Chronic Lymphocytic Leukemia (CLL) for Patients and Their Families
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antineoplastic Agents
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Pharmacy Policy Antineoplastic Agents Policy Number: 9.700 Version Number: 2.0 Version Effective Date: 9/1/2021 Product Applicability All Plan+ Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth- MCO MassHealth- ACO Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options Note: Disclaimer and audit information is located at the end of this document. Prior Authorization Policy Products Affected: Daurismo™ (glasdegib tablet) Rubraca™ (rucaparib tablets) Erleada™ (apalutamide tablet) Sarclisa® (Isatuximab–IRFC injection) Farydak® (panobinostat capsule) Tazverik™ (tazemetostat tablet) Folotyn® (pralatrexate injection) Talzenna® (talazoparib capsule) Gleostine™ (lomustine capsule) Tibsovo® (ivosidenib tablet) Idhifa® (enasidenib mesylate tablet) Ukoniq (umbralisib tosylate tablet) Lonsurf® (tipiracil hcl and trifluridine tablet) Valchlor™ (mechlorethamine gel) Lynparza™ (olaparib capsule, and tablets) Zejula™ (niraparib capsules) Ninlaro® (ixazomib capsule) Zelboraf® (vemurafenib tablet) Odomzo® (sonidegib capsules) Zytiga® (abiraterone acetate tablet) Pomalyst® (pomalidomide capsule) + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. The Plan operates in Massachusetts under the trade name Boston Medical Center HealthNet Plan and in other states under the trade name Well Sense Health Plan. Antineoplastic Agents 1 of 4 The Plan may authorize coverage of the above products for members meeting the following criteria: Covered FDA approved indication Use Use supported by: o American Hospital Formulary Service Drug Information o DRUGDEX Information System o United States Pharmacopeia- Drug Information o National Comprehensive Cancer Network (categories 1,2a, and 2b) Medically accepted indications will also be considered for approval. -

PI3K Inhibitors in Cancer: Clinical Implications and Adverse Effects
International Journal of Molecular Sciences Review PI3K Inhibitors in Cancer: Clinical Implications and Adverse Effects Rosalin Mishra , Hima Patel, Samar Alanazi , Mary Kate Kilroy and Joan T. Garrett * Department of Pharmaceutical Sciences, College of Pharmacy, University of Cincinnati, Cincinnati, OH 45267-0514, USA; [email protected] (R.M.); [email protected] (H.P.); [email protected] (S.A.); [email protected] (M.K.K.) * Correspondence: [email protected]; Tel.: +1-513-558-0741; Fax: +1-513-558-4372 Abstract: The phospatidylinositol-3 kinase (PI3K) pathway is a crucial intracellular signaling pathway which is mutated or amplified in a wide variety of cancers including breast, gastric, ovarian, colorectal, prostate, glioblastoma and endometrial cancers. PI3K signaling plays an important role in cancer cell survival, angiogenesis and metastasis, making it a promising therapeutic target. There are several ongoing and completed clinical trials involving PI3K inhibitors (pan, isoform-specific and dual PI3K/mTOR) with the goal to find efficient PI3K inhibitors that could overcome resistance to current therapies. This review focuses on the current landscape of various PI3K inhibitors either as monotherapy or in combination therapies and the treatment outcomes involved in various phases of clinical trials in different cancer types. There is a discussion of the drug-related toxicities, challenges associated with these PI3K inhibitors and the adverse events leading to treatment failure. In addition, novel PI3K drugs that have potential to be translated in the clinic are highlighted. Keywords: cancer; PIK3CA; resistance; PI3K inhibitors Citation: Mishra, R.; Patel, H.; Alanazi, S.; Kilroy, M.K.; Garrett, J.T. -

Optumrx Brand Pipeline Forecast
RxOutlook® 1st Quarter 2019 OptumRx brand pipeline forecast Route of Regulatory Estimated Specialty Orphan Drug name Generic name Company Drug class Therapeutic use administration status release date drug drug 2019 Possible launch date Ophthalmological DS-300 DS-300 Eton undisclosed SC Filed NDA 2019 unknown N disease anti-sclerostin Evenity romosozumab Amgen Osteoporosis SC Filed NDA 2/2019 Y N monoclonal antibody tetrahydrofolate iclaprim iclaprim Motif Bio Bacterial infections IV Filed NDA 2/13/2019 Y Y dehydrogenase inhibitor tazarotene/ IDP-118 Valeant retinoid/ corticosteroid Psoriasis TOP Filed NDA 2/15/2019 N N halobetasol adenosine deaminase Mavenclad cladribine Merck/ Teva resistant Multiple sclerosis PO Filed NDA 2/15/2019 Y N deoxyadenosine analog Lotemax Gel loteprednol Valeant corticosteroid Ocular inflammation OP Filed NDA 2/25/2019 N N Nex Gen etabonate turoctocog alfa glyco-PEGylated factor NN-7088 Novo Nordisk Hemophilia IV/SC Filed BLA 2/27/2019 Y N pegol VIII derivative selective sphingosine-1 BAF-312 siponimod Novartis phosphate receptor Multiple sclerosis PO Filed NDA 3/1/2019 Y N agonist midazolam midazolam UCB benzodiazepine Seizures Intranasal Filed NDA 3/1/2019 N Y (USL-261) XeriSol glucagon Xeris glucagon analog Diabetes mellitus SC Filed NDA 3/1/2019 N N Glucagon optum.com/optumrx 1 RxOutlook® 1st Quarter 2019 Route of Regulatory Estimated Specialty Orphan Drug name Generic name Company Drug class Therapeutic use administration status release date drug drug dopamine receptor JZP-507 sodium oxybate Jazz Narcolepsy -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
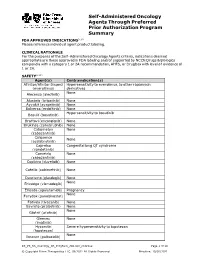
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

UKONIQ™ (Umbralisib) Tablets, for Oral Use • Severe Cutaneous Reactions: Withhold Treatment, Reduce Dose, Or Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION • Neutropenia: Monitor blood counts during treatment (5.2). These highlights do not include all the information needed to use • Diarrhea or Non-infectious colitis: Monitor for the development of diarrhea UKONIQ safely and effectively. See full prescribing information for or colitis and provide supportive care as appropriate (5.3). UKONIQ. • Hepatotoxicity: Monitor hepatic function (5.4). UKONIQ™ (umbralisib) tablets, for oral use • Severe cutaneous reactions: Withhold treatment, reduce dose, or Initial U.S. Approval: 2021 discontinue treatment depending on severity and persistence of severe cutaneous reaction (5.5). ___________________________INDICATIONS AND USAGE________________________________ • Allergic reactions due to inactive ingredient FD&C Yellow No. 5: UKONIQ is a kinase inhibitor indicated for the treatment of adult patients UKONIQ contains FD&C Yellow No. 5 (tartrazine) which may cause with: allergic-type reactions (5.6). • Relapsed or refractory marginal zone lymphoma (MZL) who have • Embryo-fetal toxicity: Can cause fetal harm. Advise patients of potential received at least one prior anti-CD20-based regimen (1.1). risk to a fetus and to use effective contraception (5.7, 8.1, 8.3). • Relapsed or refractory follicular lymphoma (FL) who have received at ____________________________ _____________________________________ least three prior lines of systemic therapy (1.2). ADVERSE REACTIONS The most common (≥15%) adverse reactions, including laboratory These indications are approved under accelerated approval based on overall abnormalities, were increased creatinine, diarrhea-colitis, fatigue, nausea, response rate. Continued approval for these indications may be contingent neutropenia, transaminase elevation, musculoskeletal pain, anemia, upon verification and description of clinical benefit in a confirmatory trial. thrombocytopenia, upper respiratory tract infection, vomiting, abdominal ________________________DOSAGE AND ADMINISTRATION_________________________ pain, decreased appetite, and rash (6.1). -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -

How We Treat Mature B-Cell Neoplasms (Indolent B-Cell Lymphomas)
Lumish et al. J Hematol Oncol (2021) 14:5 https://doi.org/10.1186/s13045-020-01018-6 REVIEW Open Access How we treat mature B-cell neoplasms (indolent B-cell lymphomas) Melissa Lumish, Lorenzo Falchi, Brandon S. Imber, Michael Scordo, Gottfried von Keudell and Erel Jofe* Abstract Mature B cell neoplasms, previously indolent non-Hodgkin lymphomas (iNHLs), are a heterogeneous group of malignancies sharing similar disease courses and treatment paradigms. Most patients with iNHL have an excellent prognosis, and in many, treatment can be deferred for years. However, some patients will have an accelerated course and may experience transformation into aggressive lymphomas. In this review, we focus on management concepts shared across iNHLs, as well as histology-specifc strategies. We address open questions in the feld, including the infuence of genomics and molecular pathway alterations on treatment decisions. In addition, we review the man- agement of uncommon clinical entities including nodular lymphocyte-predominant Hodgkin lymphoma, hairy cell leukemia, splenic lymphoma and primary lymphoma of extranodal sites. Finally, we include a perspective on novel targeted therapies, antibodies, antibody–drug conjugates, bispecifc T cell engagers and chimeric antigen receptor T cell therapy. Keywords: Indolent lymphoma, Mature B cell neoplasm, Follicular lymphoma, Marginal zone lymphoma, Active surveillance Introduction reviews have been previously published [13–19]. In this Mature B cell neoplasms, commonly known as indolent review, we will focus on general concepts in the treat- non-Hodgkin lymphomas (iNHLs), are a heterogeneous ment of iNHLs, with specifc attention to unique histolo- group of malignancies sharing similar disease courses gies and scenarios in which management should depart and treatment paradigms. -

Standard Oncology Criteria C16154-A
Prior Authorization Criteria Standard Oncology Criteria Policy Number: C16154-A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE DUE BEFORE 03/2016 12/2/2020 1/26/2022 HCPCS CODING TYPE OF CRITERIA LAST P&T APPROVAL/VERSION N/A RxPA Q1 2021 20210127C16154-A PRODUCTS AFFECTED: See dosage forms DRUG CLASS: Antineoplastic ROUTE OF ADMINISTRATION: Variable per drug PLACE OF SERVICE: Retail Pharmacy, Specialty Pharmacy, Buy and Bill- please refer to specialty pharmacy list by drug AVAILABLE DOSAGE FORMS: Abraxane (paclitaxel protein-bound) Cabometyx (cabozantinib) Erwinaze (asparaginase) Actimmune (interferon gamma-1b) Calquence (acalbrutinib) Erwinia (chrysantemi) Adriamycin (doxorubicin) Campath (alemtuzumab) Ethyol (amifostine) Adrucil (fluorouracil) Camptosar (irinotecan) Etopophos (etoposide phosphate) Afinitor (everolimus) Caprelsa (vandetanib) Evomela (melphalan) Alecensa (alectinib) Casodex (bicalutamide) Fareston (toremifene) Alimta (pemetrexed disodium) Cerubidine (danorubicin) Farydak (panbinostat) Aliqopa (copanlisib) Clolar (clofarabine) Faslodex (fulvestrant) Alkeran (melphalan) Cometriq (cabozantinib) Femara (letrozole) Alunbrig (brigatinib) Copiktra (duvelisib) Firmagon (degarelix) Arimidex (anastrozole) Cosmegen (dactinomycin) Floxuridine Aromasin (exemestane) Cotellic (cobimetinib) Fludara (fludarbine) Arranon (nelarabine) Cyramza (ramucirumab) Folotyn (pralatrexate) Arzerra (ofatumumab) Cytosar-U (cytarabine) Fusilev (levoleucovorin) Asparlas (calaspargase pegol-mknl Cytoxan (cyclophosphamide) -

American Society of Hematology (ASH) Annual Meeting December 5-8, 2020
American Society of Hematology (ASH) Annual Meeting December 5-8, 2020 http://www.hematology.org/Annual-Meeting/Program/ **Case CCC Members in BOLD; Presenter UNDERLINED** Events listed in Eastern Standard Time (EST) PRESENTATIONS/SESSION CHAIRS/MODERATORS Amar Desai, PhD Case Comprehensive Cancer Center Speaker, Regulation of the Hematopoietic Niche By 15-PGDH and Live Q&A Wednesday, Dec 2, 2020, 10:05 AM-10:45 AM; Scientific Workshops @ ASH, Stem Cells Hetty E. Carraway, MD, MBA Case Comprehensive Cancer Center, Cleveland Clinic Moderator, Blood Drop: Health Disparities Thursday, Dec 3, 2020, 10:15 AM-10:55 AM; ASH-a-Palooza Chair, Myelodysplastic Syndromes: What We Have And What We Want Speaker, Therapy For Lower Risk MDS Saturday, Dec 5, 2020, 12:30 PM-1:15 PM; Education Program ASH-a-Palooza Thank You Video (Available On-Demand beginning Dec 2) Keith R. McCrae, MD Case Comprehensive Cancer Center, Cleveland Clinic Speaker, MicroRNA and Role in Cancer Associated Thrombosis and Live Q&A Thursday, Dec 3, 2020, 10:05 AM-10:29 AM; Scientific Workshops @ ASH Speaker, Clinical Advances in Immune Thrombocytopenia: Integrating New Therapies Friday, Dec 4, 2020, 2:00 PM-5:00 PM; Sattelite Symposia Lalitha V. Nayak, MD Case Comprehensive Cancer Center, University Hospitals Speaker, NLF-2, Cancer, and Thrombosis and Live Q&A Thursday, Dec 3, 2020, 10:29 AM-11:17 AM; Scientific Workshops @ ASH, Interplay Between the Hematologic System and Solid Tumor Progression Shadi Swaidani, MD, PhD Cleveland Clinic Speaker, Elevated Systemic Myeloid-Derived -

Ukoniq (Umbralisib) Tablets
NDA 213176/Original 1 NDA 213176/Original 2 ACCELERATED APPROVAL TG Therapeutics, Inc. Attention: Anne Frederick, PhD Vice President, Global Regulatory Affairs Strategy 343 Thornall Street, Suite 740 Edison, NJ 08837 Dear Dr. Frederick: Please refer to your new drug application (NDA) dated June 15, 2020, received June 15, 2020, and your amendments, submitted under section 505(b) of the Federal Food, Drug, and Cosmetic Act (FDCA) for Ukoniq (umbralisib) tablets. NDA 213176 provides for the use of Ukoniq (umbralisib) tablets for the following indications which, for administrative purposes, we have designated as follows: NDA 213176/Original 1 – treatment of adult patients with relapsed or refractory marginal zone lymphoma (MZL) who have received at least one prior anti-CD20- based regimen NDA 213176/Original 2 – treatment of adult patients with relapsed or refractory follicular lymphoma (FL) who have received at least three prior lines of systemic therapy APPROVAL & LABELING We have completed our review of this application, as amended. It is approved under the provisions of accelerated approval regulations (21 CFR 314.500), effective on the date of this letter, for use as recommended in the enclosed agreed-upon labeling. Marketing of this drug product and related activities must adhere to the substance and procedures of the referenced accelerated approval regulations. CONTENT OF LABELING As soon as possible, but no later than 14 days from the date of this letter, submit the content of labeling [21 CFR 314.50(l)] in structured product labeling (SPL) format using the Food and Drug Administration (FDA) automated drug registration and listing system Reference ID: 4742425 NDA 213176/Original 1 NDA 213176/Original 2 Page 2 (eLIST).1 Content of labeling must be identical to the enclosed labeling (text for the Prescribing Information and Medication Guide) as well as annual reportable changes not included in the enclosed labeling. -

Master Trial List April 2021 ***New & Reopened Trials Highlighted in Green!***
MASTER TRIAL LIST APRIL 2021 ***NEW & REOPENED TRIALS HIGHLIGHTED IN GREEN!*** JUST IN TIME TRIALS (JIT) AML ANAL APL BILIARY BLADDER-UROTHELIAL BRAIN BREAST CANCER CONTROL CARCINOID CLL CML COLON-RECTAL ESOPHAGEAL - GASTRIC HEAD & NECK LYMPHOMA MDS MELANOMA MERKEL MOLECULAR STUDIES MULTIPLE MYELOMA NSCLC PANCREATIC PROSTATE RADIATION TRIALS RENAL CELL SMALL CELL LUNG CANCER VULVA Updated 4.23.21 RADIATION LOCATIONS: OSF Glen Oak - OSF main hospital OSF Route 91 (attached to Illinois CancerCare) UPHM - Unity Point Health Methodist Galesburg - Western Illinois Cancer Treatment Center MASTER TRIAL LIST MENU APRIL 2021 JUST IN TIME (JIT) TRIALS *Contact Disease Specific Navigator Brain A Prospective, Multi-Institutional Phase II Trial Evaluating Temozolomide A021804 vs. Temozolomide and Olaparib for Advanced Pheochromocytoma and Paraganglioma A Phase II Study of Checkpoint Blockade Immunotherapy in Patients With A071702 Somatically Hypermutated Recurrent Glioblastoma Breast (RT not credentialed yet)-A Phase II Randomized Trial of Olaparib (NSC- S1706 747856) Administered Concurrently with Radiotherapy versus Radiotherapy Alone for Inflammatory Breast Cancer Endometrial Genitourinary - Rare Phase II Study of Cabozantinib in Combination with Nivolumab and Ipilimumab in Rare Genitourinary Tumors (temp closed cohorts - small cell A031702 carcinoma/neuroendorine & adenocarcinoma of bladder, penile, and misc GU tract variants) Gastrointestinal Optimal Perioperative Therapy for Incidental Gallbladder Cancer (OPT-IN): EA2197 A Randomized Phase II/III -

Treating Non-Hodgkin Lymphoma If You’Ve Been Diagnosed with Non-Hodgkin Lymphoma, Your Treatment Team Will Discuss Your Options with You
cancer.org | 1.800.227.2345 Treating Non-Hodgkin Lymphoma If you’ve been diagnosed with non-Hodgkin lymphoma, your treatment team will discuss your options with you. It’s important to weigh the benefits of each treatment option against the possible risks and side effects. How is non-Hodgkin lymphoma treated? Depending on the type and stage (extent) of the lymphoma and other factors, treatment options for people with NHL might include: ● Chemotherapy for Non-Hodgkin Lymphoma ● Immunotherapy for Non-Hodgkin Lymphoma ● Targeted Drug Therapy for Non-Hodgkin Lymphoma ● Radiation Therapy for Non-Hodgkin Lymphoma ● High-Dose Chemotherapy and Stem Cell Transplant for Non-Hodgkin Lymphoma ● Surgery for Non-Hodgkin Lymphoma Common treatment approaches Treatment approaches for NHL depend on the type of cancer, how advanced it is, as well as your health and other factors. Another important part of treatment for many people is palliative or supportive care. This can help prevent or treat problems such as infections, low blood cell counts, or some symptoms caused by the lymphoma. ● Treating B-Cell Non-Hodgkin Lymphoma ● Treating T-Cell Non-Hodgkin Lymphoma ● Treating HIV-Associated Lymphoma 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 ● Palliative and Supportive Care for Non-Hodgkin Lymphoma Who treats non-Hodgkin lymphoma? Based on your treatment options, you may have different types of doctors on your treatment team. These doctors could include: ● A medical oncologist or hematologist: a doctor who treats lymphoma with chemotherapy, immunotherapy, and targeted therapy. ● A radiation oncologist: a doctor who treats cancer with radiation therapy. ● A bone marrow transplant doctor: a doctor who specializes in treating cancer or other diseases with bone marrow or stem cell transplants.