Drug Coverage Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antineoplastic Agents
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Pharmacy Policy Antineoplastic Agents Policy Number: 9.700 Version Number: 2.0 Version Effective Date: 9/1/2021 Product Applicability All Plan+ Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth- MCO MassHealth- ACO Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options Note: Disclaimer and audit information is located at the end of this document. Prior Authorization Policy Products Affected: Daurismo™ (glasdegib tablet) Rubraca™ (rucaparib tablets) Erleada™ (apalutamide tablet) Sarclisa® (Isatuximab–IRFC injection) Farydak® (panobinostat capsule) Tazverik™ (tazemetostat tablet) Folotyn® (pralatrexate injection) Talzenna® (talazoparib capsule) Gleostine™ (lomustine capsule) Tibsovo® (ivosidenib tablet) Idhifa® (enasidenib mesylate tablet) Ukoniq (umbralisib tosylate tablet) Lonsurf® (tipiracil hcl and trifluridine tablet) Valchlor™ (mechlorethamine gel) Lynparza™ (olaparib capsule, and tablets) Zejula™ (niraparib capsules) Ninlaro® (ixazomib capsule) Zelboraf® (vemurafenib tablet) Odomzo® (sonidegib capsules) Zytiga® (abiraterone acetate tablet) Pomalyst® (pomalidomide capsule) + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. The Plan operates in Massachusetts under the trade name Boston Medical Center HealthNet Plan and in other states under the trade name Well Sense Health Plan. Antineoplastic Agents 1 of 4 The Plan may authorize coverage of the above products for members meeting the following criteria: Covered FDA approved indication Use Use supported by: o American Hospital Formulary Service Drug Information o DRUGDEX Information System o United States Pharmacopeia- Drug Information o National Comprehensive Cancer Network (categories 1,2a, and 2b) Medically accepted indications will also be considered for approval. -

PI3K Inhibitors in Cancer: Clinical Implications and Adverse Effects
International Journal of Molecular Sciences Review PI3K Inhibitors in Cancer: Clinical Implications and Adverse Effects Rosalin Mishra , Hima Patel, Samar Alanazi , Mary Kate Kilroy and Joan T. Garrett * Department of Pharmaceutical Sciences, College of Pharmacy, University of Cincinnati, Cincinnati, OH 45267-0514, USA; [email protected] (R.M.); [email protected] (H.P.); [email protected] (S.A.); [email protected] (M.K.K.) * Correspondence: [email protected]; Tel.: +1-513-558-0741; Fax: +1-513-558-4372 Abstract: The phospatidylinositol-3 kinase (PI3K) pathway is a crucial intracellular signaling pathway which is mutated or amplified in a wide variety of cancers including breast, gastric, ovarian, colorectal, prostate, glioblastoma and endometrial cancers. PI3K signaling plays an important role in cancer cell survival, angiogenesis and metastasis, making it a promising therapeutic target. There are several ongoing and completed clinical trials involving PI3K inhibitors (pan, isoform-specific and dual PI3K/mTOR) with the goal to find efficient PI3K inhibitors that could overcome resistance to current therapies. This review focuses on the current landscape of various PI3K inhibitors either as monotherapy or in combination therapies and the treatment outcomes involved in various phases of clinical trials in different cancer types. There is a discussion of the drug-related toxicities, challenges associated with these PI3K inhibitors and the adverse events leading to treatment failure. In addition, novel PI3K drugs that have potential to be translated in the clinic are highlighted. Keywords: cancer; PIK3CA; resistance; PI3K inhibitors Citation: Mishra, R.; Patel, H.; Alanazi, S.; Kilroy, M.K.; Garrett, J.T. -

Optumrx Brand Pipeline Forecast
RxOutlook® 1st Quarter 2019 OptumRx brand pipeline forecast Route of Regulatory Estimated Specialty Orphan Drug name Generic name Company Drug class Therapeutic use administration status release date drug drug 2019 Possible launch date Ophthalmological DS-300 DS-300 Eton undisclosed SC Filed NDA 2019 unknown N disease anti-sclerostin Evenity romosozumab Amgen Osteoporosis SC Filed NDA 2/2019 Y N monoclonal antibody tetrahydrofolate iclaprim iclaprim Motif Bio Bacterial infections IV Filed NDA 2/13/2019 Y Y dehydrogenase inhibitor tazarotene/ IDP-118 Valeant retinoid/ corticosteroid Psoriasis TOP Filed NDA 2/15/2019 N N halobetasol adenosine deaminase Mavenclad cladribine Merck/ Teva resistant Multiple sclerosis PO Filed NDA 2/15/2019 Y N deoxyadenosine analog Lotemax Gel loteprednol Valeant corticosteroid Ocular inflammation OP Filed NDA 2/25/2019 N N Nex Gen etabonate turoctocog alfa glyco-PEGylated factor NN-7088 Novo Nordisk Hemophilia IV/SC Filed BLA 2/27/2019 Y N pegol VIII derivative selective sphingosine-1 BAF-312 siponimod Novartis phosphate receptor Multiple sclerosis PO Filed NDA 3/1/2019 Y N agonist midazolam midazolam UCB benzodiazepine Seizures Intranasal Filed NDA 3/1/2019 N Y (USL-261) XeriSol glucagon Xeris glucagon analog Diabetes mellitus SC Filed NDA 3/1/2019 N N Glucagon optum.com/optumrx 1 RxOutlook® 1st Quarter 2019 Route of Regulatory Estimated Specialty Orphan Drug name Generic name Company Drug class Therapeutic use administration status release date drug drug dopamine receptor JZP-507 sodium oxybate Jazz Narcolepsy -

NG198 Evidence Review E1
1 2 Research recommendations for review question: For people with mild to 3 moderate acne vulgaris what are the most effective treatment options? 4 Research question - physical modalities 5 What is the effectiveness of physical modalities (such as light devices) in the treatment of 6 acne vulgaris or persistent acne vulgaris-related scarring? 7 Why this is important 8 Physical treatments for acne are popular with people because they have the benefit of 9 treating a local area without systemic effects. They can be used in people with co-morbidities 10 or side effects where other treatments are unsuitable. They are currently available in the 11 private sector but there is no standardisation of treatment modalities or duration. Many 12 different physical therapies have been described for acne including: 13 • Comedone extraction 14 • Phototherapy – including UVB, intense pulsed light, blue and red light 15 • Photochemical therapy (e.g. photodynamic therapy) 16 • Laser 17 • Photopneumatic therapy (e.g. intense pulsed light + vacuum) 18 • Photothermal therapy (eg gold nanoparticles +light or laser) 19 Physical treatments are also used for acne scarring. These include: 20 • Punch excision 21 • CO2 laser 22 • Dermabrasion 23 • Radiofrequency (e.g. fractional microneedling, bipolar) 24 Further research is required to determine the most effective physical treatments for acne and 25 acne scarring. This could open the way to wider availability in the NHS. 26 Table 26: Research recommendation rationale Research question What is the effectiveness of physical modalities (such as light devices) in the treatment of acne vulgaris or persistent acne vulgaris-related scarring? Why is this needed Importance to ‘patients’ or the Physical treatments for acne are popular with people because population they have the benefit of treating a local area without systemic effects. -

June 2021 Therapeutic Research Center (TRC) Is the Leading Advisory Service on Drug Therapy and Medication Management
June 2021 Therapeutic Research Center (TRC) is the leading advisory service on drug therapy and medication management. Every month over 400,000 prescribers, pharmacists, and pharmacy technicians rely on our unbiased, evidence-based clinical recommendations to help them improve medication use, prevent medication errors, and improve patient care and outcomes. We also have one of the most extensive CE/CME course offerings in the industry. Our accredited continuing education and continuing medical education courses are trusted and relied on by hundreds of thousands of pharmacists, technicians, and prescribers every month. Therapeutic Research Center does not receive commercial support and does not accept any advertising. It is completely independent and is supported entirely by subscriptions. Credit is reported to CPE Monitor, AAFP, and CE Broker as appropriate. Accreditation Information: Therapeutic Research Center is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing education for physicians. Pharmacist’s Letter / Therapeutic Research Center is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Therapeutic Research Center / Prescriber’s Letter is accredited by the American Association of Nurse Practitioners as an approved provider of nurse practitioner continuing education. Provider number:080517. Select Therapeutic Research Center courses are also acceptable for American Academy of Family Physicians (AAFP) Prescribed credit, American Osteopathic Association (AOA) credit, and American College of Emergency Physicians (ACEP) Category I Credit. Please refer to the detailed accreditation statements available online for each course. Get started at TherapeuticResearchCenter.com. Log in to access your course list or purchase a course or subscription. For additional assistance, please call 209-472-2240 and we’ll be happy to help you. -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
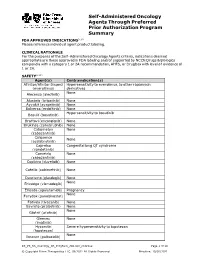
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Acne Vulgaris
CLINICAL REVIEW What’s New in the Management of Acne Vulgaris Leon H. Kircik, MD A better understanding of acne pathophysiology and the PRACTICE POINTS role of inflammation has, however, yielded a better under- • Sarecycline is the first new antibiotic approved for standing of how existing therapies treat the disease and acne in several years. have led to more comprehensive treatment strategies that • Tazarotene foam 0.1% was relaunched to the market. are multitargeted. Nonetheless, topical and oral antibiotics The foam formulation attempts to impart moisturizing remain mainstays of acne therapy, along with topical reti- effects to offset potential irritation. noids and benzoyl peroxide. Current guidelines of care for • Topical minocycline for acne optimizes the therapeutic acne emphasize strategies that reduce dependence on anti- effects while reducing systemic effects. biotics and minimizecopy the risk for resistance.4 The therapeutic • Clascoterone and cannabidiol currently are under landscape might at last be shifting, with new chemical enti- investigation for acne treatment. ties for acne and several novel formulations in development. Sarecycline: A Novel Tetracycline Tetracyclinenot antibiotics have been used to manage acne Drug development continues to focus on the challenge of treat- since the 1950s, but their method of action in the disease ing acne effectively and safely. Inflammation is a backdrop to has not been fully elucidated.5 In addition to antibiotic the commonly cited elements of the pathophysiology of acne: effects, tetracyclines have been shown to confer anti- Propionibacterium acnes proliferation, increased sebum Dopro- inflammatory properties and other biologic effects.6,7 duction with an increase in circulating androgens, and faulty keratinization. -

Novel Drug Candidates for Blast Phase Chronic Myeloid Leukemia from High-Throughput Drug Sensitivity and Resistance Testing
OPEN Citation: Blood Cancer Journal (2015) 5, e309; doi:10.1038/bcj.2015.30 www.nature.com/bcj ORIGINAL ARTICLE Novel drug candidates for blast phase chronic myeloid leukemia from high-throughput drug sensitivity and resistance testing PO Pietarinen1, T Pemovska2, M Kontro1, B Yadav2, JP Mpindi2, EI Andersson1, MM Majumder2, H Kuusanmäki2, P Koskenvesa1, O Kallioniemi2, K Wennerberg2, CA Heckman2, S Mustjoki1,3 and K Porkka1,3 Chronic myeloid leukemia in blast crisis (CML BC) remains a challenging disease to treat despite the introduction and advances in tyrosine kinase inhibitor (TKI) therapy. In this study we set out to identify novel candidate drugs for CML BC by using an unbiased high-throughput drug testing platform. We used three CML cell lines representing different types of CML blast phases (K562, EM-2 and MOLM-1) and primary leukemic cells from three CML BC patients. Profiling of drug responses was performed with a drug sensitivity and resistance testing platform comprising 295 anticancer agents. Overall, drug sensitivity scores and the drug response profiles of cell line and primary cell samples correlated well and were distinct from other types of leukemia samples. The cell lines were highly sensitive to TKIs and the clinically TKI-resistant patient samples were also resistant ex vivo. Comparison of cell line and patient sample data identified new candidate drugs for CML BC, such as vascular endothelial growth factor receptor and nicotinamide phosphoribosyltransferase inhibitors. Our results indicate that these drugs in particular warrant further evaluation by analyzing a larger set of primary patient samples. The results also pave way for designing rational combination therapies. -

UKONIQ™ (Umbralisib) Tablets, for Oral Use • Severe Cutaneous Reactions: Withhold Treatment, Reduce Dose, Or Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION • Neutropenia: Monitor blood counts during treatment (5.2). These highlights do not include all the information needed to use • Diarrhea or Non-infectious colitis: Monitor for the development of diarrhea UKONIQ safely and effectively. See full prescribing information for or colitis and provide supportive care as appropriate (5.3). UKONIQ. • Hepatotoxicity: Monitor hepatic function (5.4). UKONIQ™ (umbralisib) tablets, for oral use • Severe cutaneous reactions: Withhold treatment, reduce dose, or Initial U.S. Approval: 2021 discontinue treatment depending on severity and persistence of severe cutaneous reaction (5.5). ___________________________INDICATIONS AND USAGE________________________________ • Allergic reactions due to inactive ingredient FD&C Yellow No. 5: UKONIQ is a kinase inhibitor indicated for the treatment of adult patients UKONIQ contains FD&C Yellow No. 5 (tartrazine) which may cause with: allergic-type reactions (5.6). • Relapsed or refractory marginal zone lymphoma (MZL) who have • Embryo-fetal toxicity: Can cause fetal harm. Advise patients of potential received at least one prior anti-CD20-based regimen (1.1). risk to a fetus and to use effective contraception (5.7, 8.1, 8.3). • Relapsed or refractory follicular lymphoma (FL) who have received at ____________________________ _____________________________________ least three prior lines of systemic therapy (1.2). ADVERSE REACTIONS The most common (≥15%) adverse reactions, including laboratory These indications are approved under accelerated approval based on overall abnormalities, were increased creatinine, diarrhea-colitis, fatigue, nausea, response rate. Continued approval for these indications may be contingent neutropenia, transaminase elevation, musculoskeletal pain, anemia, upon verification and description of clinical benefit in a confirmatory trial. thrombocytopenia, upper respiratory tract infection, vomiting, abdominal ________________________DOSAGE AND ADMINISTRATION_________________________ pain, decreased appetite, and rash (6.1). -

Tivozanib for Advanced Renal Cell Carcinoma – First Line January 2011
Tivozanib for advanced renal cell carcinoma – first line January 2011 This technology summary is based on information available at the time of research and a limited literature search. It is not intended to be a definitive statement on the safety, efficacy or effectiveness of the health technology covered and should not be used for commercial purposes. The National Horizon Scanning Centre Research Programme is part of the National Institute for Health Research January 2011 Tivozanib for advanced renal cell carcinoma – first line Target group • Renal cell carcinoma (RCC): advanced – first line. Technology description Tivozanib (AV-951; KRN-951) is a selective inhibitor of vascular endothelial growth factor (VEGF) receptors 1, 2 and 3, which are involved in angiogenesis. Inhibition of VEGF driven angiogenesis has been demonstrated to reduce vascularisation of tumours, thereby suppressing tumour growth. Tivozanib is intended to substitute current therapies for the first line treatment of patients with advanced RCC. It is administered orally at 1.5mg once daily for 3 weeks in a 4 week cycle. Tivozanib is in phase I/II clinical trials for the treatment of breast cancer, gastrointestinal cancer and non-small cell lung cancer. Innovation and/or advantages If licensed, tivozanib will offer an additional first line treatment option for advanced RCC, a condition where current therapies offer relatively limited benefit. Developer AVEO Pharma Limited. Availability, launch or marketing dates, and licensing plans In phase III clinical trials. NHS or Government priority area This topic is relevant to the NHS Cancer Plan (2000) and Cancer Reform Strategy (2007). Relevant guidance • NICE technology appraisal in development. -

A Systematic Review and Meta-Analysis Comparing The
EUROPEAN UROLOGY 71 (2017) 426–436 available at www.sciencedirect.com journal homepage: www.europeanurology.com Review – Kidney Cancer A Systematic Review and Meta-analysis Comparing the Effectiveness and Adverse Effects of Different Systemic Treatments for Non-clear[3_TD$IF] Cell Renal Cell Carcinoma Sergio Ferna´ndez-Pello a,[3_TD$IF] Fabian Hofmann b, Rana Tahbaz c, Lorenzo Marconi d, Thomas B. Lam e,f, Laurence Albiges g, Karim Bensalah h, Steven E. Canfield i, Saeed Dabestani j, Rachel H. Giles k, Milan Hora l, Markus A. Kuczyk m, Axel S. Merseburger n, Thomas Powles o, Michael Staehler p, Alessandro Volpe q,Bo¨rje Ljungberg r, Axel Bex s,* a Department of Urology, Cabuen˜es Hospital, Gijo´n, Spain; b Department of Urology, Sunderby Hospital, Sunderby, Sweden; c Department of Urology, University Hospital Hamburg Eppendorf, Hamburg, Germany; d Department of Urology, Coimbra University Hospital, Coimbra, Portugal; e Academic Urology Unit, University of Aberdeen, Aberdeen, UK; f Department of Urology, Aberdeen Royal Infirmary, Aberdeen, UK; g Department of Cancer Medicine, Institut Gustave Roussy, Villejuif, France; h Department of Urology, University of Rennes, Rennes, France; i Division of Urology, University of Texas Medical School at Houston, Houston, TX, USA; j Department of Urology, Ska˚ne University Hospital, Malmo¨, Sweden; k Patient Advocate International Kidney Cancer Coalition (IKCC), University Medical Centre Utrecht, Department of Nephrology and Hypertension, Utrecht, The Netherlands; l Department of Urology, Faculty Hospital -

Individualized Systems Medicine Strategy to Tailor Treatments for Patients with Chemorefractory Acute Myeloid Leukemia
Published OnlineFirst September 20, 2013; DOI: 10.1158/2159-8290.CD-13-0350 RESEARCH ARTICLE Individualized Systems Medicine Strategy to Tailor Treatments for Patients with Chemorefractory Acute Myeloid Leukemia Tea Pemovska 1 , Mika Kontro 2 , Bhagwan Yadav 1 , Henrik Edgren 1 , Samuli Eldfors1 , Agnieszka Szwajda 1 , Henrikki Almusa 1 , Maxim M. Bespalov 1 , Pekka Ellonen 1 , Erkki Elonen 2 , Bjørn T. Gjertsen5 , 6 , Riikka Karjalainen 1 , Evgeny Kulesskiy 1 , Sonja Lagström 1 , Anna Lehto 1 , Maija Lepistö1 , Tuija Lundán 3 , Muntasir Mamun Majumder 1 , Jesus M. Lopez Marti 1 , Pirkko Mattila 1 , Astrid Murumägi 1 , Satu Mustjoki 2 , Aino Palva 1 , Alun Parsons 1 , Tero Pirttinen 4 , Maria E. Rämet 4 , Minna Suvela 1 , Laura Turunen 1 , Imre Västrik 1 , Maija Wolf 1 , Jonathan Knowles 1 , Tero Aittokallio 1 , Caroline A. Heckman 1 , Kimmo Porkka 2 , Olli Kallioniemi 1 , and Krister Wennerberg 1 ABSTRACT We present an individualized systems medicine (ISM) approach to optimize cancer drug therapies one patient at a time. ISM is based on (i) molecular profi ling and ex vivo drug sensitivity and resistance testing (DSRT) of patients’ cancer cells to 187 oncology drugs, (ii) clinical implementation of therapies predicted to be effective, and (iii) studying consecutive samples from the treated patients to understand the basis of resistance. Here, application of ISM to 28 samples from patients with acute myeloid leukemia (AML) uncovered fi ve major taxonomic drug-response sub- types based on DSRT profi les, some with distinct genomic features (e.g., MLL gene fusions in subgroup IV and FLT3 -ITD mutations in subgroup V). Therapy based on DSRT resulted in several clinical responses.