HUMIRA Is Administered by Subcutaneous Injection INITIAL DOSE FOLLOWED BY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy
Medical Coverage Policy Effective Date ............................................. 7/10/2021 Next Review Date ....................................... 3/15/2022 Coverage Policy Number .................................. 0554 Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy Table of Contents Related Coverage Resources Overview .............................................................. 1 Balloon Sinus Ostial Dilation for Chronic Sinusitis and Coverage Policy ................................................... 2 Eustachian Tube Dilation General Background ............................................ 3 Drug-Eluting Devices for Use Following Endoscopic Medicare Coverage Determinations .................. 10 Sinus Surgery Coding/Billing Information .................................. 10 Rhinoplasty, Vestibular Stenosis Repair and Septoplasty References ........................................................ 28 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence -

672 Rapid Development of Visual Field Defects Associated with Vigabatrin Therapy
Case report The incidence of penetrating injury is thought in part to be due to globe shape, with myopic eyes being at A 64-year-old woman presented to eye casualty with a greater risk. Vohra and Good7 suggest, however, that a second episode of right dacryocystitis. The visual acuity medial canthal approach is the safest, especially in larger was 6/6 bilaterally. She was given a 7 day course of oral globes? This is because of a reduction in the equatorial amoxicillin 500 mg t.d.s. with flucloxacillin 250 mg q.d.s. width to axial length ratio in high degrees of axial and was reviewed when the infection had settled. myopia. Inflammation of the tissues surrounding the Syringing showed patent canaliculi with regurgitation usual landmarks, for example following dacryocystitis, and she was listed for dacryocystorhinostomy (DCR) as in this patient, can alter the anatomy of the injection under local anaesthesia. site and increase the risk of perforation. MeyerS reports In the anaesthetic room the patient was sedated with some success with topical anaesthetic techniques which 2.5 mg of intravenous midazolam. Two drops of would eliminate the risk of penetrating ocular injury. amethocaine were instilled into both eyes. Two puffs of Early diagnosis and treatment of ocular perforations 2% lignocaine spray were applied to the right nasal are essential for a good visual outcome6,9 and therefore passage. A nasal pack of 5% cocaine with adrenaline was there should be a high index of suspicion in those cases placed in the right nasal antrum. A local anaesthetic where the injections are excessively painful, or mixture containing 4 ml of 2% lignocaine with 1:200 000 ineffective, or if there is hypotony of the globe or a adrenaline and 4 ml of 0.75% bupivacaine was decrease in visual acuity. -

Quality of Vision in Eyes with Epiphora Undergoing Lacrimal Passage Intubation
Quality of Vision in Eyes With Epiphora Undergoing Lacrimal Passage Intubation SHIZUKA KOH, YASUSHI INOUE, SHINTARO OCHI, YOSHIHIRO TAKAI, NAOYUKI MAEDA, AND KOHJI NISHIDA PURPOSE: To investigate visual function and optical PIPHORA, THE MAIN COMPLAINT OF PATIENTS WITH quality in eyes with epiphora undergoing lacrimal passage lacrimal passage obstruction, causes blurred vision, intubation. discomfort, and skin eczema, and may even cause so- E DESIGN: Prospective case series. cial embarrassment. Several studies have assessed the qual- METHODS: Thirty-four eyes of 30 patients with ity of life (QoL) or vision-related QoL of patients suffering lacrimal passage obstruction were enrolled. Before and from lacrimal disorders and the impact of surgical treat- 1 month after lacrimal passage intubation, functional vi- ments on QoL, using a variety of symptom-based question- sual acuity (FVA), higher-order aberrations (HOAs), naires.1–8 According to these studies, epiphora negatively lower tear meniscus, and tear clearance were assessed. affects QoL physically and socially; however, surgical An FVA measurement system was used to examine treatment can improve QoL. Increased tear meniscus changes in continuous visual acuity (VA) over time, owing to inadequate drainage contributes to blurry and visual function parameters such as FVA, visual main- vision.9 However, quality of vision (QoV) has not been tenance ratio, and blink frequency were obtained. fully quantified in eyes with epiphora, and the effects of Sequential ocular HOAs were measured for 10 seconds lacrimal surgery on such eyes are unknown. after the blink using a wavefront sensor. Aberration Dry eye, a clinically significant multifactorial disorder of data were analyzed in the central 4 mm for coma-like, the ocular surface and tear film, may cause visual distur- spherical-like, and total HOAs. -

Primary External Dacryocystorhinostomy
11 Primary External Dacryocystorhinostomy Richard H. Hart, Suzanne Powrie, and Geoffrey E. Rose The watering eye may be the result of excessive tear production, abnor- malities of lid position or movement, lacrimal canalicular pump failure, or obstruction of the outfl ow tract. With external dacryocystorhinos- tomy (DCR), the lacrimal sac is directly incorporated into the lateral wall of the nose, so that the canaliculi drain directly into the nasal cavity. The aims of surgery are twofold: to eliminate fl uid and mucus reten- tion within the lacrimal sac and prevent sac enlargement (as a muco- cele) – the latter leading to intermittent viscous ocular discharge – and to bypass the higher hydraulic resistance of the nasolacrimal duct, thereby increasing tear conductance and aiding the relief of epiphora. Indications for Surgery 1. Primary acquired nasolacrimal duct obstruction 2. Secondary acquired nasolacrimal duct obstruction attributed, for example, to dacryolithiasis, endonasal surgery, infl ammatory nasal or sinus disease, or prior midfacial injury 3. Persistent congenital nasolacrimal duct obstruction, often after unsuccessful probing or intubation of the nasolacrimal duct 4. Functional obstruction of lacrimal outfl ow with decreased tear conductance as a result of: (a) Stenosis, but not occlusion, of the nasolacrimal duct (b) Lacrimal canalicular pump failure from age-related laxity of the lower eyelid, or after facial nerve palsy 5. Acute or chronic dacryocystitis; the former group requiring initial treatment with systemic antibiotics Surgical Principles External DCR should establish a low-resistance drainage pathway between the conjunctival tear sac and the nasal cavity, by conversion of the lacrimal sac into part of the lateral nasal wall. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

1 Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL
Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL BIFURCATION OCT06- 0201 LINEAR CRANIECTOMY 0050 IMPL CRT PACEMAKER SYS 0202 ELEVATE SKULL FX FRAGMNT 0051 IMPL CRT DEFIBRILLAT SYS 0203 SKULL FLAP FORMATION 0052 IMP/REP LEAD LF VEN SYS 0204 BONE GRAFT TO SKULL 0053 IMP/REP CRT PACEMAKR GEN 0205 SKULL PLATE INSERTION 0054 IMP/REP CRT DEFIB GENAT 0206 CRANIAL OSTEOPLASTY NEC 0056 INS/REP IMPL SENSOR LEAD OCT06- 0207 SKULL PLATE REMOVAL 0057 IMP/REP SUBCUE CARD DEV OCT06- 0211 SIMPLE SUTURE OF DURA 0061 PERC ANGIO PRECEREB VES (OCT 04) 0212 BRAIN MENINGE REPAIR NEC 0062 PERC ANGIO INTRACRAN VES (OCT 04) 0213 MENINGE VESSEL LIGATION 0066 PTCA OR CORONARY ATHER OCT05- 0214 CHOROID PLEXECTOMY 0070 REV HIP REPL-ACETAB/FEM OCT05- 022 VENTRICULOSTOMY 0071 REV HIP REPL-ACETAB COMP OCT05- 0231 VENTRICL SHUNT-HEAD/NECK 0072 REV HIP REPL-FEM COMP OCT05- 0232 VENTRI SHUNT-CIRCULA SYS 0073 REV HIP REPL-LINER/HEAD OCT05- 0233 VENTRICL SHUNT-THORAX 0074 HIP REPL SURF-METAL/POLY OCT05- 0234 VENTRICL SHUNT-ABDOMEN 0075 HIP REP SURF-METAL/METAL OCT05- 0235 VENTRI SHUNT-UNINARY SYS 0076 HIP REP SURF-CERMC/CERMC OCT05- 0239 OTHER VENTRICULAR SHUNT 0077 HIP REPL SURF-CERMC/POLY OCT06- 0242 REPLACE VENTRICLE SHUNT 0080 REV KNEE REPLACEMT-TOTAL OCT05- 0243 REMOVE VENTRICLE SHUNT 0081 REV KNEE REPL-TIBIA COMP OCT05- 0291 LYSIS CORTICAL ADHESION 0082 REV KNEE REPL-FEMUR COMP OCT05- 0292 BRAIN REPAIR 0083 REV KNEE REPLACE-PATELLA OCT05- 0293 IMPLANT BRAIN STIMULATOR 0084 REV KNEE REPL-TIBIA LIN OCT05- 0294 INSERT/REPLAC SKULL TONG 0085 RESRF HIPTOTAL-ACET/FEM -

Rvs Code Description Annex 7. List of Procedures with Laterality
ANNEX 7. LIST OF PROCEDURES WITH LATERALITY RVS CODE DESCRIPTION 15820 Blepharoplasty, lower eyelid 15822 Blepharoplasty, upper eyelid; 15823 Blepharoplasty, upper eyelid; with excessive skin weighting down lid 19160 Mastectomy, partial; 19162 Mastectomy, partial; with axillary lymphadenectomy 19180 Mastectomy, simple, complete 19182 Mastectomy, subcutaneous 19200 Mastectomy, radical, icnluding pectoral muscles, axillary lymph nodes 19220 Mastectomy, radical, including pectoral muscles, axillary and internal mammary lymph nodes (Urban type operation) Mastectomy, modified radical, including axillary lymph nodes, w/ or w/o pectoralis minor muscle, but excluding pectoralis major 19240 muscle 19340 Immediate insertion of breast prosthesis following mastopexy, mastectomy or in reconstruction 19342 Delayed insertion of breast prosthesis following mastopexy, mastectomy or in reconstruction 19350 Nipple/areola reconstruction 19357 Breast reconstruction, immediate or delayed, with tissue expander, including subsequent expansion 19361 Breast reconstruction with latissimus dorsi flap, with or without prosthetic implant 19364 Breast reconstruction with free flap 19366 Breast reconstruction with other technique 19367 Breast reconstruction with transverse rectus abdominis myocutaneous flap (TRAM), single pedicle, including closure of donor site; 19369 Breast reconstruction with transverse rectus abdominis myocutaneous flap (TRAM), double pedicle, including closure of donor site 19370 Open periprosthetic capsulotomy, breast 19371 Periprosthetic capsulectomy, -

Ophthalmology
LECTURE NOTES For Health Science Students Ophthalmology Dereje Negussie, Yared Assefa, Atotibebu Kassa, Azanaw Melese University of Gondar In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education 2004 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2004 by Dereje Negussie, Yared Assefa, Atotibebu Kassa, Azanaw Melese All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. PREFACE This lecture note will serve as a practical guideline for the hard-pressed mid-level health workers. We hope that it will be a good introduction to eye diseases for health science students working in Ethiopia. -
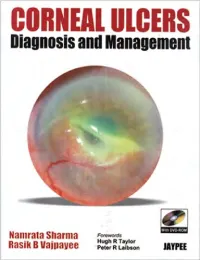
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Usability and Reproducibility of Tear Meniscus Values Generated Via Swept-Source Optical Coherence Tomography and the Slit Lamp with a Graticule Method
Int Ophthalmol DOI 10.1007/s10792-017-0517-3 ORIGINAL PAPER Usability and reproducibility of tear meniscus values generated via swept-source optical coherence tomography and the slit lamp with a graticule method Hitoshi Imamura . Hitoshi Tabuchi . Shunsuke Nakakura . Daisuke Nagasato . Hiroaki Baba . Yoshiaki Kiuchi Received: 24 October 2016 / Accepted: 4 April 2017 Ó The Author(s) 2017. This article is an open access publication Abstract each method (ICC [ 0.75 for both). No statistically Purpose To investigate the usability and the repro- significant differences were found in TMH among the ducibility of the tear meniscus values via swept-source age groups using both SS-OCT and slit lamp methods optical coherence tomography (SS-OCT) and the (P = 0.985, 0.380, respectively). TMH values at both conventional slit lamp microscope method with a sides of the corneal center were significantly smaller graticule. than those at the corneal center (P \ 0.0001). Methods The right eye was examined in 90 healthy Conclusions TMH values obtained by the slit lamp adult subjects who were grouped according to age method were lower than those obtained by SS-OCT. (group 1: 20–39 years; group 2: 40–59 years; group 3: However, both methods yielded highly reproducible C60 years). The tear meniscus height (TMH) and tear TMH measurements, suggesting that they are clini- meniscus area were measured using SS-OCT and cally useful. Tear meniscus values did not vary by age TMH by the slit lamp microscope method. The but by measurement points in our cohort. reproducibility of each method was calculated using intraclass correlation coefficients (ICCs) in addition- Keywords Tear meniscus Á Slit lamp Á SS-OCT Á ally enrolled 30 healthy young subjects. -

What's New and Important in Pediatric Ophthalmology and Strabismus In
What’s New and Important in Pediatric Ophthalmology and Strabismus in 2021 Complete Unabridged Handout AAPOS Virtual Meeting April 2021 Presented by the AAPOS Professional Education Committee Tina Rutar, MD - Chairperson Austin E Bach, DO Kara M Cavuoto, MD Robert A Clark, MD Marina A Eisenberg, MD Ilana B Friedman, MD Jennifer A Galvin, MD Michael E Gray, MD Gena Heidary, MD PhD Laryssa Huryn, MD Alexander J Khammar MD Jagger Koerner, MD Eunice Maya Kohara, DO Euna Koo, MD Sharon S Lehman, MD Phoebe Dean Lenhart, MD Emily A McCourt, MD - Co-Chairperson Julius Oatts, MD Jasleen K Singh, MD Grace M. Wang, MD PhD Kimberly G Yen, MD Wadih M Zein, MD 1 TABLE OF CONTENTS 1. Amblyopia page 3 2. Vision Screening page 12 3. Refractive error page 20 4. Visual Impairment page 31 5. Neuro-Ophthalmology page 37 6. Nystagmus page 48 7. Prematurity page 52 8. ROP page 55 9. Strabismus page 65 10. Strabismus surgery page 82 11. Anterior Segment page 101 12. Cataract page 108 13. Cataract surgery page 110 14. Glaucoma page 120 15. Refractive surgery page 127 16. Genetics page 128 17. Trauma page 151 18. Retina page 156 19. Retinoblastoma / Intraocular tumors page 167 20. Orbit page 171 21. Oculoplastics page 175 22. Infections page 183 23. Pediatrics / Infantile Disease/ Syndromes page 186 24. Uveitis page 190 25. Practice management / Health care systems / Education page 192 2 1. AMBLYOPIA Self-perception in Preschool Children With Deprivation Amblyopia and Its Association With Deficits in Vision and Fine Motor Skills. Birch EE, Castaneda YS, Cheng-Patel CS, Morale SE, Kelly KR, Wang SX. -

I Can Confirm That Case 1 Had Both a Central 24/2 Humphrey Visual Field and the Standard DVLA Binocular Esterman Visual Field Te
Correspondence 546 I can confirm that Case 1 had both a central 24/2 myopic astigmatism and anisometropia. Syringing and Humphrey visual field and the standard DVLA probing of the tear passages under general anaesthetic binocular Esterman visual field test. As you mention, confirmed the presence of bilateral lacrimal sac Case 1 passed her driving test without being aware of mucocoeles with bony nasolacrimal duct obstruction at any field defect. With regard to Case 2, I am unable to 28 mm from the puncta in the right and 25 mm in the left. trace any disc photographs. I was in touch with the A dacryocystogram confirmed dilated lacrimal drainage DVLA and their ophthalmological advisers regarding systems bilaterally. Bilateral external DCRs without tubes Case 1 and can report that her driving licence was produced a complete resolution of his symptoms. Figure returned to her approximately 6 months ago, after a great 1 shows the patient following the right DCR and before deal of negotiation. the left DCR. We hope that the recent modifications in field He was born at 32 weeks gestation with a birthweight standards proposed by the DVLA, dated 7.7.02, will of 1.69 kg. His mother had epilepsy (treated with sodium reduce the risk of peremptory loss of licence and valproate), smoked cigarettes, and was a nondrinker. On livelihood in the future. examination he was found to have hypotonia, developmental delay, and dysmorphic facial features SEP Burgess including a broad nasal bridge, congested face, narrow palpebral fissures, low-set ears and redundant skin folds Princess Margaret Hospital on his forehead (Figure 1).