trials Database 2016-000394-21 (EudraCT) #: Protocol Number: FRAG-A001-201 (A6301094) Phase: II Version #: Amendment 9 – 18 October 2016 Pfizer Inc 235 East 42nd Street New York, NY 10017 - Do Not Distribute Page 1 FRAG-A001-201 (A6301094) Final Protocol Amendment 9, 18 October 2016 Document History This amendment incorporates all revisions to date, including amendments made at the request of country health authorities, institutional review boards/ethics committees (IRBs/ECs), etc. Document Date Summary of Changes and Rationale Original Protocol June 23, 2008 Legacy Eisai Inc Protocol Protocol Amendment 1 September 04, 2008 Legacy Eisai Inc Protocol Correction to Amendment 1 January 05, 2009 Legacy Eisai Inc Protocol Protocol Amendment 2 February 20, 2009 Legacy Eisai Inc Protocol Protocol Amendment 3 September 15, 2010 Legacy Eisai Inc Protocol Protocol Amendment 4 September 01, 2011 Legacy Eisai Inc Protocol Protocol Amendment 5 April 21, 2015 Administrative changes per transition of study to Pfizer Inc from Eisai; Updating of Safety Section per Pfizer safety reporting processes and procedures, and other relevant sections per Pfizer Inc processes and procedures. Protocol Amendment 6 09 September 2015 This version was never finalized or submitted and was replaced by Amendment 7. Protocol Amendment 7 18 November 2015 Includes protocol modifications endorsed by FDA in a Type C Meeting conducted on 05 November 2015, including updating age cohort groups, inclusion of all patients with VTE and removal of the central imaging reader and Adjudication Committee. -

Perioperative Management of Patients Treated with Antithrombotics in Oral Surgery
SFCO/Perioperative management of patients treated with antithrombotic agents in oral surgery/Rationale/July 2015 SOCIÉTÉ FRANÇAISE DE CHIRURGIE ORALE [FRENCH SOCIETY OF ORAL SURGERY] IN COLLABORATION WITH THE SOCIÉTÉ FRANÇAISE DE CARDIOLOGIE [FRENCH SOCIETY OF CARDIOLOGY] AND THE PERIOPERATIVE HEMOSTASIS INTEREST GROUP Space Perioperative management of patients treated with antithrombotics in oral surgery. RATIONALE July 2015 P a g e 1 | 107 SFCO/Perioperative management of patients treated with antithrombotic agents in oral surgery/Rationale/July 2015 Abbreviations ACS Acute coronary syndrome(s) ADP Adenosine diphosphate Afib Atrial Fibrillation AHT Arterial hypertension Anaes Agence nationale d’accréditation et d’évaluation en santé [National Agency for Accreditation and Health Care Evaluation] APA Antiplatelet agent(s) aPTT Activated partial thromboplastin time ASA Aspirin BDMP Blood derived medicinal products BMI Body mass index BT Bleeding Time cAMP Cyclic adenosine monophosphate COX-1 Cyclooxygenase 1 CVA Cerebral vascular accident DIC Disseminated intravascular coagulation DOA Direct oral anticoagulant(s) DVT Deep vein thrombosis GEHT Study Group on Hemostasis and Thrombosis (groupe d’étude sur l’hémostase et la thrombose) GIHP Hemostasis and Thrombosis Interest Group (groupe d’intérêt sur l’hémostase et la thrombose) HAS Haute autorité de santé [French Authority for Health] HIT Heparin-induced thrombocytopenia IANB Inferior alveolar nerve block INR International normalized ratio IV Intravenous LMWH Low-molecular-weight heparin(s) -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Antithrombotic Therapy During Pregnancy
ARC Journal of Pharmaceutical Sciences (AJPS) Volume 1, Issue 2, July – September 2015, PP 16-20 www.arcjournals.org Antithrombotic Therapy During Pregnancy Sihana Ahmeti Lika1*, Bujar H. Durmishi2, Agim Shabani2, Merita Dauti1, Ledjan Malaj3 1 Faculty of Medical Sciences, Department of Pharmacy, State University of Tetova, Ilindeni Str. n.n., 1200 Tetova, R. of Macedonia [email protected] 2 Faculty of Mathematical - Natural Sciencese, Department of Chemistry, State University of Tetova, Ilindeni Str. n.n., 1200 Tetova, R. of Macedonia 3 Faculty of Pharmacy, Medical University of Tirana, of Albania Abstract: Antithrombotic therapy is the main therapy for acute deep vein thrombosis. The objectives of anticoagulant therapy in the initial treatment are to prevent thrombus extension and early and late recurrences of deep vein thrombosis and pulmonary embolism. The main objective of our study is to analyze the usage of low molecular weight heparins in women, during the period of pregnancy. Our study, represents a retrospective study, which was undertaken during 01 July – 31 December 2013, in the Department of Gynecology and Obstetrics, at Clinical Hospital in Tetova. Among of 817 pregnant women, 277 of them received anticoagulant therapy, respectively Low Molecular Weight Heparins. 119 of them were patients with risky pregnancy and 68 were with the diagnosis Hypercoagulable State. Keywords: Antithrombotics, Deep Vein Thrombosis, Pregnancy, Low Molecular Weight Heparins. Abrevations LMWH Low molecular weight heparins VT venous thromboembolism 1. INTRODUCTION There are two main adverse expriences that are associated with thrombophilia and pregnancy. These are VT and pregnancy complications associated with placental infarction, including miscarriage, intrauterine growth restriction, preeclampsia, abruption, and intrauterine death [1]. -
Fragmin Injection (Dalteparin Sodium)
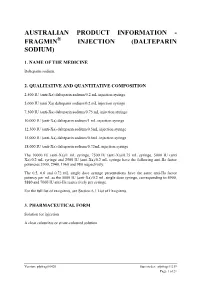
AUSTRALIAN PRODUCT INFORMATION - FRAGMIN® INJECTION (DALTEPARIN SODIUM) 1. NAME OF THE MEDICINE Dalteparin sodium. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 2,500 IU (anti-Xa) dalteparin sodium/0.2 mL injection syringe 5,000 IU (anti Xa) dalteparin sodium/0.2 mL injection syringe 7,500 IU (anti-Xa) dalteparin sodium/0.75 mL injection syringe 10,000 IU (anti-Xa) dalteparin sodium/1 mL injection syringe 12,500 IU (anti-Xa) dalteparin sodium/0.5mL injection syringe 15,000 IU (anti-Xa) dalteparin sodium/0.6mL injection syringe 18,000 IU (anti-Xa) dalteparin sodium/0.72mL injection syringe The 10000 IU (anti-Xa)/1 mL syringe, 7500 IU (anti-Xa)/0.75 mL syringe, 5000 IU (anti Xa)/0.2 mL syringe and 2500 IU (anti-Xa)/0.2 mL syringe have the following anti-IIa factor potencies 3900, 2940, 1960 and 980 respectively. The 0.5, 0.6 and 0.72 mL single dose syringe presentations have the same anti-IIa factor potency per mL as the 5000 IU (anti-Xa)/0.2 mL single dose syringe, corresponding to 4900, 5880 and 7060 IU anti-IIa respectively per syringe. For the full list of excipients, see Section 6.1 List of Excipients. 3. PHARMACEUTICAL FORM Solution for injection A clear colourless or straw-coloured solution. Version: pfpfragi10420 Supersedes: pfpfragi11219 Page 1 of 21 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications Prophylaxis against thrombotic complications during haemodialysis and treatment of acute deep vein thrombosis (DVT). Extended treatment of symptomatic venous thromboembolism (VTE) (proximal deep vein thrombosis and/or pulmonary embolism) to reduce the recurrence of VTE in patients with solid tumour cancers. -

Low-Molecular-Weight Heparins in the Treatment of Acute Coronary Syndromes
REVIEW ARTICLE Low-Molecular-Weight Heparins in the Treatment of Acute Coronary Syndromes Alexander G. G. Turpie, MD; Elliott M. Antman, MD latelet aggregation and activation of coagulation are key events in the development of acute coronary syndromes. Patients with an acute coronary syndrome are at high risk of death or myocardial infarction, and hence there is a strong rationale for the use of antithrombotic agents. Heparin has been shown to reduce the risk of death or myocar- Pdial infarction in aspirin-treated patients with acute coronary syndromes, but it has a number of limitations, including the need for regular monitoring and the risk of hemorrhage and thrombo- cytopenia. Low-molecular-weight heparins offer a number of practical and clinical advantages over unfractionated heparin, such as higher bioavailability and administration by subcutaneous injec- tion. Several low-molecular-weight heparins are available that differ in their biochemical and phar- macologic properties, and it is not possible to predict their clinical efficacy from their pharmaco- logic profile. The decision regarding the use of a specific low-molecular-weight heparin should be based on the efficacy and safety data available for each product. In clinical trials comparing low- molecular-weight heparin with heparin, only enoxaparin sodium has been shown to reduce the risk of coronary events in patients with non–ST segment elevation acute coronary ischemia. Arch Intern Med. 2001;161:1484-1490 Clinical and pathologic studies have high- gina and non–Q wave MI indicates that the lighted the importance of plaque rupture culprit artery is only partially or intermit- and platelet aggregation in the pathogen- tently occluded or that a rich collateral cir- esis of the acute coronary syndromes (ACS) culation exists. -

Review of Medical Therapies for the Management of Pulmonary Embolism
medicina Review Review of Medical Therapies for the Management of Pulmonary Embolism Ladan Panahi *, George Udeani * , Michael Horseman, Jaye Weston, Nephy Samuel, Merlyn Joseph , Andrea Mora and Daniela Bazan Department of Pharmacy Practice, Texas A&M Rangel College of Pharmacy, 1010 W Ave B, Kingsville, TX 78363, USA; [email protected] (M.H.); [email protected] (J.W.); [email protected] (N.S.); [email protected] (M.J.); [email protected] (A.M.); [email protected] (D.B.) * Correspondence: [email protected] (L.P.); [email protected] (G.U.) Abstract: Traditionally, the management of patients with pulmonary embolism has been accom- plished with anticoagulant treatment with parenteral heparins and oral vitamin K antagonists. Although the administration of heparins and oral vitamin K antagonists still plays a role in pul- monary embolism management, the use of these therapies are limited due to other options now available. This is due to their toxicity profile, clearance limitations, and many interactions with other medications and nutrients. The emergence of direct oral anticoagulation therapies has led to more options now being available to manage pulmonary embolism in inpatient and outpatient settings conveniently. These oral therapeutic options have opened up opportunities for safe and effective pulmonary embolism management, as more evidence and research is now available about reversal agents and monitoring parameters. The evolution of the pharmacological management of pulmonary embolism has provided us with better understanding regarding the selection of anticoagulants. There is also a better understanding and employment of anticoagulants in pulmonary embolism in special Citation: Panahi, L.; Udeani, G.; populations, such as patients with liver failure, renal failure, malignancy, and COVID-19. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Utah Medicaid Pharmacy and Therapeutics Committee Drug
Utah Medicaid Pharmacy and Therapeutics Committee Drug Class Review Non-Vitamin K Anticoagulants for Venous Thromboembolism and Nonvalvular Atrial Fibrillation Direct Thrombin Inhibitors Dabigatran (Pradaxa, generic) Desirudin (Iprivask) Direct Factor Xa Inhibitors Apixaban (Eliquis) Betrixaban (Bevyxxa) Edoxaban (Savaysa) Fondaparinux (Arixtra) Rivaroxaban (Xarelto) Low Molecular Weight Heparins Dalteparin (Fragmin, generic) Enoxaparin (Lovenox, generic) AHFS Classification: 20:12.04.12 Direct Thrombin Inhibitors, 20:12.04.14 Direct Factor Xa Inhibitors, 20:12.04.16 Heparins Final Report October 2018 Review prepared by: Elena Martinez Alonso, B.Pharm., MSc MTSI, Medical Writer Valerie Gonzales, Pharm.D., Clinical Pharmacist Vicki Frydrych, B.Pharm., Pharm.D., Clinical Pharmacist Lauren Heath, Pharm.D., MS, BCACP, Assistant Professor (Clinical) Michelle Fiander, MA, MLIS, Research Assistant Professor, Evidence Synthesis Librarian Joanne LaFleur, PharmD, MSPH, Associate Professor University of Utah College of Pharmacy University of Utah College of Pharmacy, Drug Regimen Review Center Copyright © 2018 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved Contents Executive Summary ........................................................................................................................ 3 Introduction ..................................................................................................................................... 7 Table 1. FDA-Approved Indications for Non-Vitamin K Anticoagulants