An Update on Research to Understand And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mix-And-Match of Vaccines Will Definitely Not Cause a Safety Issue”
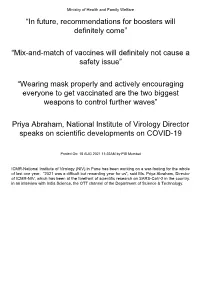
Ministry of Health and Family Welfare “In future, recommendations for boosters will definitely come” “Mix-and-match of vaccines will definitely not cause a safety issue” “Wearing mask properly and actively encouraging everyone to get vaccinated are the two biggest weapons to control further waves” Priya Abraham, National Institute of Virology Director speaks on scientific developments on COVID-19 Posted On: 18 AUG 2021 11:22AM by PIB Mumbai ICMR-National Institute of Virology (NIV) in Pune has been working on a war-footing for the whole of last one year. “2021 was a difficult but rewarding year for us”, said Ms. Priya Abraham, Director of ICMR-NIV, which has been at the forefront of scientific research on SARS-CoV-2 in the country. in an interview with India Science, the OTT channel of the Department of Science & Technology. Giving a quick overview of vaccine development process carried out at the institute which has been at the forefront of scientific research on SARS-CoV-2 in the country, she explained: “We quickly isolated and gave a strain to Bharat Biotech International Limited (BBIL) by the end of April (2020), after which they developed a whole virion-inactivated vaccine in the month of May and gave us back for review. We checked it for its complete inactivation, did its complete characterisation and started pre-clinical trials on hamsters and non-human primates, that is, monkeys. Those are very difficult experiments to do. These were conducted in our highest Bio-Safety Level-4 level containment facilities. In the next phase, we assisted them in the Phase I, II and III clinical trials in areas such as diagnostic aspect and laboratory support”. -

US and International Responses to the Global Spread of Avian
Order Code RL33219 CRS Report for Congress Received through the CRS Web U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Updated January 11, 2006 Tiaji Salaam-Blyther and Emma Chanlett-Avery Coordinators Foreign Affairs, Defense, and Trade Division Congressional Research Service ˜ The Library of Congress U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Summary One strain of avian influenza currently identified in Asia and Europe is known as Influenza A/H5N1. Although it is a bird flu, it has infected a relatively small number of people — killing around 50% of those infected. Scientists are concerned that H5N1 may cause the next influenza pandemic. Flu pandemics have occurred cyclically, roughly between every 30 and 50 years. Since 1997, when the first human contracted H5N1 in Hong Kong, the virus has resurfaced and spread to more than a dozen countries in Asia and Europe — infecting more than 140 people and killing approximately half. Britain and Taiwan both reported avian flu cases of H5N1 in 2005. In the latter cases, the infected birds were identified as imports, and died in quarantine. A global influenza pandemic could have a number of consequences. Global competition for existing vaccines and treatments could ensue. Some governments might restrict the export of vaccines or other supplies in order to treat their own population. Some countries might face a shortage of vaccines, antiviral medication, or other medical equipment, because of limited global supply. Hospitality and airline industries, and international trade could be negatively impacted. If global travel and trade were to suddenly drop, there could be productivity losses and service disruptions. -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -

ESCMID Online Lecture Library © by Author
Albert Osterhaus Head Dept Virology Chairman ESWI CSO Viroclinics-Biosciences BV Library Pandemic flu and the anti-H1N1 vaccine: Lecture a retrospective view. author Onlineby © ESCMID ESCMID conference on the impact of vaccines on Public Health Prague, 2nd April 2011 Human influenza: three appearances Library Seasonal influenza (A: H3N2, H1N1; B) Lecture Avian influenza author (A: H7N7, H5N1…)Online by © PandemicESCMID influenza (A: H1N1, H2N2, H3N2, H1N1…?) INFLUENZA A VIRUS Recent zoonotic transmissions Library Subtype Country Year # Cases # Deaths H7N7 UK Lecture1996 1 0 H5N1 Hongkong 1997 18 6 H9N2 SE-Asia 1999author >2 0 H5N1 HongkongOnlineby 2003 2? 1 H7N7 Netherlands© 2003 89 1 H7N2 USA 2003 1 0 H7N3 Canada 2004 2 0 H5N1ESCMIDSE-Asia/M-East/ 2003-11 .>500 >300* Europe/W-Africa *CFR ~ 60% Library Lecture author Onlineby © ESCMID Confirmed H5N1 avian influenza virus endemic areas (poultry and wild birds) since 2003 Avian influenza A H5N1 virus - HA: Receptor specificity - Library Shinya et al., Nature 440, 2006 Lecture Van Riel et al., Science 2006 author Van Riel et al., Online Am J Pathol 2007 by Van Riel et al., © Am J Pathol 2009 Van Riel et al., ESCMID Am J Pathol 2010 Library Lecture author Onlineby © ESCMID Introduction - Attachment to the upper respiratory tract - Seasonal H3N2 Pandemic H1N1 HPAIV H5N1 Last four pandemics Library Lecture Credit: US National Museum of Health and Medicine author 1918 1957Online 1968 2009 “Spanish Flu” “Asian Flu” by “Hong Kong Flu” © ”Swine Flu” >40 million deaths 1-4 million deaths 1-4million deaths ??? A(H1N1)ESCMIDA(H2N2) A(H3N2) A(H1N1) Library Lecture author Onlineby © ESCMID Air traffic from Mexico ~ 1998 PB2,PA: Triple reassortant ~ 1968 ~ 1998 PB1: LibraryN-America ~ 1918 Classical swine HA, NP, NS: Lecture ~ 1979 NA, MA: authorEurasian swine Eurasia Onlineby A/California/4/2009 © PB2 PB1 The H1N1v flu virus PA Courtesy: Ron Fouchier HA NP ESCMID NA MA NS Library Lecture author Onlineby © ESCMID The Mexican flu virus.. -

Options for the Use of Human H5N1 Influenza Vaccines and the WHO H5N1 Vaccine Stockpile
Options for the use of human H5N1 influenza vaccines and the WHO H5N1 vaccine stockpile THIRD DRAFT – 02/11/07 WHO SCIENTIFIC CONSULTATION: TECHNICAL CONSIDERATIONS FOR DEVELOPING OPTIONS FOR USE OF HUMAN H5N1 INFLUENZA VACCINES AND A WHO H5N1 VACCINE STOCKPILE GENEVA, 01-03 OCTOBER 2007 GENEVA, 2007 CONTENTS Executive summary ................................................................................................... 3 1. Characteristics of human H5N1 influenza vaccines 1.1: Safety......................................................................................................................... 8 1.2: Immunogenicity....................................................................................................... 10 1.3: Cross-reactivity........................................................................................................ 12 1.4: Degree and duration of protection ........................................................................... 13 1.5: Conclusions and priority areas ................................................................................ 14 2. Options for using human H5N1 influenza vaccines................................ 16 2.1: To protect people at high risk of contracting zoonotic avian H5N1 influenza........ 17 2.2: To “prime” selected groups or whole populations in anticipation of a possible H5N1 influenza pandemic ....................................................................................... 18 2.3: To immunize selected groups or whole populations in anticipation of -

(H5N1) Virus © World Health Organization 2006
WHO/PSM/PAR/2006.6 WHO Rapid Advice Guidelines on pharmacological management of humans infected with avian influenza A (H5N1) virus © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

MEDICAL COUNTERMEASURES Status of Supplies and Distribution/Allocation Systems
MEDICAL COUNTERMEASURES Status of Supplies and Distribution/Allocation Systems Prepared by Divya Hosangadi CAPS Antiviral • In addition to vaccines, monovalent antibody therapies and antivirals have been investigated for treating coronavirus infections (Table 1). • In this scenario, extranavir is a FICTIONAL antiviral drug. o Extranavir is currently used to treat HIV but has been shown to be an effective treatment for CAPS. o Extranavir may be an effective prophylactic if given throughout a period of possible exposure to the virus. o When used as a therapeutic, extranavir may reduce the severity of disease and length of viral shedding in infected individuals. o Extranavir is a generic drug that is manufactured in 5 countries, including the US and China. o About 1 million people per day take extranavir to treat HIV. o If all extranavir users were switched to a different HIV treatment, current supplies of the antiviral could treat up to 26 million CAPS patients. o It may be possible to double production of extranavir by expanding existing manufacturing capacity and by licensing the drug to additional manufacturers. This expansion could allow for 52 million treatment courses per year but would likely require a year to reach that capacity. o If extranavir were used broadly as a prophylactic rather than a treatment, a much greater supply of the drug would be needed. Current Vaccines in Development • There are no vaccines currently licensed and available for use against any coronavirus. Coronavirus vaccines for SARS and MERS have been technically challenging to develop and have not made it out of clinical trials.1-3 • While scientists are researching a vaccine against the FICTIONAL CAPS virus, there is currently no product in development. -

Early Efficacy from Covid-19 Phase 3 Vaccine Studies
Emerging Challenges to the Development of Covid-19 Vaccines Clinical Development & Operations SWAT Team | Thursday January 28, 2021 Workshop Agenda Time (CET) Topic Speaker(s) 15:00 – 15:10 Welcome & Meeting Objectives Peter Dull PART 1: Path to approval of additional Covid-19 vaccines Status of EUA/Licensure and vaccine use globally and key updates from previous workshops, 15:15 – 15:35 Peter Dull including correlates of protection 15:35 – 15:45 The ethics of placebo-controlled COVID-19 efficacy studies when vaccines are available Joseph Millum Placebo-controlled efficacy studies: Possibilities and Challenges – Alternative trial designs Alan Fix & 15:45 – 16:05 based on clinical endpoints and non-inferiority assessment based on immunogenicity Dean Follmann Phase 4 clinical studies: post authorization study designs to support accelerated or conditional 16:05 – 16:15 Daniel Feikin approvals Moderated by: 16:15 – 16:45 PANEL DISCUSSION: Practical paths to approval of vaccines still in development Peter Dull 16:45 – 16:50 Break Privileged and confidential 2 Workshop Agenda continued Time (CET) Topic Speaker(s) PART 2: Clinical development gaps – optimizing vaccination schedules for currently available Covid-19 vaccines Post-infection and vaccine-induced immune responses against SARS-CoV-2: summary of 17:00 – 17:15 Shabir Madhi impact of new variants 17:15 – 17:30 Heterologous prime-boost & prolonged dosing interval: Immunologic considerations Arnaud Didierlaurent 17:30 – 17:45 Comparing COVID-19 Vaccine Schedule Combinations (Com-COV) Matthew -

Flubytes June 28, 2013
FluBytes June 28, 2013 Michigan Department of Community Health, 201 Townsend Street, Lansing, MI 48933 VACCINE RECOMMENDATION FOR EGG-ALLERGIC PERSONS FIRST VARIANT INFLUENZA A H3N2 CASES IN 2013 OnFor June additional 20, the flu Advisory information Committee visit: www.michigan.gov/flu on Immunization Indiana state health officials have reported four cases of Practices (ACIP) voted in favor of recommending FluBlok human infection with H3N2 variant virus (H3N2v). These are during the 2013-14 flu season for persons 18-49 years with the first H3N2v cases reported for 2013. All four visited a egg allergy of any severity. FluBlok is the only vaccine that county agricultural fair in June before they got sick, and at is completely egg-free. The CDC media advisory can be least two had contact with pigs. found here. ISDH press release: Health officials encourage Hoosiers to protect themselves from swine flu 2012 MICHIGAN BEHAVIORAL RISK FACTOR SURVEY CIDRAP: Indiana reports four fair-linked H3N2v cases Data from the 2012 MI Behavioral Risk Factor Survey (MiBRFS) have been released. Results include the percent of CDC: Influenza A (H3N2) variant virus adults aged 65 years and older who received flu vaccine in the past year or ever received pneumococcal vaccine. In INFLUENZA-RELATED JOURNAL ARTICLES A study team, including researchers at the University of 2012, 55.4% of adults 65 and older received a flu shot, down Michigan, used a computerized model of pneumonia from 58.0% in 2011. transmission and found a 100-fold increase in risk of MICHIGAN IMMUNIZATION TIMELY TIPS NEWSLETTER pneumococcal pneumonia during the week after flu The May/June issue of the Michigan Immunization Timely infection. -

Package Insert
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------WARNINGS AND PRECAUTIONS---------------------- These highlights do not include all the information needed to use • Hypersensitivity reactions can occur. Appropriate medical treatment and AUDENZ™ (Influenza A (H5N1) Monovalent Vaccine, supervision must be available to manage possible anaphylactic reactions Adjuvanted) safely and effectively. See full prescribing information for following administration of the vaccine. (5.1) AUDENZ. • If Guillain-Barré syndrome has occurred within 6 weeks of receipt of a prior influenza vaccine, the decision to give AUDENZ should be based on AUDENZ (Influenza A (H5N1) Monovalent Vaccine, Adjuvanted) careful consideration of potential benefits and risks. (5.2) injectable emulsion for intramuscular use ------------------------------ADVERSE REACTIONS------------------------------- Initial U.S. Approval: 2020 • In adults 18 through 64 years of age, the most common (≥ 10%) solicited local and systemic reactions reported in clinical trials were injection site -----------------------------INDICATIONS AND USAGE-------------------------- pain (64%), fatigue (25%), headache (25%), malaise (22%), myalgia AUDENZ is an inactivated vaccine indicated for active immunization for the (14%), arthralgia (10%), and nausea (10%). (6.1) prevention of disease caused by the influenza A virus H5N1 subtype • In adults 65 years of age and older, the most common (≥ 10%) solicited contained in the vaccine. AUDENZ is approved for use in persons 6 months local and systemic reactions reported in clinical trials were injection site of age and older at increased risk of exposure to the influenza A virus H5N1 pain (36%), fatigue (20%), malaise (16%), headache (16%), and arthralgia subtype contained in the vaccine. (1) (10%). (6.1) Use in persons 6 months through 17 years of age is approved under • In infants and children, 6 months through 5 years of age, the most common accelerated approval based on the immune response elicited by AUDENZ. -

An Overview of Coronavirus (COVID-19) Drugs and Recent Status of Vaccine Trials
Journal of Clinical and Cellular Immunology Research article An Overview of Coronavirus (COVID-19) Drugs and Recent Status of Vaccine Trials Ayan Raichaudhuri* Department of Biotechnology, Amity University, Kolkata, India ABSTRACT A flare-up identified with the serious intense respiratory disorder coronavirus 2 (SARS-CoV-2) was first reported in Wuhan, China in December 2019. An incredibly high potential for scattering came about in the worldwide coronavirus illness 2019 (COVID-19) pandemic in 2020. Regardless of the exacerbating patterns of COVID-19, no medications are approved to have huge viability in the clinical treatment of COVID-19 patients in enormous scope examines. Remdesivir is viewed as the most encouraging antiviral operator; it works by repressing the movement of RNA-subordinate RNA polymerase (RdRp). The other superb enemy of flu RdRp inhibitor favipiravir is likewise being clinically assessed for its adequacy in COVID-19 patients. The protease inhibitor lopinavir/ritonavir (LPV/ RTV) alone isn't appeared to give preferable antiviral adequacy over standard consideration. Another promising option is hydroxychloroquine (200 mg threefold day by day) in addition to azithromycin (500 mg on day 1, trailed by 250 mg once every day on day 2-5), which indicated fantastic clinical adequacy on Chinese COVID-19 patients and hostile to SARS-CoV-2 intensity in vitro. The jobs of teicoplanin (which hinders the viral genome introduction in the cytoplasm) and monoclonal and polyclonal antibodies in the treatment of SARS-CoV-2 are under scrutiny. Staying away from the remedy of non-steroidal calming drugs, angiotensin changing over protein inhibitors, or angiotensin II type I receptor blockers is exhorted for COVID-19 patients. -

Supplemental 1 (PDF)
Supplemental Table 1. Summary of Formulations and Subtype Target in Influenza Vaccine Pandemic Clinical Trials. Adapted from the WHO, “Pandemic and Potentially Pandemic Viruses.” (165) Inactivated Whole Inactivated Inactivated Live Viral Virus Split Virus Subunit Attenuated Recombinant Vector DNA Peptide Undefined Total H1N1 20 251 84 26 14 36 431 H2N2 1 2 3 H3N2 1 2 1 6 1 11 H5N1 43 64 29 6 9 5 5 161 H5N2 2 9 11 H5N3 7 7 H6N1 1 1 H7N1 4 4 H7N3 3 3 H7N7 1 1 2 4 H7N9 8 1 7 4 1 21 H9N2 7 1 8 Non- 6 1 4 11 specific Total 73 330 124 57 33 11 8 4 36 676 Supplemental Table 2. Current Phase III SARS-CoV-2 Vaccine Candidates Phase Previous # of Doses Storage Developer Vaccine III Platform Vaccine Antigen Clinical Trial #s References (Days) Temp. Efficacy Use Anhui Zhifei Longcom Adjuvanted NCT04445194, Biopharmaceutical/ Protein RBD- 2 or 3 NCT04466085, Institute of ZF2001 MERS 2-8o C (1) subunit Dimer NCT04550351, Microbiology, Chinese NCT04646590 Academy of Sciences Bharat Biotech/ Indian CTRI/2020/07/026300, Council of Medical NCT04471519, Research/ National COVAXIN Inactivated Whole- 2 2-8o C CTRI/2020/09/027674, (2) Institute of Virology/ (BBV152) virus virion CTRI/2020/11/028976, Ocugen/ Precisa NCT04641481 Medicamentos ChiCTR2000030906, ChiCTR2000031781, NCT04313127, CanSino Biologics/ NCT04341389, Non- Beijing Institute of S NCT04398147, Ad5-nCoV replicating Ebola 1 2-8o C (3, 4) Biotechnology/ protein NCT04526990, viral vector Petrovax NCT04540419, NCT04552366, NCT04566770, NCT04568811 RABV, EudraCT 2020-004066-19, LASV, YFV, NCT04449276,