Targeting the Epigenome for Treatment of Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
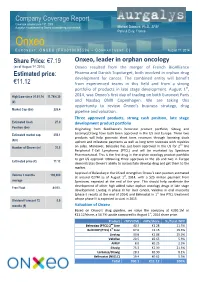
Company Coverage Report
Company Coverage Report th Coverage initiated June 19 , 2009 Aurgalys is contracted by Onxeo to provide equity research Mickael Dubourd, Ph.D., SFAF Paris & Evry, France Onxeo E URONEXT : ONXEO [FR0010095596 – C OMPARTMENT C] August 1st, 2014 Share Price: €7.19 Onxeo, leader in orphan oncology (as of August 1st, 2014) Onxeo resulted from the merger of French BioAlliance Estimated price: Pharma and Danish Topotarget, both involved in orphan drug development for cancer. The combined entity will benefit €11.12 from experienced teams in this field and from a strong portfolio of products in late stage development. August 1st, High/Low since 01.01.14 11.74/4.30 2014, was Onxeo’s first day of trading on both Euronext Paris (€) and Nasdaq OMX Copenhagen. We are taking this opportunity to review Onxeo’s business strategy, drug Market Cap (€m) 226.4 pipeline and valuation. Three approved products, strong cash position, late stage Estimated Cash 27.0 development product portfolio Position (€m) Originating from BioAlliance's historical product portfolio, Sitavig and Estimated market cap. 350.1 Loramyc/Oravig have both been approved in the US and Europe. These two products will help generate short term revenues through licensing deals (€m) upfront and milestone payments as well as long term revenues with royalties nd Number of Shares (m) 31.5 on sales. Moreover, Beleodaq has just been approved in the US for 2 line Peripheral T-Cell Lymphoma (PTCL) and will be marketed by Spectrum Pharmaceutical. This is the first drug in the orphan oncology product portfolio to get US approval. -

National Cancer Institute Cancer National
DIVISION OF CANCER TREATMENT AND DIAGNOSIS National Cancer Institute Cancer National PROGRAM ACCOMPLISHMENTS 2006 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health TABLE OF CONTENTS Foreword . iii Division of Cancer Treatment and Diagnosis Overview . .1 Major Ongoing Initiatives and Accomplishments . .7 Biometric Research Branch Overview . 11 Partnerships and Collaborations . 12 Scientific Advances . 17 Other Biostatistical Research . 24 Tools, Products, and Resources . 27 Cancer Diagnosis Program Overview . 29 Major Ongoing Initiatives . 30 Current Funding Opportunities . 34 Partnerships and Collaborations . 36 Scientific Advances . 39 Tools, Products, and Resources . 41 Cancer Imaging Program Overview . 45 Major Ongoing Initiatives . 47 Current Funding Opportunities . 54 Partnerships and Collaborations . 57 Scientific Advances . 61 Tools, Products, and Resources . 63 Cancer Therapy Evaluation Program Overview . 65 Major Ongoing Initiatives . 67 Significant Ongoing Clinical Trials . 71 Current Funding Opportunities . 73 Partnerships and Collaborations . 75 Scientific Advances . 79 Tools, Products, and Resources . 92 TABLE OF CONTENTS ■ i Developmental Therapeutics Program Overview . 95 New Initiatives . 97 Major Ongoing Initiatives . .100 Current Funding Opportunities . .104 Tools, Products, and Resources . .105 History-Marking Event . .114 Scientific Advances . .115 Radiation Research Program Overview . .119 Partnerships and Collaborations . .121 Scientific Advances . .127 Tools, Products, and Resources . .129 -

Belinostat Phase II Trial Initiated in Platinum-Resistant Ovarian Cancer by the Gynecologic Oncology Group (GOG) Supported by the National Cancer Institute (US)
To NASDAQ OMX Copenhagen A/S TopoTarget A/S Announcement No. 01-10 / Copenhagen, January 6 2010 Symbion Fruebjergvej 3 DK 2100 Copenhagen Denmark Tel: +45 39 17 83 92 Fax: +45 39 17 94 92 CVR-nr: 25695771 www.topotarget.com Belinostat phase II trial initiated in platinum-resistant ovarian cancer by the Gynecologic Oncology Group (GOG) supported by the National Cancer Institute (US) Copenhagen, Denmark – January 6, 2010 – TopoTarget A/S (OMX: TOPO) announced today that GOG (The Gynecologic Oncology Group, US) has initiated a phase II trial evaluating efficacy and safety of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube or peritoneal cancer. GOG receives support for this trial from the National Cancer Institute (NCI) of the National Institutes of Health (NIH). “Positive efficacy and safety data with belinostat and carboplatin and paclitaxel (BelCaP) in patients with platinum resistant ovarian cancer have previously been announced by TopoTarget. We are very pleased that GOG now initiates this phase II study with belinostat and carboplatin (BelCar) in this difficult to treat patient population. Platin-resistance is a huge unsolved clinical problem in relapsing ovarian cancer and hopefully GOG will be able to show that BelCar, without additional paclitaxel is active in the platinum resistant setting.” said MD., Professor Peter Buhl Jensen, CEO of TopoTarget “ if GOG is able to repeat our initial positive results in platinum resistant patients we hope to advance into pivotal trials.” The study A Phase II evaluation of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube, or primary peritoneal cancer. -

Clinical Study Report Belinostat Study Report No: PXD101-CLN-8/PXD101-040-EU
Topotarget A/S - Spectrum Pharmaceuticals, Inc. Module 5 Clinical Study Report Belinostat Study Report No: PXD101-CLN-8/PXD101-040-EU 2 SYNOPSIS NAME OF COMPANY: Individual Study Table (FOR NATIONAL AUTHORITY Topotarget A/S, CuraGen, and Spectrum Referring to Part of the USE ONLY) Pharmaceuticals, Inc. Dossier: NAME OF FINISHED PRODUCT: Belinostat Injection 50 mg/mL Volume: NAME OF ACTIVE INGREDIENT: Belinostat (PXD101) Page: TITLE OF STUDY: A Phase 1/2 Safety, Pharmacodynamic, and Pharmacokinetic Study of Intravenously Administered PXD101 Plus Carboplatin or Paclitaxel or Both in Patients with Advanced Solid Tumors INVESTIGATORS: Coordinating Investigator (Site 001): Dr. Ulrik Lassen, Department of Oncology, The Finsen Center, Copenhagen University Hospital, Copenhagen, DK. Principal Investigators: Site 002: Dr, Johann de Bono. Site 003: Dr. Robert John Jones. Site 004: Dr. Lisa Sengeløv. Site 101: Dr. Richard Penson. Site 102: Dr Don Dizon. Site 105: Dr. James Hoffman. Site 106: Dr. John Micha. Site 108: Dr. Neil Finkler. Site 109 Dr. Patricia Braly. Site 111: Dr. Paul Celano. STUDY CENTERS: Part A: The Phase 1 part (advanced tumor) was conducted at: • Site 001: The Finsen Center, Copenhagen University Hospital, DK • Site 002: The Royal Marsden NHS Trust, Cancer Research, UK • Site 101: Massachusetts General Hospital Cancer center, Boston, US Part B: The Phase 2 part, MTD expansion phase (ovarian cancer) was conducted at: • Site 001: The Finsen Center, Copenhagen University Hospital, DK • Site 002: The Royal Marsden NHS Trust, Cancer -

Pricing of Cancer Medicines and Its Impacts
ACCESS TO MEDICINES, VACCINES AND PHARMACEUTICALS TECHNICAL REPORT Pricing of cancer medicines and its impacts A comprehensive technical report for the World Health Assembly Resolution 70.12 Operative paragraph 2.9 on pricing approaches and their impacts on availability and affordability of medicines for the prevention and treatment of cancer TECHNICAL REPORT Pricing of cancer medicines and its impacts Pricing of cancer medicines and its impacts ISBN 978-92-4-151511-5 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. -

140703EN NDA Belinostat
FDA approval of Beleodaq™ (belinostat) Accelerated Approval of Topotarget’s Beleodaq™ for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma Early Action follows Priority Review 5 weeks before PDUFA Date Trigger milestone payment of USD 25 million to Topotarget Beleodaq™ is expected to be available to patients in July 2014 and will be launched through Spectrum Pharmaceutical's existing oncology sales force The Orphan Oncology Innovator BioAlliance Pharma and Topotarget are merging to create Onxeo, following approval of both companies shareholders end of June 2014 Paris, July 3, 2014 – BioAlliance Pharma SA (Euronext Paris - BIO), an innovative Company specialized in the development of drugs in orphan oncology diseases, today announced that the U.S. Food and Drug Administration (FDA) has granted Topotarget Accelerated Approval of Beleodaq™ for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma (R/R PTCL). This follows a Priority Review of the Beleodaq™ New Drug Application (NDA) and was an Early Approval action prior to the August 9, 2014 PDUFA (Prescription Drug User Fee Act) date. Beleodaq™ was granted marketing authorization under the FDA’s accelerated approval program, which allows conditional approval of a medicine for a life-threatening disease based on early evidence suggesting clinical benefit. The approval is based on results from the BELIEF study, which enrolled 129 PTCL patients refractory to or who had failed at least one prior systemic therapy. A milestone cash payment of USD 25 million from Spectrum Pharmaceuticals is triggered by the NDA approval. A double-digit royalties as well as sales milestones of the aggregated net sales will be received by the company. -

Topotarget A/S Rodman & Renshaw Annual Global Investment Conference 2013 Safe Harbor Statement
Topotarget A/S Rodman & Renshaw Annual Global Investment Conference 2013 Safe harbor statement This announcement may contain forward-looking statements, including statements about Topotarget A/S’ expectations to the progression of Topotarget A/S’ clinical pipeline and with respect to cash burn guidance. Such statements are subject to risks and uncertainties of which many are outside the control of Topotarget A/S, and which could cause actual results to differ materially from those described. Topotarget A/S disclaims any intention or obligation to update or revise any forward-looking statements, whether as a result of new information, future events, or otherwise, unless required by Danish law. 2 Topotarget at a glance A Scandinavian-based biopharmaceutical company dedicated to develop and market cancer therapies • Situated in Copenhagen, Denmark with ~14 employees and a lean cost structure • Focused on the development and commercialization of belinostat, a molecular targeted cancer therapy NASDAQ OMX Listing Copenhagen 22% Symbol TOPO Denmark Switzerland 45% Market UK capitalization EUR 48 million Sweden (as of Aug 28, 2013) 20% ROW No. of shares 143,317,114 8% 4% 3 Building a strong commercial profile for belinostat Large sales potential in solid First registration filing tumors (CRC, bladder, expected Q4 2013 ovarian, NSCLC) Partnership with Spectrum Outstanding safety profile. Pharmaceuticals, Inc. Belinostat tested in more Pursuing partnerships in EU than 1,100 patients and Asia-Pac Belinostat – a pan-HDACi - Orphan indications (PTCL, -

A Preclinical Study on the Rescue of Normal Tissue by Nicotinic Acid in High-Dose Treatment with APO866, a Specific Nicotinamide Phosphoribosyltransferase Inhibitor
Published OnlineFirst June 1, 2010; DOI: 10.1158/1535-7163.MCT-09-1130 Research Article Molecular Cancer Therapeutics A Preclinical Study on the Rescue of Normal Tissue by Nicotinic Acid in High-Dose Treatment with APO866, a Specific Nicotinamide Phosphoribosyltransferase Inhibitor Uffe Høgh Olesen1,2, Annemette V. Thougaard2, Peter Buhl Jensen2, and Maxwell Sehested1,2 Abstract Inhibitor of nicotinamide phosphoribosyltransferase APO866 is a promising cancer drug currently in phase II clinical trials in oncology. Here, we present a strategy for increasing the therapeutic potential of APO866 through the rescue of normal tissues by coadministration of nicotinic acid (Vitamin B3). We examined the toxicity profile of APO866 in B6D2F1 mice and the effect of oral administration of nicotinic acid on tissue toxicity. Nicotinic acid (50 mg/kg) protects mice from death and severe toxicity from an APO866 dose (60 mg/kg) four times the monotherapy maximum tolerated dose (15 mg/kg). In a panel of six cancer cell lines, we find that three (including ML-2 cells) are protected by nicotinic acid in vitro, whereas the cytotoxi- city of APO866 remains unaffected in the remaining three (including A2780 cells). A selective biomarker for the protection by nicotinic acid was subsequently identified by quantitative RT-PCR. The expression of nicotinic acid phosphoribosyltransferase is low in the cell lines not rescued from APO866 by nicotinic acid compared with protected cell lines. The findings in cell lines translated into xenograft models in which the combination of 50 mg/kg nicotinic acid and 50 mg/kg APO866 in mouse xenografts of A2780 cells increased life span by >3-fold compared with standard treatment of 15 mg/kg, and the effect of APO866 was clearly decreased when using the same treatment paradigm in ML-2 xenografts. -
Biopartnering Executive Summary
BIOWORLD® BIOPARTNERING REPORT 2009: STRATEGIES AND PARADIGMS OF THE DEAL EXECUTIVE SUMMARY By Michael Harris, BioWorld Executive Editor and Amanda Lyle, BioWorld Managing Editor LIST OF CONTENTS Introduction and Analysis Trends Depressing First Half of 2008 in Worldwide Public Markets Drug/Device Combos Could Salvage Dropped Compounds A Match Made in Heaven; R&D Productivity Via Partnering Drug and Medical Device Deals: A Different Type of Partnership As Big Pharma Model Falters, Biotech Rides to the Rescue Deals to M&As: The Culture of False-Flagging, Shape-Shifting Notable Deals Autoimmune and Inflammation Deals Immunomedics Inks Potential $620M Deal with Nycomed ARYx Seeking New Partner for GI Program after P&G Bails Out UCB Licenses Keppra, Cimzia Rights in Japan Alizyme, Norgine Team Up in $67M Marketing Deal Bionomics Signs Merck Serono in MS, Autoimmune Partnership TransPharma Gets $35M in Osteo Deal with Lilly QLT Sells Acne Gel Product Aczone for $150M to Allergan Start-up TFT Adds NF-Kappa B Decoy Program from Anesiva Early Stage Antibody Nets EUSA $44M from GSK Scil, Pfizer Enter $250M Deal for Preclinical Osteo Drug Catalyst Partners with Centocor for Engineered Protease Drugs Galapagos Inks $395M Deal with Lilly for Osteo Drugs Alba Inks Ex-U.S./Japan Deal with Shire for Celiac Drug Excaliard Snags $15.5M and Isis Fibrosis Drugs Galapagos and Janssen in RA Partnership Axcan, Cellerix Deal for Adult Stem Cell Therapy Radius Grants Novartis Option to BA058 in Potential $500M Deal Microbia, Forest Collaborate: Up to $330M for -

Phase I Pharmacokinetic Study of Belinostat for Solid Tumors and Lymphomas in Patients with Varying Degrees of Hepatic Dysfunction
CTEP #8846 Clinical Center #11-C-0060 Phase I Pharmacokinetic Study of Belinostat for Solid Tumors and Lymphomas in Patients with Varying Degrees of Hepatic Dysfunction Abbreviated Title: PhI Belinostat ODWG Coordinating Center: Developmental Therapeutics Clinic (DTC) National Cancer Institute 10 Center Drive, 12N226 Bethesda, MD 20892 Principal Investigator: Naoko Takebe, MD, PhDA-E, DTC Bldg 31 Room 3A44 Bethesda, MD 20892 Phone: (240) 781-3398; Fax: (240) 541-4515 [email protected] NIH Co-Investigators: James H. Doroshow, MDA-E, DCTD Alice P. Chen, MDA-E, DCTD Howard Streicher, MDA-E, CTEP/DCTD Geraldine O’Sullivan Coyne, MDA-E, DCTD Non-NCI Co-investigators Lamin Juwara, CRNPA,B,E, Leidos Biomed/FNLCR Participating Centers: NCI Organ Dysfunction Working Group (ODWG): Albert Einstein College of Medicine University of California Davis Cancer Center Emory University University of Southern California/Norris Karmanos Cancer Institute Comprehensive Cancer Center City of Hope Comprehensive Cancer Center Referral Contact: Nancy Moore, RNA,B,E Bldg 10/RM 8D53 National Cancer Institute Phone: (240) 760-6045; Fax: (301) 451-5625 [email protected] Roles: Aobtains information by intervening or interacting with living individuals for research purposes; Bobtains identifiable private information about living individuals; Cobtains the voluntary informed consent of individuals to be subjects; Dmakes decisions about subject eligibility; Estudies, interprets, or analyzes identifiable private information or data/specimens for research purposes 1 CTEP #8846 Clinical Center #11-C-0060 CoH Pharmacy Contact: Timothy Synold, Pharm D FWA#: 00000692 (626) 256-4673 x 62110 Fax: (626) 471-9376 PI: Vincent Chung, MD, FACP [email protected] (626) 471-9200 Fax: (626) 301-8233 Cecilia Lau, Clinical Pharmacist [email protected] (626) 256-4673 x 64165 Fax: (626) 301-5237 PI: Edward Newman, Ph.D. -

The Orphan Oncology Innovator Definitive Merger
Press Release / Company Announcement THE ORPHAN ONCOLOGY INNOVATOR DEFINITIVE MERGER PLAN BETWEEN BIOALLIANCE PHARMA AND TOPOTARGET COMBINED ENTITY TO BE NAMED ONXEO -- Onxeo expected to have a broader complementary pipeline of late-stage products addressing significant unmet medical needs -- -- Topotarget shareholders will receive 2 new BioAlliance Pharma ordinary shares for every 27 Topotarget shares that they own, which implies approximately a 1/3 ownership for Topotarget shareholders and approximately a 2/3 ownership for BioAlliance Pharma shareholders -- -- Shareholders to vote at extraordinary general meetings on June 27, 2014 for Topotarget and June 30, 2014 for BioAlliance Pharma -- PARIS, FRANCE AND COPENHAGEN, DENMARK – May 21, 2014 – BioAlliance Pharma SA (Euronext Paris: BIO), an innovative company specializing in the development of medicines for orphan oncology diseases, and Topotarget A/S (NASDAQ OMX: TOPO) a Danish biopharmaceutical company, today announced the signature of a definitive merger plan to create the combination of BioAlliance Pharma SA and Topotarget A/S to be operating under the new name, Onxeo, with the aim of becoming a global leader in orphan oncology. The merger agreement has been unanimously approved by the Boards of Directors of both companies. The merger plan signed today confirmed the terms of the merger agreement announced on April 16, 2014, whereby the continuing entity will be BioAlliance Pharma and the exchange ratio of 2 newly issued shares in BioAlliance Pharma for every 27 Topotarget shares -

Topotarget Signs an Agreement with Potential Value of USD 350 Million
To NASDAQ OMX Copenhagen A/S TopoTarget A/S Announcement No. 02-10 / Copenhagen, 2 February 2010 Symbion Fruebjergvej 3 DK 2100 Copenhagen Denmark Tel: +45 39 17 83 92 Fax: +45 39 17 94 92 CVR-nr: 25695771 www.topotarget.com TopoTarget signs an agreement with potential value of USD 350 million with Spectrum Pharmaceuticals for the development and commercialisation of Belinostat in North America and India -A telephone conference will be held today at 13:00 CET. Dial-in details: +4570265040- • Potential value of USD 350 million plus double digit royalties • TopoTarget to receive USD 30 million cash upfront • TopoTarget and Spectrum will jointly develop belinostat with Spectrum contributing 70% of future development costs • Spectrum territory includes North America, India and a first right of offer for the Chinese market • TopoTarget can use data to commercialise belinostat in Europe, Japan and rest of the world Copenhagen, Denmark & Irvine, California, US – 2 February, 2010 – TopoTarget A/S (NASDAQ-OMX: TOPO.CO) and Spectrum Pharmaceuticals Inc. (NASDAQ: SPPI) announced today an agreement to co-develop and commercialise belinostat, TopoTarget’s lead anticancer drug for cancer in North America and India. Belinostat, an HDAC inhibitor, is in registrational clinical trial in Peripheral T-Cell Lymphoma (PTCL) as monotherapy and in a randomized phase 2 clinical trial for cancer of unknown primary site (CUP) in combination with carboplatinum and paclitaxel (BelCaP). Belinostat is currently being investigated in 20 clinical trials in haematological and solid cancers in monotherapy as well as in combination therapies. “We are very happy to enter into collaboration with Spectrum – a highly committed successful US biotech company specialised in development of oncology and haematology products and expert marketeers” said MD, Professor Peter Buhl Jensen, Chief Executive Officer of TopoTarget.