District Health Society Siwan 2010-2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gopalganj District
GOPALGANJ- DISTRICT INDUSTRIAL POTENTIAL SURVEY lR;eso t;rs Government of India Ministry of MSME Brief Industrial Profile of GOPALGANJ DISTRICT Carried out by MSME-Development Institute, Muzaffarpur (Ministry of MSME, Govt. of India,) Phone :-0621-2284425 Fax: 0621-2282486 e-mail:[email protected] Web- www.msmedimzfpur.bih.nic.in GOPALGANJ- DISTRICT INDUSTRIAL POTENTIAL SURVEY Contents S. No. Topic 1. General Characteristics of the District 1.1 Location & Geographical Area 1.2 Topography 1.3 Availability of Minerals. 1.4 Forest 1.5 Administrative set up 2. District at a glance 2.1 Existing Status of Industrial Area in the District GOPALGANJ 3. Industrial Scenario Of GOPALGANJ 3.1 Industry at a Glance 3.2 Year Wise Trend Of Units Registered 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The District 3.4 Large Scale Industries / Public Sector undertakings 3.5 Major Exportable Item 3.6 Growth Trend 3.7 Vendorisation / Ancillarisation of the Industry 3.8 Medium Scale Enterprises 3.8.1 List of the units in ------ & near by Area 3.8.2 Major Exportable Item 3.9 Service Enterprises 3.9.2 Potentials areas for service industry 3.10 Potential for new MSMEs 4. Existing Clusters of Micro & Small Enterprise 4.1 Detail Of Major Clusters x 4.1.1 Manufacturing Sector 4.1.2 Service Sector 4.2 Details of Identified cluster 4.2.1 Cluster details identified 4.2.2 Cluster details identified 5. General issues raised by industry association during the course of meeting 6 Steps to set up MSMEs GOPALGANJ- DISTRICT INDUSTRIAL POTENTIAL SURVEY Brief Industrial Profile of GOPALGANJ District 1. -

A Report on Investigation of Zika Case & Dengue Outbreak in Siwan Bihar
International Journal of Medical and Health Research International Journal of Medical and Health Research ISSN: 2454-9142 www.medicalsciencejournal.com Volume X; Issue X; October XXXX; Page No. 00-00 A report on investigation of Zika case & dengue outbreak in siwan Bihar in 2018 Dr. Nand Kishor1, Dr. Ragini Mishra2, Navnit Kumar Dutta3*, Naveen Kumar Raman4 1 Tutor, Department of Microbiology, Patna Medical College, Patna, Bihar, India 2 State Epidemiologist, IDSP, State Health Society Bihar, Patna, Bihar, India 3 Department of Microbiology, State Microbiologist, IDSP, Patna Medical College, Patna, Bihar, India 4 Department of Microbiology, District Microbiologist, IDSP, Patna Medical College, Patna, Bihar, India *Corresponding Author: Navnit Kumar Dutta Abstract Dengue outbreak in Siwan district in 2018 was investigated to determine the causes of current outbreak and prevent occurrence of outbreak in future. One patient from Hariharpur Lalgarh Village of Siwan was Zika Positive at SMS Hospital, Jaipur. Both Dengue & Zika virus is transmitted by same vector Ades Aegypti. The urban areas of Siwan like Puranikila, Siwan Nagar, Dakhintola, Sukultola, saikhtola, kagazi mohalla had reported increased number of fever cases & confirmed Dengue positive in Microbiology lab of PMCH, Patna. Entomological findings confirmed the presence of Aedine vector in the affected area. Finding confirms the factor leading to the present outbreak and highlights risk factor & control strategies to prevent future in the Siwan district. Community support and participation is also crucial for the prevention of future outbreaks and improving the health and well being of population in the Siwan district. Keywords: substituted Li ferrite, magnetostatic and spin waves, microstrip array antenna, X-band frequency range Introduction India notified the State Surveillance Unit, IDSP, Bihar about a Zika Virus Disease (ZVD) is a mosquito-borne viral infection Zika confirmed case by SMS Hospital, Jaipur on 7 Oct 2018. -
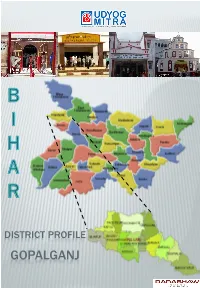
Gopalganj Introduction
DISTRICT PROFILE GOPALGANJ INTRODUCTION Gopalganj district is one of the thirty-eight administrative districts of Bihar. Gopalganj sub-division was notified as a district on October 2, 1973. Gopalganj district falls in Saran division. Gopalganj is bounded by the districts of Patna, Samastipur, Khagaria, Munger and Lakhisarai. The river flowing through Gopalganj district is Gandak. HISTORICAL BACKGROUND The composite Saran district lies on one of the main lines of the eastwards progression of the Aryans. According to the Vedic traditions, Videhas marched eastwards from the Saraswati and made the eastern banks of river Gandak their home. After crossing river Gandak, the Videhas founded a powerful kingdom on its eastern bank. It is likely that some of them settled in Saran, while the majority of them crossed the river Gandak. In pre- historic times, the present districts of Gopalganj and Siwan up to the bank of river Saryu which bounds Siwan district on its south, was a part of Nepal. The name Siwan means the boundary i.e. the southern boundary of the erstwhile Nepal kingdom. The history of Gopalganj is the history of Saran district. The ancient state of "Mallyas“ served as the frontier of Gopalganj. Saran was part of Kaushal kingdom. During the medieval period, Gopalganj came under the control of the Afghans and Mughals. Under the British, the district of Gopalganj was a Kingdom of Maharaja Fateh Shahi of Hussaipur. Until 1875 A.D., the tiny hamlet of Gopalganj was an Anchal within the erstwhile Saran district. In 1875, Gopalganj Anchal was upgraded to the status of a sub- division of the erstwhile Saran district. -

Ziradei Assembly Bihar Factbook
Editor & Director Dr. R.K. Thukral Research Editor Dr. Shafeeq Rahman Compiled, Researched and Published by Datanet India Pvt. Ltd. D-100, 1st Floor, Okhla Industrial Area, Phase-I, New Delhi- 110020. Ph.: 91-11- 43580781, 26810964-65-66 Email : [email protected] Website : www.electionsinindia.com Online Book Store : www.datanetindia-ebooks.com Report No. : AFB/BR-106-0619 ISBN : 978-93-5313-205-7 First Edition : January, 2018 Third Updated Edition : June, 2019 Price : Rs. 11500/- US$ 310 © Datanet India Pvt. Ltd. All rights reserved. No part of this book may be reproduced, stored in a retrieval system or transmitted in any form or by any means, mechanical photocopying, photographing, scanning, recording or otherwise without the prior written permission of the publisher. Please refer to Disclaimer at page no. 167 for the use of this publication. Printed in India No. Particulars Page No. Introduction 1 Assembly Constituency - (Vidhan Sabha) at a Glance | Features of Assembly 1-2 as per Delimitation Commission of India (2008) Location and Political Maps Location Map | Boundaries of Assembly Constituency - (Vidhan Sabha) in 2 District | Boundaries of Assembly Constituency under Parliamentary 3-9 Constituency - (Lok Sabha) | Town & Village-wise Winner Parties- 2019, 2014, 2010 and 2009 Administrative Setup 3 District | Sub-district | Towns | Villages | Inhabited Villages | Uninhabited 10-20 Villages | Village Panchayat | Intermediate Panchayat Demographics 4 Population | Households | Rural/Urban Population | Towns and Villages -

Vlcc Merchant VLCC KOTWALI PATNA1 Patna 800001 PATNA Vlcc
BIHAR MERCHANT NAME STORE NAME ADDRESS1 PINCODE STORE CITY Vlcc Merchant VLCC KOTWALI PATNA1 patna 800001 PATNA Vlcc Merchant VLCC ALAMGANJ CITY PATNA2 patna 800013 PATNA Samsung Mobile AXIS Ritik In Touch -Patna Verma Complex Boring Road Bihd1080 403601 PATNA Reliance Digital RDKHAJPURAPATNA Plot No 968, 998, 969, 971, 970, Thana No-11, 800014 PATNA Samsung Mobile BIHD19538 SHREE HARI Om Vihar Complex, Nala Road 800004 PATNA RELIANCE RETAIL RR Kankarbagh Patna B - 51, Sadho Shivam Complex, Type A, Thana No- 9 800008 PATNA RELIANCE RETAIL RR Gujri Bazaar Patna Holding No 30- 25-18A,Plot No - 950,Circle No-110 800008 PATNA RELIANCE RETAIL RD ASHOK RAJPATH PATNA Ward No 4130, Circle No 27, Circle, Bankipur 800004 PATNA RELIANCE RETAIL RR 7949 Civil Line GB Road Gaya Khata No 342, Plot No - 1201 Ka, Kha, Ga/ 13915 823001 GAYA RELIANCE RETAIL RD 7951 RAMPUR GAYA BIHAR Khata No 2252, Plot No 5585, 5411, Ward No 31 823001 GAYA RELIANCE RETAIL RD 7948 BATA MORE GAYA House No 355, Ward No 18, Khata No 118 823001 GAYA RELIANCE RETAIL RD 7238 BAHADURPUR PATNA Holding No 594/2/147/2 (Old), Ward No- 46, Circle 800020 PATNA RELIANCE RETAIL RD Patliputra Manpura C 22, Patliputra Industrial Estate 800013 PATNA RELIANCE RETAIL RD DHAKANPURA Shop No 213, Ground Floor, Brij Laxmi Mansion 800005 PATNA RELIANCE RETAIL RD 7801 DANAPUR PATNA Ward No 22, Holding No 23 Circle 801503 PATNA RELIANCE RETAIL RD 7822 BAILEY ROAD PATNA Mouza Rukanpura, P S Danapur Thana, No 18 800014 PATNA NOKIA MOBILE MOBTEL FRAZER RD PATNA Frazer Road 800001 PATNA RELIANCE RETAIL RD 6384 PHULWARI PATNA Holding No. -

Of India 100935 Parampara Foundation Hanumant Nagar ,Ward No
AO AO Name Address Block District Mobile Email Code Number 97634 Chandra Rekha Shivpuri Shiv Mandir Road Ward No 09 Araria Araria 9661056042 [email protected] Development Foundation Araria Araria 97500 Divya Dristi Bharat Divya Dristi Bharat Chitragupt Araria Araria 9304004533 [email protected] Nagar,Ward No-21,Near Subhash Stadium,Araria 854311 Bihar Araria 100340 Maxwell Computer Centre Hanumant Nagar, Ward No 15, Ashram Araria Araria 9934606071 [email protected] Road Araria 98667 National Harmony Work & Hanumant Nagar, Ward No.-15, Po+Ps- Araria Araria 9973299101 [email protected] Welfare Development Araria, Bihar Araria Organisation Of India 100935 Parampara Foundation Hanumant Nagar ,Ward No. 16,Near Araria Araria 7644088124 [email protected] Durga Mandir Araria 97613 Sarthak Foundation C/O - Taranand Mishra , Shivpuri Ward Araria Araria 8757872102 [email protected] No. 09 P.O + P.S - Araria Araria 98590 Vivekanand Institute Of 1st Floor Milan Market Infront Of Canara Araria Araria 9955312121 [email protected] Information Technology Bank Near Adb Chowk Bus Stand Road Araria Araria 100610 Ambedkar Seva Sansthan, Joyprakashnagar Wardno-7 Shivpuri Araria Araria 8863024705 [email protected] C/O-Krishnamaya Institute Joyprakash Nagar Ward No -7 Araria Of Higher Education 99468 Prerna Society Of Khajuri Bazar Araria Bharga Araria 7835050423 [email protected] Technical Education And ma Research 100101 Youth Forum Forbesganj Bharga Araria 7764868759 [email protected] -

Pradhan Mantri Gram Sadak Yojana CUCPL - Comprehensive Up-Gradation Cum Consolidation Priority List
Pradhan Mantri Gram Sadak Yojana CUCPL - Comprehensive Up-gradation cum Consolidation Priority List State : Bihar District : All Districts Block : All Blocks Sr.No. State District Block Plan CN Plan Road Name Plan Road Route Educati Medical Veterin Transp Market Administ Populatio Total Score Per Avg PCI Road No. Length Priority onal Faciliti ary ort and Faciliti rative n Score Unit Services es Facilitie Commu es Centres Length s nicatio n Infrastr ucture 1 Bihar Arwal Arwal MRL01 Walidad, T01 To Khamhaini 10.835 M 12 0 0.00 0.00 0.00 1 68 81.00 7.48 1.00 2 Bihar Arwal Banshi MRL02 Manjhiyama to Khatangi 9.465 M 16 8 0.00 9.00 0.00 1 77 111.00 11.73 1.00 Surajpur 3 Bihar Arwal Banshi MRL03 Kharasi to Belaura 14.943 M 22 8 0.00 3.00 0.00 1 89 123.00 8.23 1.00 Surajpur 4 Bihar Arwal Banshi MRL01 Khatangi senari RD to Mobarakpur 10.860 M 9 4 0.00 3.00 0.00 1 42 59.00 5.43 1.00 Surajpur 5 Bihar Arwal Kaler MRL01 Sohasa Road L037 To Masadpur 21.676 M 10 6 0.00 6.00 0.00 1 54 77.00 3.55 1.00 6 Bihar Arwal Karpi MRL02 Imamganj Deokund Road,T04 To Jonha 7.365 M 22 8 3.00 11.00 9.00 2 91 146.00 19.82 1.00 7 Bihar Arwal Karpi MRL01 Karpi Barahmile Road, T03 To Salarpur 12.365 M 18 6 0.00 9.00 7.00 2 104 146.00 11.81 1.00 8 Bihar Arwal Karpi MRL03 Arwal Jehanabad Road, T02 To Aiyara 16.787 M 7 0 0.00 0.00 7.00 1 52 67.00 3.99 1.00 9 Bihar Arwal Kurtha MRL02 Salarpur L042, To Dhamaul 15.238 M 9 4 0.00 3.00 7.00 2 88 113.00 7.42 1.00 10 Bihar Arwal Kurtha MRL01 Pinjrawan to Manepaker 9.456 M 8 2 0.00 0.00 0.00 1 55 66.00 6.98 1.00 11 Bihar Aurangabad -

District Health Action Plan Siwan 2012 – 13
DISTRICT HEALTH ACTION PLAN SIWAN 2012 – 13 Name of the district : Siwanfloku Create PDF files without this message by purchasing novaPDF printer (http://www.novapdf.com) Foreword National Rural health Mission was launched in India in the year 2005 with the purpose of improving the health of children and mothers and reaching out to meet the health needs of the people in the hard to reach areas of the nation. National Rural Health Mission aims at strengthening the rural health infrastructures and to improve the delivery of health services. NRHM recognizes that until better health facilities reaches the last person of the society in the rural India, the social and economic development of the nation is not possible. The District Health Action Plan of Siwan district has been prepared keeping this vision in mind. The DHAP aims at improving the existing physical infrastructures, enabling access to better health services through hospitals equipped with modern medical facilities, and to deliver the health service with the help of dedicated and trained manpower. It focuses on the health care needs and requirements of rural people especially vulnerable groups such as women and children. The DHAP has been prepared keeping in mind the resources available in the district and challenges faced at the grass root level. The plan strives to bring about a synergy among the various components of the rural health sector. In the process the missing links in this comprehensive chain have been identified and the Plan will aid in addressing these concerns. The plan has attempts to bring about a convergence of various existing health programmes and also has tried to anticipate the health needs of the people in the forthcoming years. -

Gender and Land Tenure Security
CHALLENGES GENDER AND AND BARRIERS LAND TENURE SECURITY TO WOMEN’S ENTITLEMENT TO LAND IN INDIA 0 © UN Women All rights reserved. Reproduction and dissemination of material in this publication for educational or other non- commercial purposes are authorized without prior written permission from UN Women provided the source is fully acknowledged. Reproduction of this publication for resale or other commercial purposes is prohibited without written permission from UN Women. Applications for such permission may be addressed to [email protected] Published by: UN Women www.unwomen.org Disclaimer: The views expressed in this publication are those of the Rural Development Institute, and do not necessarily represent the views of UN Women, the United Nations or any of its affiliated organizations. Table of Contents 1. Summary and Key Findings .............................................................................................. 1 2. Background ............................................................................................................................ 2 3. Methodology and Profile of Sample ............................................................................... 4 4. Barriers to Women’s Land Ownership ......................................................................... 6 5. Women’s Land Ownership and Intra-Household Decision-Making ................ 17 6. Women’s Land Ownership and Children’s Outcomes .......................................... 19 7. Conclusion …………………….. ............................................................................................ -
Clbr291116.Pdf
Pradhan Mantri Gram Sadak Yojana Road List for attachment with Sanction Letter - District Wise Abstract State : Bihar Sanction Year : 2016-2017 Batch : 1 Collaboration : Regular PMGSY Sr.No. District No of Road Length MoRD Cost State Cost (Rs Total Cost Maint. Cost Habs (1000+, 500+, 250+, <250, Total) Works (Kms) / Bridge (Rs Lacs) Lacs) (Rs Lacs) (Rs Lacs) Length (Mtrs) 1 2 3 4 5 6 7 8 9 Road Proposals 1 Araria 14 53.847 2,028.42 1,352.29 3,380.71 359.41 (38 , 22 , 7 , 6 , 73) 2 Arwal 17 24.592 789.32 526.21 1,315.53 94.39 (2 , 8 , 9 , 0 , 19) 3 Aurangabad 98 247.119 7,472.00 4,981.32 12,453.32 769.17 (30 , 43 , 63 , 31 , 167) 4 Banka 51 154.415 4,878.39 3,252.27 8,130.66 901.54 (5 , 56 , 10 , 47 , 118) 5 Begusarai 6 7.749 202.83 135.22 338.05 22.97 (3 , 4 , 3 , 1 , 11) 6 Bhagalpur 9 30.252 974.39 649.59 1,623.98 190.73 (5 , 5 , 1 , 0 , 11) 7 Bhojpur 12 23.800 894.47 596.34 1,490.81 130.11 (5 , 9 , 1 , 0 , 15) 8 Buxar 5 9.990 395.39 263.61 659.00 58.31 (0 , 6 , 0 , 0 , 6) 9 Darbhanga 20 58.903 1,910.50 1,273.67 3,184.17 139.63 (30 , 23 , 22 , 24 , 99) 10 East Champaran 67 124.877 4,000.46 2,667.01 6,667.47 385.71 (32 , 50 , 22 , 32 , 136) 11 Gaya 200 311.574 8,617.98 5,745.35 14,363.33 1,149.84 (44 , 107 , 143 , 45 , 339) 12 Gopalganj 6 24.150 749.26 499.80 1,249.06 56.40 (0 , 7 , 0 , 0 , 7) 13 Jahanabad 15 19.397 556.53 371.02 927.55 73.72 (2 , 5 , 12 , 6 , 25) 14 Jamui 9 55.851 1,706.79 1,137.86 2,844.65 202.73 (0 , 1 , 14 , 58 , 73) 15 Kaimur (Bhabhua) 106 204.660 6,353.25 4,235.54 10,588.79 952.99 (7 , 45 , 93 , 41 , 186) 16 Katihar -

TACR: India: Preparing the Bihar State Highways II Project
Technical Assistance Consultant’s Report Project Number: 41629 October 2010 India: Preparing the Bihar State Highways II Project Prepared by Sheladia Associates, Inc. Maryland, USA For Road Construction Department Government of Bihar This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. (For project preparatory technical assistance: All the views expressed herein may not be incorporated into the proposed project’s design. TA No. 7198-INDIA: Preparing the Bihar State Highways II Project Final Report TTTAAABBBLLLEEE OOOFFF CCCOOONNNTTTEEENNNTTTSSS 1 INTRODUCTION .............................................................................................................................. 8 1.1 INTRODUCTION .............................................................................................................................. 8 1.2 PROJECT APPRECIATION............................................................................................................. 8 1.2.1 Project Location and Details 9 1.2.2 Road Network of Bihar 11 1.3 PERFORMANCE OF THE STUDY ................................................................................................ 14 1.3.1 Staff Mobilization 14 1.3.2 Work Shop 14 1.4 STRUCTURE OF THE FINAL REPORT ....................................................................................... 14 2 SOCIO ECONOMIC PROFILE OF PROJECT AREA .................................................................. -
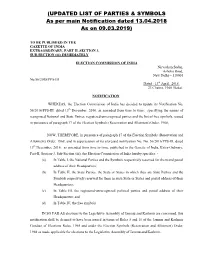
UPDATED LIST of PARTIES & SYMBOLS As Per Main Notification Dated 13.04.2018 As on 09.03.2019
(UPDATED LIST OF PARTIES & SYMBOLS As per main Notification dated 13.04.2018 As on 09.03.2019) TO BE PUBLISHED IN THE GAZETTE OF INDIA EXTRAORDINARY, PART II, SECTION 3, SUB-SECTION (iii) IMMEDIATELY ELECTION COMMISSION OF INDIA Nirvachan Sadan, Ashoka Road, New Delhi – 110001 No.56/2018/PPS-III Dated : 13th April, 2018. 23 Chaitra, 1940 (Saka). NOTIFICATION WHEREAS, the Election Commission of India has decided to update its Notification No. 56/2016/PPS-III, dated 13th December, 2016, as amended from time to time, specifying the names of recognised National and State Parties, registered-unrecognised parties and the list of free symbols, issued in pursuance of paragraph 17 of the Election Symbols (Reservation and Allotment) Order, 1968; NOW, THEREFORE, in pursuance of paragraph 17 of the Election Symbols (Reservation and Allotment) Order, 1968, and in supersession of its aforesaid notification No. No. 56/2016/PPS-III, dated 13th December, 2016, as amended from time to time, published in the Gazette of India, Extra-Ordinary, Part-II, Section-3, Sub-Section (iii), the Election Commission of India hereby specifies: - (a) In Table I, the National Parties and the Symbols respectively reserved for them and postal address of their Headquarters; (b) In Table II, the State Parties, the State or States in which they are State Parties and the Symbols respectively reserved for them in such State or States and postal address of their Headquarters; (c) In Table III, the registered-unrecognized political parties and postal address of their Headquarters; and (d) In Table IV, the free symbols. IN SO FAR AS elections to the Legislative Assembly of Jammu and Kashmir are concerned, this notification shall be deemed to have been issued in terms of Rules 5 and 10 of the Jammu and Kashmir Conduct of Elections Rules, 1965 and under the Election Symbols (Reservation and Allotment) Order, 1968 as made applicable for elections to the Legislative Assembly of Jammu and Kashmir.