Microbiological Characteristics of Corynebacterium Striatum, an Emerging Pathogen
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
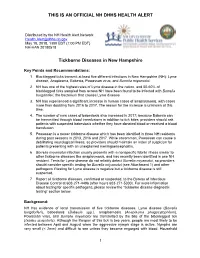
Official Nh Dhhs Health Alert
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections
toxins Review The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections Patience Shumba 1, Srikanth Mairpady Shambat 2 and Nikolai Siemens 1,* 1 Center for Functional Genomics of Microbes, Department of Molecular Genetics and Infection Biology, University of Greifswald, D-17489 Greifswald, Germany; [email protected] 2 Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, University of Zurich, CH-8091 Zurich, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +49-3834-420-5711 Received: 20 May 2019; Accepted: 10 June 2019; Published: 11 June 2019 Abstract: Necrotizing soft tissue infections (NSTIs) are critical clinical conditions characterized by extensive necrosis of any layer of the soft tissue and systemic toxicity. Group A streptococci (GAS) and Staphylococcus aureus are two major pathogens associated with monomicrobial NSTIs. In the tissue environment, both Gram-positive bacteria secrete a variety of molecules, including pore-forming exotoxins, superantigens, and proteases with cytolytic and immunomodulatory functions. The present review summarizes the current knowledge about streptococcal and staphylococcal toxins in NSTIs with a special focus on their contribution to disease progression, tissue pathology, and immune evasion strategies. Keywords: Streptococcus pyogenes; group A streptococcus; Staphylococcus aureus; skin infections; necrotizing soft tissue infections; pore-forming toxins; superantigens; immunomodulatory proteases; immune responses Key Contribution: Group A streptococcal and Staphylococcus aureus toxins manipulate host physiological and immunological responses to promote disease severity and progression. 1. Introduction Necrotizing soft tissue infections (NSTIs) are rare and represent a more severe rapidly progressing form of soft tissue infections that account for significant morbidity and mortality [1]. -

ID 2 | Issue No: 4.1 | Issue Date: 29.10.14 | Page: 1 of 24 © Crown Copyright 2014 Identification of Corynebacterium Species
UK Standards for Microbiology Investigations Identification of Corynebacterium species Issued by the Standards Unit, Microbiology Services, PHE Bacteriology – Identification | ID 2 | Issue no: 4.1 | Issue date: 29.10.14 | Page: 1 of 24 © Crown copyright 2014 Identification of Corynebacterium species Acknowledgments UK Standards for Microbiology Investigations (SMIs) are developed under the auspices of Public Health England (PHE) working in partnership with the National Health Service (NHS), Public Health Wales and with the professional organisations whose logos are displayed below and listed on the website https://www.gov.uk/uk- standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical- laboratories. SMIs are developed, reviewed and revised by various working groups which are overseen by a steering committee (see https://www.gov.uk/government/groups/standards-for-microbiology-investigations- steering-committee). The contributions of many individuals in clinical, specialist and reference laboratories who have provided information and comments during the development of this document are acknowledged. We are grateful to the Medical Editors for editing the medical content. For further information please contact us at: Standards Unit Microbiology Services Public Health England 61 Colindale Avenue London NW9 5EQ E-mail: [email protected] Website: https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality- and-consistency-in-clinical-laboratories UK Standards for Microbiology Investigations are produced in association with: Logos correct at time of publishing. Bacteriology – Identification | ID 2 | Issue no: 4.1 | Issue date: 29.10.14 | Page: 2 of 24 UK Standards for Microbiology Investigations | Issued by the Standards Unit, Public Health England Identification of Corynebacterium species Contents ACKNOWLEDGMENTS ......................................................................................................... -

Scarlet Fever Fact Sheet
Scarlet Fever Fact Sheet Scarlet fever is a rash illness caused by a bacterium called Group A Streptococcus (GAS) The disease most commonly occurs with GAS pharyngitis (“strep throat”) [See also Strep Throat fact sheet]. Scarlet fever can occur at any age, but it is most frequent among school-aged children. Symptoms usually start 1 to 5 days after exposure and include: . Sandpaper-like rash, most often on the neck, chest, elbows, and on inner surfaces of the thighs . High fever . Sore throat . Red tongue . Tender and swollen neck glands . Sometimes nausea and vomiting Scarlet fever is usually spread from person to person by direct contact The strep bacterium is found in the nose and/or throat of persons with strep throat, and can be spread to the next person through the air with sneezing or coughing. People with scarlet fever can spread the disease to others until 24 hours after treatment. Treatment of scarlet fever is important Persons with scarlet fever can be treated with antibiotics. Treatment is important to prevent serious complications such as rheumatic fever and kidney disease. Infected children should be excluded from child care or school until 24 hours after starting treatment. Scarlet fever and strep throat can be prevented . Cover the mouth when coughing or sneezing. Wash hands after wiping or blowing nose, coughing, and sneezing. Wash hands before preparing food. See your doctor if you or your child have symptoms of scarlet fever. Maryland Department of Health Infectious Disease Epidemiology and Outbreak Response Bureau Prevention and Health Promotion Administration Web: http://health.maryland.gov February 2013 . -
Chapter 11 – PROKARYOTES: Survey of the Bacteria & Archaea
Chapter 11 – PROKARYOTES: Survey of the Bacteria & Archaea 1. The Bacteria 2. The Archaea Important Metabolic Terms Oxygen tolerance/usage: aerobic – requires or can use oxygen (O2) anaerobic – does not require or cannot tolerate O2 Energy usage: autotroph – uses CO2 as a carbon source • photoautotroph – uses light as an energy source • chemoautotroph – gets energy from inorganic mol. heterotroph – requires an organic carbon source • chemoheterotroph – gets energy & carbon from organic molecules …more Important Terms Facultative vs Obligate: facultative – “able to, but not requiring” e.g. • facultative anaerobes – can survive w/ or w/o O2 obligate – “absolutely requires” e.g. • obligate anaerobes – cannot tolerate O2 • obligate intracellular parasite – can only survive within a host cell The 2 Prokaryotic Domains Overview of the Bacterial Domain We will look at examples from several bacterial phyla grouped largely based on rRNA (ribotyping): Gram+ bacteria • Firmicutes (low G+C), Actinobacteria (high G+C) Proteobacteria (Gram- heterotrophs mainly) Gram- nonproteobacteria (photoautotrophs) Chlamydiae (no peptidoglycan in cell walls) Spirochaetes (coiled due to axial filaments) Bacteroides (mostly anaerobic) 1. The Gram+ Bacteria Gram+ Bacteria The Gram+ bacteria are found in 2 different phyla: Firmicutes • low G+C content (usually less than 50%) • many common pathogens Actinobacteria • high G+C content (greater than 50%) • characterized by branching filaments Firmicutes Characteristics associated with this phylum: • low G+C Gram+ bacteria -

Corynebacterium Species Rarely Cause Orthopedic Infections
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2018 Corynebacterium species rarely cause orthopedic infections Kalt, Fabian ; Schulthess, Bettina ; Sidler, Fabian ; Herren, Sebastian ; Fucentese, Sandro F ; Zingg, Patrick O ; Berli, Martin ; Zinkernagel, Annelies S ; Zbinden, Reinhard ; Achermann, Yvonne Abstract: Corynebacterium spp. are rarely considered as pathogens but data in orthopedic infections are sparse. Therefore, we asked how often Corynebacterium spp. caused an infection in a defined cohort of orthopedic patients with a positive culture. In addition, we aimed to determine the species variety and susceptibility of isolated strains in regards to potential treatment strategies. Between 2006 and 2015, we retrospectively assessed all Corynebacterium sp. bone and joint cultures from an orthopedic ward. The isolates were considered as relevant indicating an infection if the same Corynebacterium sp. was present in at least two samples. We found 97 orthopedic cases with isolation of Corynebacterium spp. (128 positive samples), mainly Corynebacterium tuberculostearicum (n=26), Corynebacterium amycolatum (n=17), Corynebacterium striatum (n=13), and Corynebacterium afermentans (n=11). Compared to a cohort of positive blood cultures, we found significantly more C. striatum and C. tuberculostearicum but no C. jeikeium cases. Only 16 cases out 66 cases (24.2%) with an available diagnostic set of at least 2 samples had an infection. Antibiotic susceptibility testing (AST) of different antibiotics showed various susceptibility results except for vancomycin and linezolid with a 100% susceptibility rate. Rates of susceptibility of corynebacteria isolated from orthopedic samples and of isolates from blood cultures were comparable. In conclusion, our study results confirmed that Corynebacterium sp. -

Streptococcus Pneumoniae Technical Sheet
technical sheet Streptococcus pneumoniae Classification On necropsy, a serosanguineous to purulent exudate Alpha-hemolytic, Gram-positive, encapsulated, aerobic is often found in the nasal cavities and the tympanic diplococcus bullae. The lungs can have areas of firm, dark red consolidation. Fibrinopurulent pleuritis, pericarditis, Family and peritonitis are other changes seen on necropsy of animals affected by S. pneumoniae. Histologic Streptococcaceae lesions are consistent with necropsy findings, Affected species and bronchopneumonia of varying severity and fibrinopurulent serositis are often seen. Primarily described as a pathogen of rats and guinea pigs. Mice are susceptible to infection. Agent of human Diagnosis disease and human carriers are a likely source of An S. pneumoniae infection should be suspected if animal infections. Zoonotic infection is possible. encapsulated Gram-positive diplococci are seen on a smear from a lesion. Confirmation of the diagnosis is Frequency via culture of lesions or affected tissues. S. pneumoniae Rare in modern laboratory animal colonies. Prevalence grows best on 5% blood agar and is alpha-hemolytic. in pet and wild populations unknown. The organism is then presumptively identified with an optochin test. PCR assays are also available for Transmission diagnosis. PCR-based screening for S. pneumoniae Transmission is primarily via aerosol or contact with may be conducted on respiratory samples or feces. nasal or lacrimal secretions of an infected animal. S. PCR may also be useful for confirmation of presumptive pneumoniae may be cultured from the nasopharynx and microbiologic identification or confirming the identity of tympanic bullae. bacteria observed in histologic lesions. Clinical Signs and Lesions Interference with Research Inapparent infections and carrier states are common, Animals carrying S. -

A Case of Severe Human Granulocytic Anaplasmosis in an Immunocompromised Pregnant Patient
Elmer ress Case Report J Med Cases. 2015;6(6):282-284 A Case of Severe Human Granulocytic Anaplasmosis in an Immunocompromised Pregnant Patient Marijo Aguileraa, c, Anne Marie Furusethb, Lauren Giacobbea, Katherine Jacobsa, Kirk Ramina Abstract festations include respiratory or neurologic involvement, acute renal failure, invasive opportunistic infections and a shock- Human granulocytic anaplasmosis (HGA) is a tick-borne disease that like illness [2-4]. Recent delineation of the various species can often result in persistent fevers and other non-specific symptoms associated with ehrlichia infections and an increased under- including myalgias, headache, and malaise. The incidence among en- standing of the epidemiology has augmented our knowledge of demic areas has been increasing, and clinician recognition of disease these tick-borne diseases. However, a detailed understanding symptoms has aided in the correct diagnosis and treatment of patients of HGA infections in both immunocompromised and pregnant who have been exposed. While there have been few cases reported of patients is limited. We report a case of a severe HGA infection HGA disease during pregnancy, all patients have undergone a rela- presenting as an acute exacerbation of Crohn’s disease in a tively mild disease course without complications. HGA may cause pregnant immunocompromised patient. more severe disease in the elderly and immunocompromised. Herein, we report an unusual presentation and severe disease complications of HGA in a pregnant female who was concomitantly immunocompro- Case Report mised due to azathioprine treatment of her Crohn’s disease. Follow- ing successful treatment with rifampin, she subsequently delivered a A 34-year-old primigravida at 17+2 weeks’ gestation presented healthy female infant without any disease sequelae. -

Corynebacterium Striatum: an Emerging Respiratory Pathogen
Brief Original Article Corynebacterium striatum: an emerging respiratory pathogen Malini Shariff1, Aditi1, Kiran Beri1 1 Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India Abstract Introduction: Corynebacterium spp. are primarily considered normal flora and dismissed when isolated from clinical specimens. In recent years, Corynebacterium striatum has emerged as a multi-drug resistant human pathogen which can cause nosocomial outbreaks. The organism has infrequently been noted to cause respiratory infections. A retrospective study was conducted to identify the clinical and microbiological features of respiratory infection by Corynebacterium striatum. Methodology: C. striatum isolates from clinical and surveillance samples were tested for susceptibility to antimicrobials and typed by Random Amplification of Polymorphic DNA (RAPD). Clinical data was obtained through a retrospective review of records. Results: 15 isolates from clinical and surveillance samples of 11 hospitalised patients were included. The patients suffered from either an exacerbation of COPD (n = 9) or pneumonia (n = 2). The isolates were all multi-drug resistant. RAPD typing found no evidence of an outbreak/ transmission between patients. Conclusions: Corynebacterium spp. must be considered potential pathogens. Suspicious isolates should be identified to the species level since Corynebacterium striatum is often multi-drug resistant. Key words: Corynebacterium; diphtheroid; respiratory infection; MDR; RAPD. J Infect Dev Ctries 2018; 12(7):581-586. doi:10.3855/jidc.10406 (Received 28 March 2018 – Accepted 14 May 2018) Copyright © 2018 Shariff et al. This is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Introduction approved by the Institute Ethics Committee. -

Induction and Resuscitation of Viable but Nonculturable Corynebacterium Diphtheriae
microorganisms Communication Induction and Resuscitation of Viable but Nonculturable Corynebacterium diphtheriae Takashi Hamabata 1, Mitsutoshi Senoh 2,*, Masaaki Iwaki 3, Ayae Nishiyama 1, Akihiko Yamamoto 3 and Keigo Shibayama 2 1 Research Institute, National Center for Global Health and Medicine, Tokyo 162-8655, Japan; [email protected] (T.H.); [email protected] (A.N.) 2 Department of Bacteriology II, National Institute of Infectious Diseases, Tokyo 208-0011, Japan; [email protected] 3 Management Department of Biosafety and Laboratory Animal, National Institute of Infectious Diseases, Tokyo 208-0011, Japan; [email protected] (M.I.); [email protected] (A.Y.) * Correspondence: [email protected]; Tel.: +81-42-561-0771 Abstract: Many pathogenic bacteria, including Escherichia coli and Vibrio cholerae, can become vi- able but nonculturable (VBNC) following exposure to specific stress conditions. Corynebacterium diphtheriae, a known human pathogen causing diphtheria, has not previously been shown to enter the VBNC state. Here, we report that C. diphtheriae can become VBNC when exposed to low tem- peratures. Morphological differences in culturable and VBNC C. diphtheriae were examined using scanning electron microscopy. Culturable cells presented with a typical rod-shape, whereas VBNC cells showed a distorted shape with an expanded center. Cells could be transitioned from VBNC to culturable following treatment with catalase. This was further evaluated via RNA sequence-based transcriptomic analysis and reverse-transcription quantitative PCR of culturable, VBNC, and resusci- Citation: Hamabata, T.; Senoh, M.; tated VBNC cells following catalase treatment. As expected, many genes showed different behavior Iwaki, M.; Nishiyama, A.; Yamamoto, A.; Shibayama, K. -

Human Microbiota Network: Unveiling Potential Crosstalk Between the Different Microbiota Ecosystems and Their Role in Health and Disease
nutrients Review Human Microbiota Network: Unveiling Potential Crosstalk between the Different Microbiota Ecosystems and Their Role in Health and Disease Jose E. Martínez †, Augusto Vargas † , Tania Pérez-Sánchez , Ignacio J. Encío , Miriam Cabello-Olmo * and Miguel Barajas * Biochemistry Area, Department of Health Science, Public University of Navarre, 31008 Pamplona, Spain; [email protected] (J.E.M.); [email protected] (A.V.); [email protected] (T.P.-S.); [email protected] (I.J.E.) * Correspondence: [email protected] (M.C.-O.); [email protected] (M.B.) † These authors contributed equally to this work. Abstract: The human body is host to a large number of microorganisms which conform the human microbiota, that is known to play an important role in health and disease. Although most of the microorganisms that coexist with us are located in the gut, microbial cells present in other locations (like skin, respiratory tract, genitourinary tract, and the vaginal zone in women) also play a significant role regulating host health. The fact that there are different kinds of microbiota in different body areas does not mean they are independent. It is plausible that connection exist, and different studies have shown that the microbiota present in different zones of the human body has the capability of communicating through secondary metabolites. In this sense, dysbiosis in one body compartment Citation: Martínez, J.E.; Vargas, A.; may negatively affect distal areas and contribute to the development of diseases. Accordingly, it Pérez-Sánchez, T.; Encío, I.J.; could be hypothesized that the whole set of microbial cells that inhabit the human body form a Cabello-Olmo, M.; Barajas, M. -

Microbial Community and Vibrio Parahaemolyticus Population Dynamics in Relayed Oysters
University of New Hampshire University of New Hampshire Scholars' Repository Doctoral Dissertations Student Scholarship Fall 2017 MICROBIAL COMMUNITY AND VIBRIO PARAHAEMOLYTICUS POPULATION DYNAMICS IN RELAYED OYSTERS Michael Anthony Taylor University of New Hampshire, Durham Follow this and additional works at: https://scholars.unh.edu/dissertation Recommended Citation Taylor, Michael Anthony, "MICROBIAL COMMUNITY AND VIBRIO PARAHAEMOLYTICUS POPULATION DYNAMICS IN RELAYED OYSTERS" (2017). Doctoral Dissertations. 2288. https://scholars.unh.edu/dissertation/2288 This Dissertation is brought to you for free and open access by the Student Scholarship at University of New Hampshire Scholars' Repository. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of University of New Hampshire Scholars' Repository. For more information, please contact [email protected]. MICROBIAL COMMUNITY AND VIBRIO PARAHAEMOLYTICUS POPULATION DYNAMICS IN RELAYED OYSTERS BY MICHAEL ANTHONY TAYLOR BS, University of New Hampshire, 2002 Master’s Degree, University of New Hampshire, 2005 DISSERTATION Submitted to the University of New Hampshire in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Microbiology September, 2017 This dissertation has been examined and approved in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Microbiology by: Dissertation Director, Stephen H. Jones Research Associate Professor, Natural Resources and the Environment Cheryl A. Whistler, Associate Professor, Molecular, Cellular & Biomedical Sciences Vaughn S. Cooper, Associate Professor, Microbiology & Molecular Genetics, University of Pittsburg School of Medicine Kirk Broders, Assistant Professor, Plant Pathology, Colorado State University College of Agricultural Sciences Thomas Howell, President / Owner, Spinney Creek Shellfish, Inc., Eliot, Maine On March 24, 2017 Original approval signatures are on file with the University of New Hampshire Graduate School.