Walsall / Dudley Mental Health Partnership
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contacts: T Becoming More Active
KEY National Cycle Route Existing cycle routes and safer routes to school On road cycle facilities rrss and bus lanes AA SSttaa Canal towpath Cycle stands Pedestrian area Walsall Walk On Health Walks Local Programme Town Centre Map Groups TO BROWNHILLS A454 TO ALDRIDGE & A34 TO BLOXWICH/ A461 TO BROWNHILLS CANNOCK TO ALDRIDGE Active Sustainable Travel TO Da & LICHFIELD Gr y WALSALL Str REEDSWOOD een ee t COLLEGE L an POLICE ARBORETUM e STATION And Road Safety Walking is Not sure where to start? Joining a group LAW LEATHER MUSEUM COURTS treet Littleton S one of the best is a great way of discovering new routes A4148 The A*STARS programme looks at promoting Wi llen A4148 TO h sustainable travel on the school journey and during and improving your skills and fitness with al st St t l C e y af t e BIRMINGHAM/ cle We Rout e ford n ee Str e La tr ld M6 J7 & J9 the school day. It also develops opportunities for e St and easiest ways of S the help of more experienced people. TO WILLENHALL u fie Bl on re rt Lich et training and new initiatives, such as walking bus he Here are a few useful contacts: t becoming more active. Supermarket Ha schemes. After a successful pilot, the programme is Supermarket now being rolled-out across all Walsall schools d CIVIC Walking regularly can: CTC Walsall Member Group a BATHS Ro CENTRE Pilot project achievements (2010-2012): n to LIBRARY Wol er verhampton POST (Cyclists’ Touring Club) Street Hath In OFFICE to • Help weight loss A454 TO WILLENHALL/ wn 3% increase in walking and cycling levels in R WOLVERHAMPTON M6 J10 WALSALL CANAL ART ow Contact: 01543 377145 BASIN GALLERY COUNCIL A*STARS schools, compared to an overall Walsall THE • Ease back pain Butlers HOUSE [email protected] Passage CROSSING t average of 1.8% e e r Pa t S rk l www.chasecycling.co.uk l • Reduce the risks of heart disease St re Br ha i s 3.7% reduction in single car use. -

West Midlands European Regional Development Fund Operational Programme
Regional Competitiveness and Employment Objective 2007 – 2013 West Midlands European Regional Development Fund Operational Programme Version 3 July 2012 CONTENTS 1 EXECUTIVE SUMMARY 1 – 5 2a SOCIO-ECONOMIC ANALYSIS - ORIGINAL 2.1 Summary of Eligible Area - Strengths and Challenges 6 – 14 2.2 Employment 15 – 19 2.3 Competition 20 – 27 2.4 Enterprise 28 – 32 2.5 Innovation 33 – 37 2.6 Investment 38 – 42 2.7 Skills 43 – 47 2.8 Environment and Attractiveness 48 – 50 2.9 Rural 51 – 54 2.10 Urban 55 – 58 2.11 Lessons Learnt 59 – 64 2.12 SWOT Analysis 65 – 70 2b SOCIO-ECONOMIC ANALYSIS – UPDATED 2010 2.1 Summary of Eligible Area - Strengths and Challenges 71 – 83 2.2 Employment 83 – 87 2.3 Competition 88 – 95 2.4 Enterprise 96 – 100 2.5 Innovation 101 – 105 2.6 Investment 106 – 111 2.7 Skills 112 – 119 2.8 Environment and Attractiveness 120 – 122 2.9 Rural 123 – 126 2.10 Urban 127 – 130 2.11 Lessons Learnt 131 – 136 2.12 SWOT Analysis 137 - 142 3 STRATEGY 3.1 Challenges 143 - 145 3.2 Policy Context 145 - 149 3.3 Priorities for Action 150 - 164 3.4 Process for Chosen Strategy 165 3.5 Alignment with the Main Strategies of the West 165 - 166 Midlands 3.6 Development of the West Midlands Economic 166 Strategy 3.7 Strategic Environmental Assessment 166 - 167 3.8 Lisbon Earmarking 167 3.9 Lisbon Agenda and the Lisbon National Reform 167 Programme 3.10 Partnership Involvement 167 3.11 Additionality 167 - 168 4 PRIORITY AXES Priority 1 – Promoting Innovation and Research and Development 4.1 Rationale and Objective 169 - 170 4.2 Description of Activities -

West Midlands Police Freedom of Information 10/02/2021
West Midlands Police Freedom of Information (1) From 1st January 2019-2020 to date how many people in total have sat as members on Independent Advisory groups (IAG) I would like the number of people who have sat for the while time period requested (If you are able to break this down into individual meeting within that time period that would be useful too) SOLIHULL - 18 COVENTRY - 75 BHAM EAST - We have 2 IAG’s on BE (previously Birmingham North & Birmingham East). Both meet quarterly. B’ham North attendees is 35 in 2019 and 36 in 2020. B’ham East 37 and 33 BHAM WEST – B’ham South Have 11 IAG members although not all have attended the IAGs and generally around 5 will attend the meetings. B’ham West Have 12 IAG members we are unable to say how many have previously attended WOLVERHAMPTON – At Wolverhampton there are 18 members who sat on the IAG throughout this time period DUDLEY - 27 as of October 2020 SANDWELL - 14 members in total WALSALL – Walsall NPU don’t have an IAG they have an SCRG (Strategic Community Reference Group) of which there are 31 members (2) From 1st January 2019-2020 to date how many people of South Asian ethnicity have sat as members on Independent Advisory groups (IAG) I would like to know people who have confirmed their ethnicity. If this data is not available then I would like to know the number of members who appear to be of South Asian ethnicity. SOLIHULL – None COVENTRY - 28 Asian in total – we don’t have a breakdown of South Asian BHAM EAST - We do not ask our attendees to identify themselves by ethnicity or religion. -
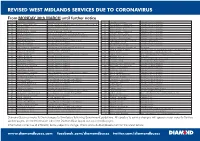
Revised West Midlands Services Due To
REVISED WEST MIDLANDS SERVICES DUE TO CORONAVIRUS From MONDAY 30th MARCH until further notice 1 Chaplefields - Walsgrave Saturday Service in Operation 61 Perry Barr - Hamstead Saturday Service in Operation 002 Weoley Castle - Merry Hill Special Timetable in Operation every 30mins / Normal Sun Service 63 Wolverhampton - Oxbarn Ave Saturday Service in Operation A1 Solihull Circular Saturday Service in Operation 64 West Bromwich - Wednesbury Saturday Service in Operation A2 Solihull Circular Saturday Service in Operation 64 Wolverhampton - Penn Saturday Service in Operation 4 West Bromwich - Walsall Service Suspended - Refer to 4H 65 Wolverhampton - Fordhouses Saturday Service in Operation 4H Walsall - Hayley Green Revised Special Timetable every 30 min Mon-Sat 65 Darlaston - Woods Estate Saturday Service in Operation 13 Merry Hill - Halesowen Mon - Sat Saturday Service / Normal Service Sundays 66 West Bromwich - Stone Cross Saturday Service in Operation 15 Tamworth - Hurley Saturday Service in Operation 68A|68C Perry Barr - Aston Six Ways Saturday Service in Operation 16 Birmingham - Hamstead Service Suspended Mon - Sat - Refer to 16W 71 Chelmsley Wood - Sutton Coldfield Normal Sunday Service T16 Tamworth - Kingsbury Saturday Service in Operation 74 Gillity Village - Walsall Saturday Service in Operation 16A Tamworth - Kingsbury Saturday Service in Operation 74A West Bromwich - Dudley Saturday Service in Operation 16W West Bromwich - Birmingham Revised Special Timetable every 30 min Mon-Sat 75 B’ham International - Business Park No Service -

The Black Country David Horovitz (Pp
JOURNAL OF THE ENGLISH PLACE-NAME SOCIETY Volume 43 (2011) ISSN 1351–3095 ______________________________________________________________ The Black Country David Horovitz (pp. 25–34) ______________________________________________________________ This article is from the Journal of the English Place-Name Society, an annual peer-reviewed journal issued free to members of the Society. The Journal welcomes contributions of articles and notes on subjects of relevance to English place-names. The English Place-Name Society (EPNS) was established in 1923 to conduct a county-by-county survey of the place-names of England. To date, the Survey has produced 90 volumes. Almost all English counties have been surveyed, at least in part, and work to complete the Survey is ongoing. The Survey is used by researchers, academics, and those interested in the origins, meaning, and significance of English place-names. The research work and the publication of the Survey are financed by the annual subscriptions of members of the Society, with the help of grants from the Arts and Humanities Research Council and the British Academy. Since the progress and success of the Survey depend largely upon the strength of the membership, the Society always welcomes new members, both personal and institutional. In return for the annual subscription, members receive free of charge the current issue of the Journal as well as the volume of the Survey allocated to that year’s subscription. They are entitled to order, in addition, any available volume of the Survey at a concessionary price. Associate Members pay a reduced subscription, for which they receive the Journal. Annual subscription prices (correct as of April 2017): Within the UK Outside the UK £40 (full) £45 (full)* £15 (associate) £18 (associate* *increased prices reflect increased postage cost. -

Merry Hill Via Wednesbury, Dudley
11 Walsall - Merry Hill via Wednesbury, Dudley Mondays to Fridays Operator: NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB Newport Street (Stop X) 0524 0554 0624 0649 0709 0729 0749 0809 0829 0849 0909 0936 0956 1016 1036 1056 1116 1136 King’s Hill, Wood Green High School (adj) 0530 0600 0630 0657 0717 0738 0758 0818 0838 0858 0918 0945 1005 1025 1045 1105 1125 1145 Wednesbury, Wednesbury Bus Station (Stand ARR0537 0607 0637 0704 0724 0747 0807 0827 0847 0907 0927 0952 1012 1032 1052 1112 1132 1152 J) Wednesbury, Wednesbury Bus Station (Stand DEP0539 0609 0639 0705 0725 0748 0808 0828 0848 0908 0928 0953 1013 1033 1053 1113 1133 1153 J) Princes End, Princes End Post Office (opp) 0551 0621 0652 0719 0740 0803 0823 0843 0903 0923 0943 1006 1026 1046 1106 1126 1146 1206 Dudley Bus Station (Stand J) ARR0603 0633 0705 0732 0756 0819 0839 0859 0916 0936 0956 1019 1039 1059 1119 1139 1159 1219 Dudley, Dudley Bus Station (Stand J) DEP 0801 0904 1004 1104 1204 Netherton, Church Road (opp) 0811 0913 1013 1113 1213 Merry Hill Bus Station 0826 0927 1027 1127 1227 Mondays to Fridays Operator: NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB NXB Newport Street (Stop X) 1156 1216 1236 1256 1316 1336 1356 1416 1436 1456 1512 1532 1552 1612 1632 1652 1712 1732 King’s Hill, Wood Green High School (adj) 1205 1225 1245 1305 1325 1345 1405 1425 1445 1505 1521 1541 1601 1621 1641 1701 1721 1741 Wednesbury, Wednesbury Bus Station (Stand ARR1212 1232 1252 1312 1332 1352 1412 1432 1452 1512 1530 1550 1610 1630 1650 1710 -

Walsall Mental Health Information Hub
Black Country Service Directory Crisis Factsheets Suicide Prevention Healthcare Walsall Mental Health Information Hub Covid-19 Information Hub Black Country Service Directory Crisis Factsheets Suicide Prevention Healthcare Accord Outreach Aldridge Men’s Asian Ladies Aaina Hub Age Matters Service Directory Service Shed Group Blue Hearts Caldmore Asian Men’s Bereavement Black Country Black Country Caldmore Group Emotional Support Bereavement Community Help point Helpline Women’s Aid Support Group Garden Men’s Shed Calm Space Community Expert Patient Friendship Friendship Camden Street Family Matters peer support Perinatal Service Programme Group Pelsall Group Walsall Health Watch Making Mind Matters Pathways for Glebe Centre Lonsdale House My Time Active Walsall Connections Cafe life Suicide Walsall IPS Walsall St Paul’s Think Again Peer Sanctuary Hub Bereavement Employment Bereavement SilverCloud Support Group Support Group support group Service Services Walsall Walsall Black Walsall Link WHG Wellbeing WHG Wellbeing WPH Enablement & Walsall M.A.D Sisters Collective Homes Service Counselling Recovery Service Line Black Country Service Directory Crisis Factsheets Suicide Prevention Healthcare Crisis Suicidal thoughts Are you worried Are you supporting Are you experiencing someone who is Are you in crisis? No about your suicidal thoughts experiencing suicidal mental health thoughts Yes Yes Yes Yes Click for Click for Click for information information information Click for information Click for helpline Click for helpline information information Black Country Service Directory Crisis Factsheets Suicide Prevention Healthcare Who to contact if you need urgent support, If you feel suicidal or feel like harming yourself: • Contact The Sanctuary Hub – during the opening times • Go to your nearest Accident and Emergency department (A&E). -

13 Pensnett to Oldbury Route
L CHF ELD STAFFORDSH RE WALSALL WOLVERHAMPTON WEST BROMW CH West Midlands Key Route Network DUDLEY Pensnett to Oldbury Route BRMNGHAM WARW CKSH RE WORCESTERSH RE SOL HULL COVENTRY Figure 1 12 A5 A38, A38(M), A47, A435, A441, A4400, A4540, A5127, B4138, M6 L CHF ELD Birmingham West Midlands Cross City B4144, B4145, B4148, B4154 11a Birmingham Outer Circle A4030, A4040, B4145, B4146 Key Route Network A5 11 Birmingham to Stafford A34 Black Country Route A454(W), A463, A4444 3 2 1 M6 Toll BROWNH LLS Black Country to Birmingham A41 M54 A5 10a Coventry to Birmingham A45, A4114(N), B4106 A4124 A452 East of Coventry A428, A4082, A4600, B4082 STAFFORDSH RE East of Walsall A454(E), B4151, B4152 OXLEY A449 M6 A461 Kingswinford to Halesowen A459, A4101 A38 WEDNESF ELD A34 Lichfield to Wednesbury A461, A4148 A41 A460 North and South Coventry A429, A444, A4053, A4114(S), B4098, B4110, B4113 A4124 A462 A454 Northfield to Wolverhampton A4123, B4121 10 WALSALL A454 A454 Pensnett to Oldbury A461, A4034, A4100, B4179 WOLVERHAMPTON Sedgley to Birmingham A457, A4030, A4033, A4034, A4092, A4182, A4252, B4125, B4135 SUTTON T3 Solihull to Birmingham A34(S), A41, A4167, B4145 A4038 A4148 COLDF ELD PENN B LSTON 9 A449 Stourbridge to Wednesbury A461, A4036, A4037, A4098 A4123 M6 Stourbridge to A449, A460, A491 A463 8 7 WEDNESBURY M6 Toll North of Wolverhampton A4041 A452 A5127 UK Central to Brownhills A452 WEST M42 A4031 9 A4037 BROMW CH K NGSTAND NG West Bromwich Route A4031, A4041 A34 GREAT BARR M6 SEDGLEY West of Birmingham A456, A458, B4124 A459 M5 A38 -

Dissolution of West Midlands Joint Committee
Agenda item 8 Cabinet – 25 April, 2018 Dissolution of West Midlands Joint Committee Portfolio: Councillor Sean Coughlan, Leader of the Council Related portfolios: None Service: All Wards: All Key decision: No Forward plan: No 1. Summary 1.1 A review has been undertaken of the role and function of the West Midlands Joint Committee (WMJC), which was setup in 1985 arising out of the dissolution of the West Midlands County Council. The review determined that the West Midlands Joint Committee is no longer an effective vehicle as most of its functions are now redundant at the Joint Committee for the purposes of the seven West Midlands Councils business. It was determined the remaining main function being matter relating to the Birmingham Airport, of which the seven West Midlands Councils are shareholders, can be more effectively dealt with by establishing a new Joint Committee solely for that purpose. 1.2 This report seeks authority from Cabinet to recommend to Full Council that the West Midlands Joint Committee (“WMJC” or the “Committee”) be dissolved and the new arrangements for managing the remaining residual business of the Committee once the Committee is dissolved. In addition, it seeks Cabinet approval to establish a Joint Executive Committee with the other six Councils within the West Midlands for the purpose of airport decisions known as West Midlands Shareholders Airport Committee. 2. Recommendations 2.1 That Cabinet recommends to Council to approve:- (i) the dissolution of the West Midlands Joint Committee, for the reasons set out in this report; (ii) the proposals for managing the remaining residual business of the WMJCs once it is dissolved as set out in Appendix 1 of this report. -

Streetly January 2020 Version - FINAL Councillors
Ward Walk Profile: Streetly January 2020 Version - FINAL Councillors Name Party Elected on: Cllr Brian Douglas- Conservatives 13 November 1980 Maul Cllr Sat Johal Conservatives 2 May 2019 Cllr Suky Samra Conservatives 3 May 2018 Geography . Covers 5.83 sq km (583 ha) . Makes up 5.6% of the area of Walsall borough . Population density of 23.4 people per hectare (lower than borough average of 27.3) Source: Ordnance Survey; ONS, Mid-2018 Population Estimates Assets Source: Ordnance Survey Population Source: ONS, Mid-2018 Population Estimates Ethnicity . 14% minority ethnic residents . Asian is the largest minority group at 8.9% (on par with Walsall average of 15.2%) . Of the Asian minority group, Indian is the most prolific at 6.1% Source: ONS, 2011 Census Housing Composition Tenure . 5,710 households (with at least 1 usual resident) . Increase of 12.6% since 2001 (Proportion of borough total 5.3%) . Average household size: 2.4 residents per h/hold (similar to Walsall average of 2.5) . 2.3% of households ‘overcrowded’* (Walsall average 6.5%) . 1.4% of households without central heating (Walsall average 2.8%) . Low proportion of socially rented (1.6%) properties compared to borough (24.1%) . Above average (31.9%) mortgage owned Source: ONS, 2011 Census (41.6%) Social Segmentation - Groups The largest groups of households are classified as group B – Prestige Positions (29%) & group F – Senior Security (26%) Most effective communication route Least effective communication routes Source: Experian - Mosaic Public Sector Profiler 2019; Ordnance Survey LLPG Address file Economic Summary • 82.6% of working age people in Streetly ward were economically active. -

217 Walsall Road, Sutton Coldfield, West Midlands, B74 4QA
217 Walsall Road, Sutton Coldfield, West Midlands, B74 4QA This imposing detached residence offers the discerning purchaser a rare opportunity to acquire a substantial and well balanced family home which enjoys sympathetic two storey side and single storey rear extensions. Comfortable and truly spacious, this beautiful home offers character and charm with internal inspection essential and highly recommended. Attractive from the kerb, the property stands well back from the roadway behind substantial fore gardens with a wide sweeping driveway providing substantial off street parking and servicing an exceptional four car integral garage. Occupying a highly regarded residential location within Four Oaks, all amenities are close at hand. Comprehensive local shops are located nearby with access to Mere Green centre only a few minutes drive away. Sutton Park is on the doorstep and provides 2400 acres of unspoilt park and woodland and the area Is well served by sought after schools including Arthur Terry Secondary School (clients should check catchment criteria as this can vary ). For commuters, Blake Street railway station provides ease of access to Birmingham, Sutton Coldfield and Lichfield. Well maintained and tastefully presented throughout, the accommodation briefly comprises; Feature canopy porch entrance, attractive reception hallway with feature glazed entrance door and side panels with leaded light and stained glass inserts, ceiling cornice and display alcove further complimented by a guest cloakroom/WC. The sitting room is a charming room with a tall bay window facing the front elevation, a modern marble fireplace surround forms a focal point with living flame electric convector fire, attractive original ceiling cornice with centre ceiling roses and decorative archway opening to a formal dining room, a light and airy space ideal for entertaining with tall double glazed bay window to front and additional windows to side, fireplace recess with conglomerate marble hearth, original ceiling cornice with decorative ceiling rose. -

Update on Stroke Reconfiguration Programme – Birmingham, Solihull and Black Country
Item 6 Appendix 1 Update on Stroke Reconfiguration Programme – Birmingham, Solihull and Black Country 1. Purpose To provide an overview of the Birmingham, Solihull and Black Country Stroke reconfiguration Programme. The programme aims to draw together work undertaken to date by the Midlands and East Stroke Review and seeks to understand if there is a need to reconfigure local stroke services to deliver better patient outcomes. 2. Context : In 2010, the West Midlands Regional Quality Review Service led a review process in co-ordination with the West Midlands Cardiac and Stroke Networks. The purpose of the review was to assess compliance with the WMQRS (West Midlands Quality Review Service) quality standards for acute stroke and Transient Ischaemic Attacks (TIA) and to train future reviewers. The review team included a Stroke Consultant, Stroke Nurse, an Allied Health Professional and members of WMQRS and the Stroke Network. The process consisted of site visits and discussions with a multidisciplinary team. The outputs of the assessment process were used to inform the quality of care that was being delivered by each provider and to assess the capability of providers to deliver 24/7 thrombolysis and other stroke services. The review process showed that there was significant variation in the quality of care that isprovided across the region. The West Midlands Strategic Health Authority was still concerned about the model / configuration for stroke services in the region. In January 2012 the NHS across the Midlands and East approved a clinically led comprehensive review of stroke across the region, to identify options that would improve outcomes by improving mortality, reduce chances of long term disability and improve patient experience.