F IDENTIFICATION of AMYOTROPHIC LATERAL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Information
Supplementary Information This text file includes: Supplementary Methods Supplementary Figure 1-13, 15-30 Supplementary Table 1-8, 16, 20-21, 23, 25-37, 40-41 1 1. Samples, DNA extraction and genome sequencing 1.1 Ethical statements and sample storage The ethical statements of collecting and processing tissue samples for each species are listed as follows: Myotis myotis: All procedures were carried out in accordance with the ethical guidelines and permits (AREC-13-38-Teeling) delivered by the University College Dublin and the Préfet du Morbihan, awarded to Emma Teeling and Sébastien Puechmaille respectively. A single M. myotis individual was humanely sacrificed given that she had lethal injuries, and dissected. Rhinolophus ferrumequinum: All the procedures were conducted under the license (Natural England 2016-25216-SCI-SCI) issued to Gareth Jones. The individual bat died unexpectedly and suddenly during sampling and was dissected immediately. Pipistrellus kuhlii: The sampling procedure was carried out following all the applicable national guidelines for the care and use of animals. Sampling was done in accordance with all the relevant wildlife legislation and approved by the Ministry of Environment (Ministero della Tutela del Territorio e del Mare, Aut.Prot. N˚: 13040, 26/03/2014). Molossus molossus: All sampling methods were approved by the Ministerio de Ambiente de Panamá (SE/A-29-18) and by the Institutional Animal Care and Use Committee of the Smithsonian Tropical Research Institute (2017-0815-2020). Phyllostomus discolor: P. discolor bats originated from a breeding colony in the Department Biology II of the Ludwig-Maximilians-University in Munich. Approval to keep and breed the bats was issued by the Munich district veterinary office. -
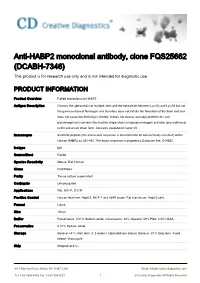
Anti-HABP2 Monoclonal Antibody, Clone FQS25662 (DCABH-7346) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-HABP2 monoclonal antibody, clone FQS25662 (DCABH-7346) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to HABP2 Antigen Description Cleaves the alpha-chain at multiple sites and the beta-chain between Lys-53 and Lys-54 but not the gamma-chain of fibrinogen and therefore does not initiate the formation of the fibrin clot and does not cause the fibrinolysis directly. It does not cleave (activate) prothrombin and plasminogen but converts the inactive single chain urinary plasminogen activator (pro-urokinase) to the active two chain form. Activates coagulation factor VII. Immunogen Synthetic peptide (the amino acid sequence is considered to be commercially sensitive) within Human HABP2 aa 350-450. The exact sequence is proprietary.Database link: Q14520 Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Rat, Human Clone FQS25662 Purity Tissue culture supernatant Conjugate Unconjugated Applications WB, IHC-P, ICC/IF Positive Control Human fetal liver, HepG2, MCF-7 and A549 lysate. Rat liver tissue. HepG2 cells. Format Liquid Size 100 μl Buffer Preservative: 0.01% Sodium azide; Constituents: 40% Glycerol, 59% PBS, 0.05% BSA Preservative 0.01% Sodium Azide Storage Store at +4°C short term (1-2 weeks). Upon delivery aliquot. Store at -20°C long term. Avoid freeze / thaw cycle. Ship Shipped at 4°C. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved -

Whole Exome Sequencing in Families at High Risk for Hodgkin Lymphoma: Identification of a Predisposing Mutation in the KDR Gene
Hodgkin Lymphoma SUPPLEMENTARY APPENDIX Whole exome sequencing in families at high risk for Hodgkin lymphoma: identification of a predisposing mutation in the KDR gene Melissa Rotunno, 1 Mary L. McMaster, 1 Joseph Boland, 2 Sara Bass, 2 Xijun Zhang, 2 Laurie Burdett, 2 Belynda Hicks, 2 Sarangan Ravichandran, 3 Brian T. Luke, 3 Meredith Yeager, 2 Laura Fontaine, 4 Paula L. Hyland, 1 Alisa M. Goldstein, 1 NCI DCEG Cancer Sequencing Working Group, NCI DCEG Cancer Genomics Research Laboratory, Stephen J. Chanock, 5 Neil E. Caporaso, 1 Margaret A. Tucker, 6 and Lynn R. Goldin 1 1Genetic Epidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 2Cancer Genomics Research Laboratory, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 3Ad - vanced Biomedical Computing Center, Leidos Biomedical Research Inc.; Frederick National Laboratory for Cancer Research, Frederick, MD; 4Westat, Inc., Rockville MD; 5Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; and 6Human Genetics Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD, USA ©2016 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol.2015.135475 Received: August 19, 2015. Accepted: January 7, 2016. Pre-published: June 13, 2016. Correspondence: [email protected] Supplemental Author Information: NCI DCEG Cancer Sequencing Working Group: Mark H. Greene, Allan Hildesheim, Nan Hu, Maria Theresa Landi, Jennifer Loud, Phuong Mai, Lisa Mirabello, Lindsay Morton, Dilys Parry, Anand Pathak, Douglas R. Stewart, Philip R. Taylor, Geoffrey S. Tobias, Xiaohong R. Yang, Guoqin Yu NCI DCEG Cancer Genomics Research Laboratory: Salma Chowdhury, Michael Cullen, Casey Dagnall, Herbert Higson, Amy A. -

Mouse Cadm3 Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Cadm3 Knockout Project (CRISPR/Cas9) Objective: To create a Cadm3 knockout Mouse model (C57BL/6N) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Cadm3 gene (NCBI Reference Sequence: NM_053199 ; Ensembl: ENSMUSG00000005338 ) is located on Mouse chromosome 1. 9 exons are identified, with the ATG start codon in exon 1 and the TAG stop codon in exon 9 (Transcript: ENSMUST00000111220). Exon 2~6 will be selected as target site. Cas9 and gRNA will be co-injected into fertilized eggs for KO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Mice homozygous for a null allele exhibit delayed myelination. Other mice with ubiquitous conditional deletion of the gene do not display neurological abnormalities. Exon 2 starts from about 6.99% of the coding region. Exon 2~6 covers 58.42% of the coding region. The size of effective KO region: ~4894 bp. The KO region does not have any other known gene. Page 1 of 8 https://www.alphaknockout.com Overview of the Targeting Strategy Wildtype allele 5' gRNA region gRNA region 3' 1 2 3 4 5 6 9 Legends Exon of mouse Cadm3 Knockout region Page 2 of 8 https://www.alphaknockout.com Overview of the Dot Plot (up) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 2000 bp section upstream of Exon 2 is aligned with itself to determine if there are tandem repeats. Tandem repeats are found in the dot plot matrix. The gRNA site is selected outside of these tandem repeats. Overview of the Dot Plot (down) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 445 bp section downstream of Exon 6 is aligned with itself to determine if there are tandem repeats. -

Nº Ref Uniprot Proteína Péptidos Identificados Por MS/MS 1 P01024
Document downloaded from http://www.elsevier.es, day 26/09/2021. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. Nº Ref Uniprot Proteína Péptidos identificados 1 P01024 CO3_HUMAN Complement C3 OS=Homo sapiens GN=C3 PE=1 SV=2 por 162MS/MS 2 P02751 FINC_HUMAN Fibronectin OS=Homo sapiens GN=FN1 PE=1 SV=4 131 3 P01023 A2MG_HUMAN Alpha-2-macroglobulin OS=Homo sapiens GN=A2M PE=1 SV=3 128 4 P0C0L4 CO4A_HUMAN Complement C4-A OS=Homo sapiens GN=C4A PE=1 SV=1 95 5 P04275 VWF_HUMAN von Willebrand factor OS=Homo sapiens GN=VWF PE=1 SV=4 81 6 P02675 FIBB_HUMAN Fibrinogen beta chain OS=Homo sapiens GN=FGB PE=1 SV=2 78 7 P01031 CO5_HUMAN Complement C5 OS=Homo sapiens GN=C5 PE=1 SV=4 66 8 P02768 ALBU_HUMAN Serum albumin OS=Homo sapiens GN=ALB PE=1 SV=2 66 9 P00450 CERU_HUMAN Ceruloplasmin OS=Homo sapiens GN=CP PE=1 SV=1 64 10 P02671 FIBA_HUMAN Fibrinogen alpha chain OS=Homo sapiens GN=FGA PE=1 SV=2 58 11 P08603 CFAH_HUMAN Complement factor H OS=Homo sapiens GN=CFH PE=1 SV=4 56 12 P02787 TRFE_HUMAN Serotransferrin OS=Homo sapiens GN=TF PE=1 SV=3 54 13 P00747 PLMN_HUMAN Plasminogen OS=Homo sapiens GN=PLG PE=1 SV=2 48 14 P02679 FIBG_HUMAN Fibrinogen gamma chain OS=Homo sapiens GN=FGG PE=1 SV=3 47 15 P01871 IGHM_HUMAN Ig mu chain C region OS=Homo sapiens GN=IGHM PE=1 SV=3 41 16 P04003 C4BPA_HUMAN C4b-binding protein alpha chain OS=Homo sapiens GN=C4BPA PE=1 SV=2 37 17 Q9Y6R7 FCGBP_HUMAN IgGFc-binding protein OS=Homo sapiens GN=FCGBP PE=1 SV=3 30 18 O43866 CD5L_HUMAN CD5 antigen-like OS=Homo -

Genetic and Functional Approaches to Understanding Autoimmune and Inflammatory Pathologies
University of Vermont ScholarWorks @ UVM Graduate College Dissertations and Theses Dissertations and Theses 2020 Genetic And Functional Approaches To Understanding Autoimmune And Inflammatory Pathologies Abbas Raza University of Vermont Follow this and additional works at: https://scholarworks.uvm.edu/graddis Part of the Genetics and Genomics Commons, Immunology and Infectious Disease Commons, and the Pathology Commons Recommended Citation Raza, Abbas, "Genetic And Functional Approaches To Understanding Autoimmune And Inflammatory Pathologies" (2020). Graduate College Dissertations and Theses. 1175. https://scholarworks.uvm.edu/graddis/1175 This Dissertation is brought to you for free and open access by the Dissertations and Theses at ScholarWorks @ UVM. It has been accepted for inclusion in Graduate College Dissertations and Theses by an authorized administrator of ScholarWorks @ UVM. For more information, please contact [email protected]. GENETIC AND FUNCTIONAL APPROACHES TO UNDERSTANDING AUTOIMMUNE AND INFLAMMATORY PATHOLOGIES A Dissertation Presented by Abbas Raza to The Faculty of the Graduate College of The University of Vermont In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Specializing in Cellular, Molecular, and Biomedical Sciences January, 2020 Defense Date: August 30, 2019 Dissertation Examination Committee: Cory Teuscher, Ph.D., Advisor Jonathan Boyson, Ph.D., Chairperson Matthew Poynter, Ph.D. Ralph Budd, M.D. Dawei Li, Ph.D. Dimitry Krementsov, Ph.D. Cynthia J. Forehand, Ph.D., Dean of the Graduate College ABSTRACT Our understanding of genetic predisposition to inflammatory and autoimmune diseases has been enhanced by large scale quantitative trait loci (QTL) linkage mapping and genome-wide association studies (GWAS). However, the resolution and interpretation of QTL linkage mapping or GWAS findings are limited. -

Current Knowledge of Germline Genetic Risk Factors for the Development of Non-Medullary Thyroid Cancer
G C A T T A C G G C A T genes Review Current Knowledge of Germline Genetic Risk Factors for the Development of Non-Medullary Thyroid Cancer Kinga Hi ´ncza 1,* , Artur Kowalik 1 and Aldona Kowalska 2,3 1 Department Molecular Diagnostics, Holycross Centre, 25-734 Kielce, Poland 2 The Faculty of Health Sciences of the Jan Kochanowski University, 25-317 Kielce, Poland 3 Endocrinology Clinic of Holycross Cancer Centre, 25-734 Kielce, Poland * Correspondence: [email protected]; Tel.: +48-4136-742-58 Received: 16 May 2019; Accepted: 25 June 2019; Published: 26 June 2019 Abstract: The thyroid is the most common site of endocrine cancer. One type of thyroid cancer, non-medullary thyroid cancer (NMTC), develops from follicular cells and represents approximately 90% of all thyroid cancers. Approximately 5%–15% of NMTC cases are thought to be of familial origin (FNMTC), which is defined as the occurrence of the disease in three or more first-degree relatives of the patient. It is often divided into two groups: Syndrome-associated and non-syndromic. The associated syndromes include Cowden syndrome, familial adenomatous polyposis, Gardner syndrome, Carney complex and Werner syndrome. The hereditary factors contributing to the unfavorable course of FNMTC remain poorly understood; therefore, considerable effort is being expended to identify contributing loci. Research carried out to date identifies fourteen genes (DICER1, FOXE1, PTCSC2, MYH9, SRGAP1, HABP2, BRCA1, CHEK2, ATM, RASAL1, SRRM2, XRCC1, TITF-1/NKX2.1, PTCSC3) associated with vulnerability to FNMTC that are not related to hereditary syndromes. In this review, we summarize FNMTC studies to date, and provide information on genes involved in the development of non-syndromic familial non-medullary thyroid cancers, and the significance of mutations in these genes as risk factors. -

HABP2 Sirna (Human)
For research purposes only, not for human use Product Data Sheet HABP2 siRNA (Human) Catalog # Source Reactivity Applications CRH2056 Synthetic H RNAi Description siRNA to inhibit HABP2 expression using RNA interference Specificity HABP2 siRNA (Human) is a target-specific 19-23 nt siRNA oligo duplexes designed to knock down gene expression. Form Lyophilized powder Gene Symbol HABP2 Alternative Names HGFAL; PHBP; Hyaluronan-binding protein 2; Factor VII-activating protease; Factor seven-activating protease; FSAP; Hepatocyte growth factor activator-like protein; Plasma hyaluronan-binding protein Entrez Gene 3026 (Human) SwissProt Q14520 (Human) Purity > 97% Quality Control Oligonucleotide synthesis is monitored base by base through trityl analysis to ensure appropriate coupling efficiency. The oligo is subsequently purified by affinity-solid phase extraction. The annealed RNA duplex is further analyzed by mass spectrometry to verify the exact composition of the duplex. Each lot is compared to the previous lot by mass spectrometry to ensure maximum lot-to-lot consistency. Components We offers pre-designed sets of 3 different target-specific siRNA oligo duplexes of human HABP2 gene. Each vial contains 5 nmol of lyophilized siRNA. The duplexes can be transfected individually or pooled together to achieve knockdown of the target gene, which is most commonly assessed by qPCR or western blot. Our siRNA oligos are also chemically modified (2’-OMe) at no extra charge for increased Application key: E- ELISA, WB- Western blot, IH- Immunohistochemistry, -

The Structure, Function and Evolution of the Extracellular Matrix: a Systems-Level Analysis
The Structure, Function and Evolution of the Extracellular Matrix: A Systems-Level Analysis by Graham L. Cromar A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Department of Molecular Genetics University of Toronto © Copyright by Graham L. Cromar 2014 ii The Structure, Function and Evolution of the Extracellular Matrix: A Systems-Level Analysis Graham L. Cromar Doctor of Philosophy Department of Molecular Genetics University of Toronto 2014 Abstract The extracellular matrix (ECM) is a three-dimensional meshwork of proteins, proteoglycans and polysaccharides imparting structure and mechanical stability to tissues. ECM dysfunction has been implicated in a number of debilitating conditions including cancer, atherosclerosis, asthma, fibrosis and arthritis. Identifying the components that comprise the ECM and understanding how they are organised within the matrix is key to uncovering its role in health and disease. This study defines a rigorous protocol for the rapid categorization of proteins comprising a biological system. Beginning with over 2000 candidate extracellular proteins, 357 core ECM genes and 524 functionally related (non-ECM) genes are identified. A network of high quality protein-protein interactions constructed from these core genes reveals the ECM is organised into biologically relevant functional modules whose components exhibit a mosaic of expression and conservation patterns. This suggests module innovations were widespread and evolved in parallel to convey tissue specific functionality on otherwise broadly expressed modules. Phylogenetic profiles of ECM proteins highlight components restricted and/or expanded in metazoans, vertebrates and mammals, indicating taxon-specific tissue innovations. Modules enriched for medical subject headings illustrate the potential for systems based analyses to predict new functional and disease associations on the basis of network topology. -

HABP2 Rabbit Polyclonal Antibody – TA335072 | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA335072 HABP2 Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: WB Recommended Dilution: WB Reactivity: Human Host: Rabbit Isotype: IgG Clonality: Polyclonal Immunogen: The immunogen for anti-HABP2 antibody: synthetic peptide directed towards the middle region of human HABP2. Synthetic peptide located within the following region: EPSTKLPGFDSCGKTEIAERKIKRIYGGFKSTAGKHPWQASLQSSLPLTI Formulation: Liquid. Purified antibody supplied in 1x PBS buffer with 0.09% (w/v) sodium azide and 2% sucrose. Note that this product is shipped as lyophilized powder to China customers. Purification: Affinity Purified Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 63 kDa Gene Name: hyaluronan binding protein 2 Database Link: NP_004123 Entrez Gene 3026 Human Q14520 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 HABP2 Rabbit Polyclonal Antibody – TA335072 Background: HABP2 is an extracellular serine protease that binds hyaluronic acid and is involved in cell adhesion. It is synthesized as a single chain, but then undergoes an autoproteolytic event to form the functional heterodimer. Further autoproteolysis leads to smaller, inactive peptides. This protease is known to cleave urinary plasminogen activator, coagulation factor VII, and the alpha and beta chains of fibrinogen, but not prothrombin, plasminogen, or the gamma chain of fibrinogen. -

Whole Genome Sequencing of Familial Non-Medullary Thyroid Cancer Identifies Germline Alterations in MAPK/ERK and PI3K/AKT Signaling Pathways
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 13 October 2019 doi:10.20944/preprints201910.0154.v1 Article Whole genome sequencing of familial non-medullary thyroid cancer identifies germline alterations in MAPK/ERK and PI3K/AKT signaling pathways Aayushi Srivastava 1,2,3,4, Abhishek Kumar 1,5,6, Sara Giangiobbe 1, Elena Bonora 7, Kari Hemminki 1, Asta Försti 1,2,3 and Obul Reddy Bandapalli 1,2,3,* 1 Division of Molecular Genetic Epidemiology, German Cancer Research Center (DKFZ), D-69120, Heidelberg, Germany; [email protected] (A.S.), [email protected] (A.K.); [email protected] (S.G.); [email protected] (K.H.); [email protected] (A.F.) 2 Hopp Children’s Cancer Center (KiTZ), D-69120, Heidelberg, Germany 3 Division of Pediatric Neurooncology, German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), D-69120, Heidelberg, Germany 4 Medical Faculty, Heidelberg University, D-69120, Heidelberg, Germany 5 Institute of Bioinformatics, International Technology Park, Bangalore, 560066, India 6 Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, 576104, India 7 S.Orsola-Malphigi Hospital, Unit of Medical Genetics,40138, Bologna, Italy ; [email protected] * Correspondence: [email protected]; Tel.: +49-6221-42-1709 Abstract: Evidence of familial inheritance in non-medullary thyroid cancer (NMTC) has accumulated over the last few decades. However, known variants account for a very small percentage of the genetic burden. Here, we focused on the identification of common pathways and networks enriched in NMTC families to better understand its pathogenesis with the final aim of identifying one novel high/moderate-penetrance germline predisposition variant segregating with the disease in each studied family. -

Peripheral Nerve Single-Cell Analysis Identifies Mesenchymal Ligands That Promote Axonal Growth
Research Article: New Research Development Peripheral Nerve Single-Cell Analysis Identifies Mesenchymal Ligands that Promote Axonal Growth Jeremy S. Toma,1 Konstantina Karamboulas,1,ª Matthew J. Carr,1,2,ª Adelaida Kolaj,1,3 Scott A. Yuzwa,1 Neemat Mahmud,1,3 Mekayla A. Storer,1 David R. Kaplan,1,2,4 and Freda D. Miller1,2,3,4 https://doi.org/10.1523/ENEURO.0066-20.2020 1Program in Neurosciences and Mental Health, Hospital for Sick Children, 555 University Avenue, Toronto, Ontario M5G 1X8, Canada, 2Institute of Medical Sciences University of Toronto, Toronto, Ontario M5G 1A8, Canada, 3Department of Physiology, University of Toronto, Toronto, Ontario M5G 1A8, Canada, and 4Department of Molecular Genetics, University of Toronto, Toronto, Ontario M5G 1A8, Canada Abstract Peripheral nerves provide a supportive growth environment for developing and regenerating axons and are es- sential for maintenance and repair of many non-neural tissues. This capacity has largely been ascribed to paracrine factors secreted by nerve-resident Schwann cells. Here, we used single-cell transcriptional profiling to identify ligands made by different injured rodent nerve cell types and have combined this with cell-surface mass spectrometry to computationally model potential paracrine interactions with peripheral neurons. These analyses show that peripheral nerves make many ligands predicted to act on peripheral and CNS neurons, in- cluding known and previously uncharacterized ligands. While Schwann cells are an important ligand source within injured nerves, more than half of the predicted ligands are made by nerve-resident mesenchymal cells, including the endoneurial cells most closely associated with peripheral axons. At least three of these mesen- chymal ligands, ANGPT1, CCL11, and VEGFC, promote growth when locally applied on sympathetic axons.