Current Treatment Options for WM
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antineoplastic Agents
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Pharmacy Policy Antineoplastic Agents Policy Number: 9.700 Version Number: 2.0 Version Effective Date: 9/1/2021 Product Applicability All Plan+ Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth- MCO MassHealth- ACO Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options Note: Disclaimer and audit information is located at the end of this document. Prior Authorization Policy Products Affected: Daurismo™ (glasdegib tablet) Rubraca™ (rucaparib tablets) Erleada™ (apalutamide tablet) Sarclisa® (Isatuximab–IRFC injection) Farydak® (panobinostat capsule) Tazverik™ (tazemetostat tablet) Folotyn® (pralatrexate injection) Talzenna® (talazoparib capsule) Gleostine™ (lomustine capsule) Tibsovo® (ivosidenib tablet) Idhifa® (enasidenib mesylate tablet) Ukoniq (umbralisib tosylate tablet) Lonsurf® (tipiracil hcl and trifluridine tablet) Valchlor™ (mechlorethamine gel) Lynparza™ (olaparib capsule, and tablets) Zejula™ (niraparib capsules) Ninlaro® (ixazomib capsule) Zelboraf® (vemurafenib tablet) Odomzo® (sonidegib capsules) Zytiga® (abiraterone acetate tablet) Pomalyst® (pomalidomide capsule) + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. The Plan operates in Massachusetts under the trade name Boston Medical Center HealthNet Plan and in other states under the trade name Well Sense Health Plan. Antineoplastic Agents 1 of 4 The Plan may authorize coverage of the above products for members meeting the following criteria: Covered FDA approved indication Use Use supported by: o American Hospital Formulary Service Drug Information o DRUGDEX Information System o United States Pharmacopeia- Drug Information o National Comprehensive Cancer Network (categories 1,2a, and 2b) Medically accepted indications will also be considered for approval. -
Cardiac Events During Treatment with Proteasome Inhibitor Therapy for Multiple Myeloma John H
Chen et al. Cardio-Oncology (2017) 3:4 DOI 10.1186/s40959-017-0023-9 RESEARCH Open Access Cardiac events during treatment with proteasome inhibitor therapy for multiple myeloma John H. Chen1*, Daniel J. Lenihan2, Sharon E. Phillips3, Shelton L. Harrell1 and Robert F. Cornell1 Abstract Background: Proteasome inhibitors (PI) bortezomib and carfilzomib are cornerstone therapies for multiple myeloma. Higher incidence of cardiac adverse events (CAEs) has been reported in patients receiving carfilzomib. However, risk factors for cardiac toxicity remain unclear. Our objective was to evaluate the incidence of CAEs associated with PI and recognize risk factors for developing events. Methods: This was a descriptive analysis of 96 patients with multiple myeloma who received bortezomib (n = 44) or carfilzomib (n = 52). We compared the cumulative incidence of CAEs using a log rank test. Patient-related characteristics were assessed and multivariate analysis was used to identify risk factors for developing CAEs. Results: PI-related CAEs occurred in 21 (22%) patients. Bortezomib-associated CAEs occurred in 7 (16%) patients while carfilzomib-associated cardiac events occurred in 14 (27%) patients. The cumulative incidence of CAEs was not significantly different between agents. Events occurred after a median of 67.5 days on PI therapy. Heart failure was the most prevalent event type. More patients receiving carfilzomib were monitored by a cardiologist. By multivariate analysis, a history of prior cardiac events and longer duration of PI therapy were identified as independent risk factors for developing CAEs. Conclusions: AEs were common in patients receiving PIs. Choice of PI did not impact the cumulative incidence of CAEs. -

PI3K Inhibitors in Cancer: Clinical Implications and Adverse Effects
International Journal of Molecular Sciences Review PI3K Inhibitors in Cancer: Clinical Implications and Adverse Effects Rosalin Mishra , Hima Patel, Samar Alanazi , Mary Kate Kilroy and Joan T. Garrett * Department of Pharmaceutical Sciences, College of Pharmacy, University of Cincinnati, Cincinnati, OH 45267-0514, USA; [email protected] (R.M.); [email protected] (H.P.); [email protected] (S.A.); [email protected] (M.K.K.) * Correspondence: [email protected]; Tel.: +1-513-558-0741; Fax: +1-513-558-4372 Abstract: The phospatidylinositol-3 kinase (PI3K) pathway is a crucial intracellular signaling pathway which is mutated or amplified in a wide variety of cancers including breast, gastric, ovarian, colorectal, prostate, glioblastoma and endometrial cancers. PI3K signaling plays an important role in cancer cell survival, angiogenesis and metastasis, making it a promising therapeutic target. There are several ongoing and completed clinical trials involving PI3K inhibitors (pan, isoform-specific and dual PI3K/mTOR) with the goal to find efficient PI3K inhibitors that could overcome resistance to current therapies. This review focuses on the current landscape of various PI3K inhibitors either as monotherapy or in combination therapies and the treatment outcomes involved in various phases of clinical trials in different cancer types. There is a discussion of the drug-related toxicities, challenges associated with these PI3K inhibitors and the adverse events leading to treatment failure. In addition, novel PI3K drugs that have potential to be translated in the clinic are highlighted. Keywords: cancer; PIK3CA; resistance; PI3K inhibitors Citation: Mishra, R.; Patel, H.; Alanazi, S.; Kilroy, M.K.; Garrett, J.T. -

Optumrx Brand Pipeline Forecast
RxOutlook® 1st Quarter 2019 OptumRx brand pipeline forecast Route of Regulatory Estimated Specialty Orphan Drug name Generic name Company Drug class Therapeutic use administration status release date drug drug 2019 Possible launch date Ophthalmological DS-300 DS-300 Eton undisclosed SC Filed NDA 2019 unknown N disease anti-sclerostin Evenity romosozumab Amgen Osteoporosis SC Filed NDA 2/2019 Y N monoclonal antibody tetrahydrofolate iclaprim iclaprim Motif Bio Bacterial infections IV Filed NDA 2/13/2019 Y Y dehydrogenase inhibitor tazarotene/ IDP-118 Valeant retinoid/ corticosteroid Psoriasis TOP Filed NDA 2/15/2019 N N halobetasol adenosine deaminase Mavenclad cladribine Merck/ Teva resistant Multiple sclerosis PO Filed NDA 2/15/2019 Y N deoxyadenosine analog Lotemax Gel loteprednol Valeant corticosteroid Ocular inflammation OP Filed NDA 2/25/2019 N N Nex Gen etabonate turoctocog alfa glyco-PEGylated factor NN-7088 Novo Nordisk Hemophilia IV/SC Filed BLA 2/27/2019 Y N pegol VIII derivative selective sphingosine-1 BAF-312 siponimod Novartis phosphate receptor Multiple sclerosis PO Filed NDA 3/1/2019 Y N agonist midazolam midazolam UCB benzodiazepine Seizures Intranasal Filed NDA 3/1/2019 N Y (USL-261) XeriSol glucagon Xeris glucagon analog Diabetes mellitus SC Filed NDA 3/1/2019 N N Glucagon optum.com/optumrx 1 RxOutlook® 1st Quarter 2019 Route of Regulatory Estimated Specialty Orphan Drug name Generic name Company Drug class Therapeutic use administration status release date drug drug dopamine receptor JZP-507 sodium oxybate Jazz Narcolepsy -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
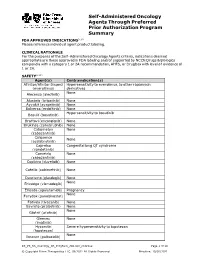
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Toward Personalized Treatment in Waldenström Macroglobulinemia
| INDOLENT LYMPHOMA:HOW UNDERSTANDING DISEASE BIOLOGY IS INFLUENCING CLINICAL DECISION-MAKING | Toward personalized treatment in Waldenstrom¨ macroglobulinemia Jorge J. Castillo and Steven P. Treon Bing Center for Waldenstrom¨ Macroglobulinemia, Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA Waldenstrom¨ macroglobulinemia (WM) is a rare lymphoma with 1000 to 1500 new patients diagnosed per year in the United States. Patients with WM can experience prolonged survival times, which seem to have increased in the last decade, but relapse is inevitable. The identification of recurrent mutations in the MYD88 and CXCR4 genes has opened avenues of research to better understand and treat patients with WM. These developments are giving way to per- sonalized treatment approaches for these patients, focusing on increasing depth and duration of response alongside lower toxicity rates. In the present document, we review the diagnostic differential, the clinical manifestations, and the pathological and genomic features of patients with WM. We also discuss the safety and efficacy data of alkylating agents, proteasome inhibitors, monoclonal antibodies, and Bruton tyrosine kinase inhibitors in patients with WM. Finally, we propose a genomically driven algorithm for the treatment of WM. The future of therapies for WM appears bright and hopeful, but we should be mindful of the cost-effectiveness and long-term toxicity of novel agents. Diagnostic considerations Learning Objectives The differential diagnosis of WM includes immunoglobulin M (IgM) • To understand recent advances on the biology of Waldenstrom¨ monoclonal gammopathy of undetermined significance; other macroglobulinemia IgM-secreting lymphomas, especially marginal zone lymphoma (MZL); • To review available and investigational agents for the treat- and the rare IgM multiple myeloma (MM). -

Abstract in Vivo Mouse Studies Drug Resistant Myeloma Cell Lines Ex
Overcoming Drug-resistance in Multiple Myeloma by CRM1 Inhibitor Combination Therapy Joel G. Turner1, Ken Shain1, Yun Dai2, Jana L. Dawson1, Chris Cubitt1, Sharon Shacham3, 1 3 2 1 H. LEE MOFFITT CANCER CENTER & RESEARCH INSTITUTE, Sharon Shacham , Michael Kaffman , Steven Grant and Daniel M. Sullivan AN NCI COMPREHENSIVE CANCER CENTER – Tampa, FL 1-888-MOFFITT (1-888-663-3488) www.MOFFITT.org 1 Moffitt Cancer Center and Research Institute, Tampa, FL © 2010 H. Lee Moffitt Cancer Center and Research Institute, Inc. 2 Virginia Commonwealth University, Richmond, VA 3 Karyopharm Therapeutics, Natick, MA Abstract Drug Resistant Myeloma Cell Lines In Vivo Mouse Studies Ex vivo Apoptosis Assay Introduction Newly Diagnosed Newly Diagnosed Significant progress has been made over the past several years in the treatment A 70 VC B 70 VC KPT-330 of multiple myeloma (MM). However patients eventually develop drug resistance A B 60 60 KPT-330 KOS-2464 KOS-2464 and die from progressive disease. The incurable nature of MM clearly 50 50 demonstrates the need for novel agents and treatments. 40 40 The overall objective of this study was to investigate the use of CRM1 inhibitors 30 30 Apoptosis (%) Apoptosis (KPT330 and KOS2464) to sensitize de novo and acquired drug-resistant MM (%) Apoptosis 20 20 cells to the proteosome inhibitors bortezomib (BTZ)and carfilzomib (CFZ) and to 10 10 the topoisomerase II (topo II) inhibitor doxorubicin (DOX). 0 0 Methods VC or Drug BTZ CFZ DOX VC or Drug BTZ CFZ DOX Drug resistant U266 and 8226 MM cell lines were developed at VCU (Steven Relapsed Relapsed Grant) and the Moffitt Cancer Center (Ken Shain) respectively by the incremental C 70 VC D 70 VC KPT-330 exposure to BTZ. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

WO 2017/173206 Al 5 October 2017 (05.10.2017) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2017/173206 Al 5 October 2017 (05.10.2017) P O P C T (51) International Patent Classification: CA 94121 (US). HUBBARD, Robert; 7684 Marker Road, A61K 31/52 (2006.01) C07D 473/02 (2006.01) San Diego, CA 92087 (US). MIKOLON, David; 6140 A61K 31/505 (2006.01) C07D 473/26 (2006.01) Calle Empinada, San Diego, CA 92120 (US). RAYMON, A61K 31/519 (2006.01) C07D 473/32 (2006.01) Heather; 3520 Vista de la Orilla, San Diego, CA 921 17 (US). SHI, Tao; 4650 Tarantella Lane, San Diego, CA (21) International Application Number: 92130 (US). TRAN, Tam, M.; 8953 Libra Drive, San PCT/US20 17/025252 Diego, CA 92126 (US). TSUJI, Toshiya; 4171 Donald (22) International Filing Date: Court, San Diego, CA 921 17 (US). WONG, Lilly, L.; 871 3 1 March 2017 (3 1.03.2017) Viva Court, Solana Beach, CA 92075 (US). XU, Suichan; 9650 Deer Trail Place, San Diego, CA 92127 (US). ZHU, (25) Filing Language: English Dan; 4432 Calle Mar De Armonia, San Diego, CA 92130 (26) Publication Language: English (US). (30) Priority Data: (74) Agents: BRUNER, Michael, J. et al; Jones Day, 250 Ve- 62/3 17,412 1 April 2016 (01.04.2016) US sey Street, New York, NY 10281-1047 (US). (71) Applicant: SIGNAL PHARMACEUTICALS, LLC (81) Designated States (unless otherwise indicated, for every [US/US]; 10300 Campus Point Drive, Suite 100, San kind of national protection available): AE, AG, AL, AM, Diego, CA 92121 (US). -

UKONIQ™ (Umbralisib) Tablets, for Oral Use • Severe Cutaneous Reactions: Withhold Treatment, Reduce Dose, Or Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION • Neutropenia: Monitor blood counts during treatment (5.2). These highlights do not include all the information needed to use • Diarrhea or Non-infectious colitis: Monitor for the development of diarrhea UKONIQ safely and effectively. See full prescribing information for or colitis and provide supportive care as appropriate (5.3). UKONIQ. • Hepatotoxicity: Monitor hepatic function (5.4). UKONIQ™ (umbralisib) tablets, for oral use • Severe cutaneous reactions: Withhold treatment, reduce dose, or Initial U.S. Approval: 2021 discontinue treatment depending on severity and persistence of severe cutaneous reaction (5.5). ___________________________INDICATIONS AND USAGE________________________________ • Allergic reactions due to inactive ingredient FD&C Yellow No. 5: UKONIQ is a kinase inhibitor indicated for the treatment of adult patients UKONIQ contains FD&C Yellow No. 5 (tartrazine) which may cause with: allergic-type reactions (5.6). • Relapsed or refractory marginal zone lymphoma (MZL) who have • Embryo-fetal toxicity: Can cause fetal harm. Advise patients of potential received at least one prior anti-CD20-based regimen (1.1). risk to a fetus and to use effective contraception (5.7, 8.1, 8.3). • Relapsed or refractory follicular lymphoma (FL) who have received at ____________________________ _____________________________________ least three prior lines of systemic therapy (1.2). ADVERSE REACTIONS The most common (≥15%) adverse reactions, including laboratory These indications are approved under accelerated approval based on overall abnormalities, were increased creatinine, diarrhea-colitis, fatigue, nausea, response rate. Continued approval for these indications may be contingent neutropenia, transaminase elevation, musculoskeletal pain, anemia, upon verification and description of clinical benefit in a confirmatory trial. thrombocytopenia, upper respiratory tract infection, vomiting, abdominal ________________________DOSAGE AND ADMINISTRATION_________________________ pain, decreased appetite, and rash (6.1). -

BC Cancer Benefit Drug List September 2021
Page 1 of 65 BC Cancer Benefit Drug List September 2021 DEFINITIONS Class I Reimbursed for active cancer or approved treatment or approved indication only. Reimbursed for approved indications only. Completion of the BC Cancer Compassionate Access Program Application (formerly Undesignated Indication Form) is necessary to Restricted Funding (R) provide the appropriate clinical information for each patient. NOTES 1. BC Cancer will reimburse, to the Communities Oncology Network hospital pharmacy, the actual acquisition cost of a Benefit Drug, up to the maximum price as determined by BC Cancer, based on the current brand and contract price. Please contact the OSCAR Hotline at 1-888-355-0355 if more information is required. 2. Not Otherwise Specified (NOS) code only applicable to Class I drugs where indicated. 3. Intrahepatic use of chemotherapy drugs is not reimbursable unless specified. 4. For queries regarding other indications not specified, please contact the BC Cancer Compassionate Access Program Office at 604.877.6000 x 6277 or [email protected] DOSAGE TUMOUR PROTOCOL DRUG APPROVED INDICATIONS CLASS NOTES FORM SITE CODES Therapy for Metastatic Castration-Sensitive Prostate Cancer using abiraterone tablet Genitourinary UGUMCSPABI* R Abiraterone and Prednisone Palliative Therapy for Metastatic Castration Resistant Prostate Cancer abiraterone tablet Genitourinary UGUPABI R Using Abiraterone and prednisone acitretin capsule Lymphoma reversal of early dysplastic and neoplastic stem changes LYNOS I first-line treatment of epidermal -

Kyprolis® (Carfilzomib)
Kyprolis® (carfilzomib) Document Number: IC-0157 Last Review Date: 12/04/2018 Date of Origin: 02/07/2013 Dates Reviewed: 12/2013, 02/2014, 06/2014, 09/2014, 12/2014, 05/2015, 08/2015, 11/2015, 02/2016, 05/2016, 08/2016, 11/2016, 02/2017, 05/2017, 08/2017, 11/2017, 02/2018, 05/2018, 09/2018, 12/2018 I. Length of Authorization Coverage will be provided for six months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [Pharmacy Benefit]: Kyprolis 30 mg powder for injection: 1 vial per 28 day supply Kyprolis 60 mg powder for injection: 12 vials per 28 day supply B. Max Units (per dose and over time) [Medical Benefit]: Multiple Myeloma o 720 billable units every 28 days Waldenström’s Macroglobulinemia/Lymphoplasmacytic Lymphoma o 320 billable units every 21 days III. Initial Approval Criteria Coverage is provided in the following conditions: Patient is at least 18 years old; AND Multiple Myeloma † Used as primary chemotherapy or for disease relapse after 6 months following primary chemotherapy with this same regimen in patients with active (symptomatic) disease; AND o Used in combination with lenalidomide and dexamethasone; OR o Used in combination with dexamethasone and cyclophosphamide in NON stem-cell transplant candidates Used for previously treated myeloma for disease relapse or for progressive or refractory disease; AND o Used as a single agent for subsequent therapy †; OR o In combination with dexamethasone with or without lenalidomide †; OR o In combinations with dexamethasone and cyclophosphamide; OR o In combination with panobinostat; AND Proprietary & Confidential © 2018 Magellan Health, Inc.