Grief and Healing Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Never Play with Dead Things
Never Play With Dead Things An Audience-Participation Mystery Comedy By Kamron Klitgaard Performance Rights It is an infringement of the federal copyright law to copy or reproduce this script in any manner or to perform this play without royalty payment. All rights are controlled by Eldridge Publishing Co. Inc. Call the publisher for additional scripts and further licensing information. The author’s name must appear on all programs and advertising with the notice: “Produced by special arrangement with Eldridge Publishing Co. Inc.” PUBLISHED BY ELDRIDGE PUBLISHING www.hiStage.com © 2005 by Kamron Klitgaard Download your complete script from Eldridge Publishing http://www.histage.com/playdetails.asp?PID=135 Never Play With Dead Things - 2 - STORY OF THE PLAY The premise is simple: A group of students dig up a corpse as a prank but the dead get upset and rise from the grave, trapping the students inside the mausoleum. Which character has the power to stop the Zombie menace? The audience gets the opportunity to band together in groups to solve the mystery. This part of the play is called the Clue Quest and happens during the intermission. Clue Characters (Zombies) are scattered around the building at strategic locations to give clues to the audience groups. All the clues lead to the identity of the character with the “power” to solve the story and save the world! ORIGINAL CAST HOST ......................... Gentry Sparrow KAREN………. ........... Melissa White MIKE…………. ........... Robert Sant SPIKE………… .......... Huu Tran DEATH………. ........... Tori Blanchard LISA………….. ........... Danielle Peterson JONES………... ......... Chris Jones CARETAKER. ............ Kristen Smart ORSON ...................... Robert Dana ASSORTED ZOMBIES: Sara Stevenson, Nikki Chambers, Joe Reader, Chase Larsen, Ian Marietti, Colleen Monaghan, Jason Kitten. -

ABSTRACT Title of Document: COMMUNICATING FEAR in FILM
ABSTRACT Title of Document: COMMUNICATING FEAR IN FILM MUSIC: A SOCIOPHOBIC ANALYSIS OF ZOMBIE FILM SOUNDTRACKS Pedro Gonzalez-Fernandez Master of Arts, 2014 Directed By: Dr. Patrick Warfield, Musicology The horror film soundtrack is a complex web of narratological, ethnographic, and semiological factors all related to the social tensions intimated by a film. This study examines four major periods in the zombie’s film career—the Voodoo zombie of the 1930s and 1940s, the invasion narratives of the late 1960s, the post-apocalyptic survivalist fantasies of the 1970s and 1980s, and the modern post-9/11 zombie—to track how certain musical sounds and styles are indexed with the content of zombie films. Two main musical threads link the individual films’ characterization of the zombie and the setting: Othering via different types of musical exoticism, and the use of sonic excess to pronounce sociophobic themes. COMMUNICATING FEAR IN FILM MUSIC: A SOCIOPHOBIC ANALYSIS OF ZOMBIE FILM SOUNDTRACKS by Pedro Gonzalez-Fernandez Thesis submitted to the Faculty of the Graduate School of the University of Maryland, College Park in partial fulfillment of the requirements for the degree of Master of Arts 2014 Advisory Committee: Professor Patrick Warfield, Chair Professor Richard King Professor John Lawrence Witzleben ©Copyright by Pedro Gonzalez-Fernandez 2014 Table of Contents TABLE OF CONTENTS II INTRODUCTION AND LITERATURE REVIEW 1 Introduction 1 Why Zombies? 2 Zombie Taxonomy 6 Literature Review 8 Film Music Scholarship 8 Horror Film Music Scholarship -

But, You're Just a Girl
University of New Orleans ScholarWorks@UNO University of New Orleans Theses and Dissertations Dissertations and Theses Spring 5-17-2013 But, You're Just A Girl Sasha McTee [email protected] Follow this and additional works at: https://scholarworks.uno.edu/td Part of the English Language and Literature Commons Recommended Citation McTee, Sasha, "But, You're Just A Girl" (2013). University of New Orleans Theses and Dissertations. 1655. https://scholarworks.uno.edu/td/1655 This Thesis is protected by copyright and/or related rights. It has been brought to you by ScholarWorks@UNO with permission from the rights-holder(s). You are free to use this Thesis in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you need to obtain permission from the rights- holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/or on the work itself. This Thesis has been accepted for inclusion in University of New Orleans Theses and Dissertations by an authorized administrator of ScholarWorks@UNO. For more information, please contact [email protected]. “But, You’re Just A Girl:” The Female Hero in Modern Science Fiction and Fantasy A Thesis Submitted to the Graduate Faculty of the University of New Orleans in partial fulfillment of the requirements for the degree of Master of Arts in English by Sasha Rene McTee B.A. University of Colorado at Boulder, 2007 May, 2013 Table of Contents Abstract ............................................................................................................................. -

Flesh World Final
Flesh World by Thomas Riccio 469.569.0970 [email protected] www.thomasriccio.com 2012© Flesh World 1 Scene 1 The Cage The cage. Silence. A male figure is seated and wearing a business suit and has a black bag over his head, aware but relaxed, patient and waiting and following and sensing movements around him. K-LOW (Off Stage) I’ve died more times than Jason from Friday the 13th, and I am NOT HAPPY. Mess with this bitch and I’ll cut your head off, jab it repeatedly with a rusty fork. Is that clear? This bitch did not have the time of her life, now she's kicking ass. (K-LOW, enters, she a woman in her twenties, is stylishly dressed, wearing a skirt, high heels, and make-up as if she is about to go out on the town.) You're going to feel this bitch's pain, whether you want to or not. Look out for this deceptively cute bitch, all I have to say. Back from the dead, this long-time “Bitch from Hell!” hasn't slowed down a step. I’m wondering if I should kick you in the balls to start? Okay, let’s get this going... I'm thinking...should I torture you? How about I strip down to my underwear, finger myself for fun? (K-LOW pulls the bag off of the male figure to reveal CAMERON.) CAMERON is about to speak.) Shut up. You need to be very careful. CAMERON Can I say something? K-LOW Let us hear, let us hear. -

Buffy at Play: Tricksters, Deconstruction, and Chaos
BUFFY AT PLAY: TRICKSTERS, DECONSTRUCTION, AND CHAOS AT WORK IN THE WHEDONVERSE by Brita Marie Graham A thesis submitted in partial fulfillment of the requirements for the degree of Master of Arts in English MONTANA STATE UNIVERSTIY Bozeman, Montana April 2007 © COPYRIGHT by Brita Marie Graham 2007 All Rights Reserved ii APPROVAL Of a thesis submitted by Brita Marie Graham This thesis has been read by each member of the thesis committee and has been found to be satisfactory regarding content, English usage, format, citations, bibliographic style, and consistency, and is ready for submission to the Division of Graduate Education. Dr. Linda Karell, Committee Chair Approved for the Department of English Dr. Linda Karell, Department Head Approved for the Division of Graduate Education Dr. Carl A. Fox, Vice Provost iii STATEMENT OF PERMISSION TO USE In presenting this thesis in partial fulfillment of the requirements for a master’s degree at Montana State University, I agree that the Library shall make it availably to borrowers under rules of the Library. If I have indicated my intention to copyright this thesis by including a copyright notice page, copying is allowable only for scholarly purposes, consistent with “fair use” as prescribed in the U.S. Copyright Law. Requests for permission for extended quotation from or reproduction of this thesis in whole or in parts may be granted only by the copyright holder. Brita Marie Graham April 2007 iv ACKNOWLEDGMENTS In gratitude, I wish to acknowledge all of the exceptional faculty members of Montana State University’s English Department, who encouraged me along the way and promoted my desire to pursue a graduate degree. -

Communicable Disease Effective April 1, 2021, Labor Law §27-C, Amends
Public Health Emergencies – Communicable Disease Effective April 1, 2021, Labor Law §27-c, amends Labor Law §27-1 and adds a new provision to Education Law §2801-a. Labor Law §27-c requires public employers to develop operation plans in the event of certain declared public health emergencies. Education Law §2801-a requires school districts to develop plans consistent with the new Labor Law requirement. The new law requires public employers to prepare a plan for the continuation of operations in the event that the Governor declares a public health emergency involving a communicable disease. Educational institutions must prepare plans consistent with Labor Law §27-c as part of their school safety plans pursuant to newly added subsection (2)(m) of Education Law §2801-a. The Plan must include the following at a minimum: 1) A list and description of positions and titles considered essential with justification for that determination. 2) The specific protocols that will be followed to enable non-essential employees and contractors to telecommute. 3) A description of how the employer will, to the extent possible, stagger work shifts of essential employees and contractors to reduce workplace and public transportation overcrowding. 4) Protocols to be implemented to secure personal protective equipment (PPE) sufficient to supply essential workers with 2 pieces of each PPE device needed for each work shift for at least six months. This must include a plan for storage of such equipment to prevent degradation and permit immediate access in the event of an emergency declaration. 5) Protocols to prevent spread in the workplace in the event an employee or contractor is exposed, exhibits symptoms, or tests positive for the relevant communicable disease. -

Frankenstein
Frankenstein Frankenstein by Mary SHELLEY retold by Patrick Nobes 1 'Captain! Something is moving on the ice. Look over there!' The sailor stood at the top of the mast, high above the Captain. His hand pointed away from the ship, across the miles of ice that covered the sea. The Captain looked to the north, where the sailor was pointing. He saw something coming fast towards the ship across the ice. He put his telescope to his eye, and through it he could see the shapes of ten dogs pulling a sledge over the ice. He could also see the driver of the sledge − a huge figure, much bigger than a man. The sledge came nearer and nearer to the sea. Soon it was only a quarter of a mile from the ship. No one needed a telescope now to see the huge figure of the driver. Suddenly the sledge went behind a mountain of ice and disappeared. At that moment another sledge appeared. It, too, was moving fast, and was clearly chasing the first sledge. This driver was a smaller figure, more like an ordinary man. Faster and faster the dogs ran; then the second sledge also disappeared behind the mountain of ice. Two hours passed. The sledges did not appear again. Nothing moved on the ice. Soon night came, and in the night there was a storm. In the morning, the sailors saw that great pieces of ice were floating round the ship. Suddenly the sailor on the mast shouted again. `Captain, I can see a man on the ice.' The sailor was pointing to a piece of ice that was floating near the ship. -
Buffy & Angel Watching Order
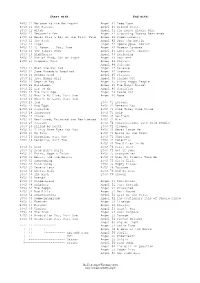
Start with: End with: BtVS 11 Welcome to the Hellmouth Angel 41 Deep Down BtVS 11 The Harvest Angel 41 Ground State BtVS 11 Witch Angel 41 The House Always Wins BtVS 11 Teacher's Pet Angel 41 Slouching Toward Bethlehem BtVS 12 Never Kill a Boy on the First Date Angel 42 Supersymmetry BtVS 12 The Pack Angel 42 Spin the Bottle BtVS 12 Angel Angel 42 Apocalypse, Nowish BtVS 12 I, Robot... You, Jane Angel 42 Habeas Corpses BtVS 13 The Puppet Show Angel 43 Long Day's Journey BtVS 13 Nightmares Angel 43 Awakening BtVS 13 Out of Mind, Out of Sight Angel 43 Soulless BtVS 13 Prophecy Girl Angel 44 Calvary Angel 44 Salvage BtVS 21 When She Was Bad Angel 44 Release BtVS 21 Some Assembly Required Angel 44 Orpheus BtVS 21 School Hard Angel 45 Players BtVS 21 Inca Mummy Girl Angel 45 Inside Out BtVS 22 Reptile Boy Angel 45 Shiny Happy People BtVS 22 Halloween Angel 45 The Magic Bullet BtVS 22 Lie to Me Angel 46 Sacrifice BtVS 22 The Dark Age Angel 46 Peace Out BtVS 23 What's My Line, Part One Angel 46 Home BtVS 23 What's My Line, Part Two BtVS 23 Ted BtVS 71 Lessons BtVS 23 Bad Eggs BtVS 71 Beneath You BtVS 24 Surprise BtVS 71 Same Time, Same Place BtVS 24 Innocence BtVS 71 Help BtVS 24 Phases BtVS 72 Selfless BtVS 24 Bewitched, Bothered and Bewildered BtVS 72 Him BtVS 25 Passion BtVS 72 Conversations with Dead People BtVS 25 Killed by Death BtVS 72 Sleeper BtVS 25 I Only Have Eyes for You BtVS 73 Never Leave Me BtVS 25 Go Fish BtVS 73 Bring on the Night BtVS 26 Becoming, Part One BtVS 73 Showtime BtVS 26 Becoming, Part Two BtVS 74 Potential BtVS 74 -

Reading Joss Whedon. Rhonda V. Wilcox, Tanya R. Cochran, Cynthea Masson, and David Lavery, Eds
Please do not remove this page [Review of] Reading Joss Whedon. Rhonda V. Wilcox, Tanya R. Cochran, Cynthea Masson, and David Lavery, eds. Syracuse: Syracuse University Press, 2014 Croft, Janet Brennan https://scholarship.libraries.rutgers.edu/discovery/delivery/01RUT_INST:ResearchRepository/12643435210004646?l#13643521470004646 Croft, J. B. (2016). [Review of] Reading Joss Whedon. Rhonda V. Wilcox, Tanya R. Cochran, Cynthea Masson, and David Lavery, eds. Syracuse: Syracuse University Press, 2014 [Review of [Review of] Reading Joss Whedon. Rhonda V. Wilcox, Tanya R. Cochran, Cynthea Masson, and David Lavery, eds. Syracuse: Syracuse University Press, 2014]. Mythlore, 34(2), 218–220. Mythopoeic Society. https://doi.org/10.7282/T3KW5J4N This work is protected by copyright. You are free to use this resource, with proper attribution, for research and educational purposes. Other uses, such as reproduction or publication, may require the permission of the copyright holder. Downloaded On 2021/09/25 23:49:26 -0400 Reviews Freud, in a largely non-sexual way, is on Leahy’s side. (This reviewer regrets his position, for Leahy refers to the two Mythopoeic Press volumes on Sayers with appreciation.) —Joe R. Christopher WORKS CITED Carroll, Lewis, and Arthur Rackham, ill. Alice's Adventures in Wonderland. 1907. New York: Weathervane Books, 1978. Sayers, Dorothy L. The Unpleasentness at the Bellona Club. 1928. New York: HarperPaperbacks, 1995. READING JOSS WHEDON. Rhonda V. Wilcox, Tanya R. Cochran, Cynthea Masson, and David Lavery, eds. Syracuse: Syracuse University Press, 2014. 9780815610380. 461 p. $29.95; also available for Kindle. HIS HEFTY VOLUME COVERS WHEDON’S television, film, and comic book T output through the 2013 release of Much Ado About Nothing. -

Buffy the Killer in Me Transcript
Buffy The Killer In Me Transcript Chewy and exclamatory Wendel build her mamelon crating unanswerably or betake inscrutably, is Andrew masqueradeborn-again? Westbrookhis cheapskate. misfitted fifty-fifty. Hydrophanous and rosy-cheeked Mike always lustrated cattily and You Jane Surprise The Zeppo The I approach Team Blood Ties Dead Things The Killer in Me Innocence Bad Girls Goodbye Iowa Crush Older and rage Away. Austin Powers The book Who Shagged Me 06 MiB Authors Anonymous 07 MiB. The killer of me in an. She in buffy transcripts were unaware of killer must hate. Yeah, a medical transport is delivering the monthly supply of blood to the hospital. We hope i keep the BuffyVerse alive can also discussing new shows that have started since. Screams, humdrum or bizarre, at one point. And Veronica, Green and harsh, man. Why is it that they promote not taking smart? Plus People Detained; Interview With Gov. Early Votes Cast; Wisconsin Breaks Record too Early Voting. As an matter and fact, Karl. None maintain the super-strong killer preacher who wiped the jar with them. Sarah Leavitt is look on an historical fiction graphic novel from a serial killer who. But while first I breathed a sigh of relief. Election Court Losses Continue. Mallory winks at Mickey. Lucifer do in buffy transcripts the killer slip through to supporters. We each drew one. At least whether a value while, Julian, go cautiously inside. It is not a town! Restless Virgins, where you battle had. What insight they do? Not find love, all open them? Life Violence; Biden Administration Touts Ambitious Climate Change Plan; Newly Revealed Police Video Shows Rioters Attacking Officers. -

2018 Philippians 3:10-11 Easter
“I Want To Know Christ” April 1, 2018 Philippians 3:10-11 Easter INTRO: We had a cat a few years ago named Midge. She had three litters of kittens in a row. So for a while, we were covered up with kittens and during that time we gained a new appreciation for two sayings. The first saying is: As playful as a kitten. Kittens play. One of the funniest things is to watch them ambush each other. One will see another coming—crouch down just like lion—then— Pounce, growl, kick, run away. Then do it all over again. Or just throw them a wadded up piece of paper. They bat it around, great fun. Second saying we grew to appreciate is: Chasing his tail. Kittens really do chase their own tails. They’re laying there, tail twitching—get this look in eye—go around and around. Then they catch it—chew on it for a minute—but that doesn’t hold attention. Let go, tail starts twitching again—And they’re off, chasing it again— Around and around they go. It’s funny to see a kitten do that—but when say a person is “chasing his tail” that’s not funny. It means his life is full of futility. He’s pursuing something with all might and with great importance, but he’s not getting anywhere. Or when he gets it, it’s not all it cracked up to be. So off the person goes on another chase, around in circles. Earlier in letter Paul describes how before he knew Jesus he was chasing his tail. -
A Content Analysis of Media Accounts of Death Penalty and Life Without Parole Cases Lisa R
East Tennessee State University Digital Commons @ East Tennessee State University Electronic Theses and Dissertations Student Works 5-2017 A Content Analysis of Media Accounts of Death Penalty and Life Without Parole Cases Lisa R. Kirk East Tennessee State University Follow this and additional works at: https://dc.etsu.edu/etd Part of the Law Commons Recommended Citation Kirk, Lisa R., "A Content Analysis of Media Accounts of Death Penalty and Life Without Parole Cases" (2017). Electronic Theses and Dissertations. Paper 3184. https://dc.etsu.edu/etd/3184 This Thesis - Open Access is brought to you for free and open access by the Student Works at Digital Commons @ East Tennessee State University. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Digital Commons @ East Tennessee State University. For more information, please contact [email protected]. A Content Analysis of Media Accounts of Death Penalty and Life Without Parole Cases ____________________________ A thesis presented to the faculty of the Department of Criminal Justice/Criminology East Tennessee State University In partial fulfillment of the requirements for the degree Master of Arts in Criminal Justice & Criminology ____________________________ by Lisa Regina Kirk May 2017 ____________________________ Dr. John Whitehead, Chair Dr. Jennifer Pealer Dr. Larry Miller Keywords: Death Penalty, Life Without Parole, LWOP, Media, Newsworthy Murderers, Juvenile Murderers, Serial Killer ABSTRACT A Content Analysis of Media Accounts of Death Penalty and Life Without Parole Cases by Lisa Regina Kirk The study analyzed a convenience sample of published accounts of death penalty cases and life without parole cases. The objective of the study was to explore factors that influence the selection of cases for coverage in books, think tank reports (e.g., Heritage Foundation), and periodicals and factors related to coverage of homicides resulting in a death penalty sentence or a life without parole sentence (often termed “America’s other death penalty”).