The Current Status of Drug Repositioning and Vaccine Developments for the COVID-19 Pandemic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fact Sheet: COVID Vaccines & Fetal Cell Lines
Fact Sheet: COVID Vaccines & Fetal Cell Lines What is a fetal cell line? A cell taken from an aborted baby is multiplied into many cells of the same kind. These can be grown indefinitely and further multiplied, creating lines of cells that are sometimes used for science experiments. Fetus Kidney Tissue Human Cell Fetal Cell Line Expand and Multiply How are fetal cell lines used in vaccines? Fetal cell lines have been used to grow viruses and then create inactive viruses for vaccines. Historical fetal cell lines (WI-38 and MRC-5) derived in the 1960’s and 1970’s were used to create vaccines for diseases such as Rubella, Hepatitis A, and rabies. These and other historical cell lines (HEK293 and PER.C6) are sometimes used today in the creation of vaccines. Any vaccine that relies on these historic cell lines will not require new abortions. Are fetal cell lines necessary for vaccines? Most vaccines use non-human cells. Vaccines can be developed ethically using no cells or cells from animals, insects, chicken eggs, or yeast. Do COVID vaccines being developed in Operation Warp Speed use fetal cell lines? Six vaccines do not use fetal cell lines. Two vaccines do, using the historically derived fetal cell lines HEK293 and PER.C6. Table: Vaccines being developed in Operation Warp Speed Sponsor(s) Type of Vaccine Production Astrazeneca & Univ. Oxford Adenovirus carrier ❌ HEK293 abortion-derived cell line Janssen and Johnson & Adenovirus carrier ❌ PER.C6 abortion-derived cell line Johnson VSV (animal virus) Merck and IAVI ✅ Vero monkey cells carrier Novavax Protein vaccine ✅ Sf9 insect cells Sanofi and GSK Protein vaccine ✅ Sf9 insect cells Moderna with NIAID mRNA vaccine ✅ No cells used Pfizer and BioNTech mRNA vaccine ✅ No cells used Inovio Pharmaceuticals DNA vaccine ✅ No cells used In order to increase the rates of COVID vaccination among the public, many of whom are opposed to the use of fetal cell lines, policymakers may want to encourage the production and availability of vaccines that do not use fetal cell lines. -

Infectious Diseases
2013 MEDICINES IN DEVELOPMENT REPORT Infectious Diseases A Report on Diseases Caused by Bacteria, Viruses, Fungi and Parasites PRESENTED BY AMERICA’S BIOPHARMACEUTICAL RESEARCH COMPANIES Biopharmaceutical Research Evolves Against Infectious Diseases with Nearly 400 Medicines and Vaccines in Testing Throughout history, infectious diseases hepatitis C that inhibits the enzyme have taken a devastating toll on the lives essential for viral replication. and well-being of people around the • An anti-malarial drug that has shown Medicines in Development world. Caused when pathogens such activity against Plasmodium falci- For Infectious Diseases as bacteria or viruses enter a body and parum malaria which is resistant to multiply, infectious diseases were the current treatments. Application leading cause of death in the United Submitted States until the 1920s. Today, vaccines • A potential new antibiotic to treat methicillin-resistant Staphylococcus Phase III and infectious disease treatments have proven to be effective treatments in aureus (MRSA). Phase II many cases, but infectious diseases still • A novel treatment that works by Phase I pose a very serious threat to patients. blocking the ability of the smallpox Recently, some infectious pathogens, virus to spread to other cells, thus 226 such as pseudomonas bacteria, have preventing it from causing disease. become resistant to available treatments. Infectious diseases may never be fully Diseases once considered conquered, eradicated. However, new knowledge, such as tuberculosis, have reemerged new technologies, and the continuing as a growing health threat. commitment of America’s biopharma- America’s biopharmaceutical research ceutical research companies can help companies are developing 394 medicines meet the continuing—and ever-changing and vaccines to combat the many threats —threat from infectious diseases. -
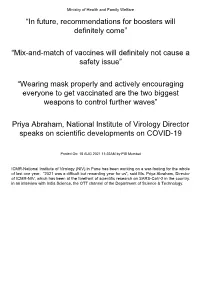
Mix-And-Match of Vaccines Will Definitely Not Cause a Safety Issue”
Ministry of Health and Family Welfare “In future, recommendations for boosters will definitely come” “Mix-and-match of vaccines will definitely not cause a safety issue” “Wearing mask properly and actively encouraging everyone to get vaccinated are the two biggest weapons to control further waves” Priya Abraham, National Institute of Virology Director speaks on scientific developments on COVID-19 Posted On: 18 AUG 2021 11:22AM by PIB Mumbai ICMR-National Institute of Virology (NIV) in Pune has been working on a war-footing for the whole of last one year. “2021 was a difficult but rewarding year for us”, said Ms. Priya Abraham, Director of ICMR-NIV, which has been at the forefront of scientific research on SARS-CoV-2 in the country. in an interview with India Science, the OTT channel of the Department of Science & Technology. Giving a quick overview of vaccine development process carried out at the institute which has been at the forefront of scientific research on SARS-CoV-2 in the country, she explained: “We quickly isolated and gave a strain to Bharat Biotech International Limited (BBIL) by the end of April (2020), after which they developed a whole virion-inactivated vaccine in the month of May and gave us back for review. We checked it for its complete inactivation, did its complete characterisation and started pre-clinical trials on hamsters and non-human primates, that is, monkeys. Those are very difficult experiments to do. These were conducted in our highest Bio-Safety Level-4 level containment facilities. In the next phase, we assisted them in the Phase I, II and III clinical trials in areas such as diagnostic aspect and laboratory support”. -

US and International Responses to the Global Spread of Avian
Order Code RL33219 CRS Report for Congress Received through the CRS Web U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Updated January 11, 2006 Tiaji Salaam-Blyther and Emma Chanlett-Avery Coordinators Foreign Affairs, Defense, and Trade Division Congressional Research Service ˜ The Library of Congress U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Summary One strain of avian influenza currently identified in Asia and Europe is known as Influenza A/H5N1. Although it is a bird flu, it has infected a relatively small number of people — killing around 50% of those infected. Scientists are concerned that H5N1 may cause the next influenza pandemic. Flu pandemics have occurred cyclically, roughly between every 30 and 50 years. Since 1997, when the first human contracted H5N1 in Hong Kong, the virus has resurfaced and spread to more than a dozen countries in Asia and Europe — infecting more than 140 people and killing approximately half. Britain and Taiwan both reported avian flu cases of H5N1 in 2005. In the latter cases, the infected birds were identified as imports, and died in quarantine. A global influenza pandemic could have a number of consequences. Global competition for existing vaccines and treatments could ensue. Some governments might restrict the export of vaccines or other supplies in order to treat their own population. Some countries might face a shortage of vaccines, antiviral medication, or other medical equipment, because of limited global supply. Hospitality and airline industries, and international trade could be negatively impacted. If global travel and trade were to suddenly drop, there could be productivity losses and service disruptions. -

The Solidarity Trial ‘Solidarity’ Is an International Clinical Trial to Help Find an Effective Treatment for COVID-19, Launched by the WHO and Partners
CORONAVIRUS (COVID-19) UPDATE NO. 22 / LAST UPDATED: 16 APRIL 2020 CURRENT SITUATION | COVID-19 RESPONSE | SCIENCE | FAITH COMMUNITY | RESOURCES CORONAVIRUS UPDATE 22 The Solidarity Trial ‘Solidarity’ is an international clinical trial to help find an effective treatment for COVID-19, launched by the WHO and partners. Find out which therapies are included in the trial. MORE Transmission Measures to reduce Guidance for the faith scenarios transmission community EPI WiN CORONAVIRUS (COVID-19) UPDATE NO. 22 / LAST UPDATED: 16 APRIL 2020 CURRENT SITUATION | COVID-19 RESPONSE | SCIENCE | FAITH COMMUNITY | RESOURCES Current global situation • Nearly 2 million confirmed cases • More than 123 000 deaths USA has more than 575 000 confirmed cases – • the most in the world Top ten countries with the highest number of new cases COUNTRY NEW REPORTED CASES IN LAST 24HRS United States of America 24 446 For the latest data, please access: France 5 483 è WHO situation dashboard United Kingdom 5 252 è WHO situation reports Turkey 4 062 è UNWFP world travel restrictions Russian Federation 3 388 Spain 3 045 Italy 2 972 Germany 2 486 Islamic Republic of Iran 1 574 Canada 1 360 Data as of 15.04.20 EPI WiN CORONAVIRUS (COVID-19) UPDATE NO. 22 / LAST UPDATED: 16 APRIL 2020 CURRENT SITUATION | COVID-19 RESPONSE | SCIENCE | FAITH COMMUNITY | RESOURCES Number of new cases of COVID-19 per day, by WHO Region 100 000 90 000 80 000 70 000 60 000 50 000 New daily cases New 40 000 30 000 20 000 10 000 0 * 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 March April AFRO AMRO EMRO EURO SEARO WPRO * There is no data from 22 March due to a change in the WHO situation reporting period EPI WiN CORONAVIRUS (COVID-19) UPDATE NO. -

Accelerated Development of COVID-19 Vaccines: Technology Platforms, Benefits, and Associated Risks
Perspective Accelerated Development of COVID-19 Vaccines: Technology Platforms, Benefits, and Associated Risks Ralf Wagner, Eberhard Hildt , Elena Grabski, Yuansheng Sun, Heidi Meyer, Annette Lommel, Brigitte Keller-Stanislawski, Jan Müller-Berghaus and Klaus Cichutek * Paul-Ehrlich-Institut, Federal Institute for Vaccines and Biomedicines, 63225 Langen, Germany; [email protected] (R.W.); [email protected] (E.H.); [email protected] (E.G.); [email protected] (Y.S.); [email protected] (H.M.); [email protected] (A.L.); [email protected] (B.K.-S.); [email protected] (J.M.-B.) * Correspondence: [email protected] Abstract: Multiple preventive COVID-19 vaccines have been developed during the ongoing SARS coronavirus (CoV) 2 pandemic, utilizing a variety of technology platforms, which have different properties, advantages, and disadvantages. The acceleration in vaccine development required to combat the current pandemic is not at the expense of the necessary regulatory requirements, including robust and comprehensive data collection along with clinical product safety and efficacy evaluation. Due to the previous development of vaccine candidates against the related highly pathogenic coronaviruses SARS-CoV and MERS-CoV, the antigen that elicits immune protection is known: the surface spike protein of SARS-CoV-2 or specific domains encoded in that protein, e.g., the receptor binding domain. From a scientific point of view and in accordance with legal Citation: Wagner, R.; Hildt, E.; frameworks and regulatory practices, for the approval of a clinic trial, the Paul-Ehrlich-Institut Grabski, E.; Sun, Y.; Meyer, H.; requires preclinical testing of vaccine candidates, including general pharmacology and toxicology as Lommel, A.; Keller-Stanislawski, B.; well as immunogenicity. -

WHO COVID-19 Database Search Strategy (Updated 26 May 2021)
Search purpose: Systematic search of the COVID-19 literature performed Monday through Friday for the WHO Database. Search strategy as of 26 May 2021. Searches performed by Tomas Allen, Kavita Kothari, and Martha Knuth. Use following commands to pull daily new entries: Entry_date:( [20210101 TO 20210120]) Entry_date:( 20210105) Duplicates: Duplicates are found in EndNote and Distillr using the Wichor method. Further screening is done by expert reviewers but some duplicates may still be in the database. Daily Search Strategy: Database Daily Search Strategy Medline (coronavir* OR corona virus* OR corona pandemic* OR betacoronavir* OR covid19 OR covid OR (Ovid) nCoV OR novel CoV OR CoV 2 OR CoV2 OR sarscov2 OR sars2 OR 2019nCoV OR wuhan virus* OR 1946- NCOV19 OR solidarity trial OR operation warp speed OR COVAX OR "ACT-Accelerator" OR BNT162b2 OR comirnaty OR "mRNA-1273" OR CoviShield OR AZD1222 OR Sputnik V OR CoronaVac OR "BBIBP-CorV" OR "Ad26.CoV2.S" OR "JNJ-78436735" OR Ad26COVS1 OR VAC31518 OR EpiVacCorona OR Convidicea OR "Ad5-nCoV" OR Covaxin OR CoviVac OR ZF2001 OR "NVX-CoV2373" OR "ZyCoV-D" OR CIGB 66 OR CVnCoV OR "INO-4800" OR "VIR-7831" OR "UB-612" OR BNT162 OR Soberana 1 OR Soberana 2 OR "B.1.1.7" OR "VOC 202012/01" OR "VOC202012/01" OR "VUI 202012/01" OR "VUI202012/01" OR "501Y.V1" OR UK Variant OR Kent Variant OR "VOC 202102/02" OR "VOC202102/02" OR "B.1.351" OR "VOC 202012/02" OR "VOC202012/02" OR "20H/501.V2" OR "20H/501Y.V2" OR "501Y.V2" OR "501.V2" OR South African Variant OR "B.1.1.28.1" OR "B.1.1.28" OR "B.1.1.248" OR -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -

An Examination of COVID-19 Medications' Effectiveness
healthcare Review An Examination of COVID-19 Medications’ Effectiveness in Managing and Treating COVID-19 Patients: A Comparative Review Mahmoud Al-Masaeed 1,* , Mohammad Alghawanmeh 2, Ashraf Al-Singlawi 3 , Rawan Alsababha 4 and Muhammad Alqudah 1 1 Faculty of Health and Medicine, University of Newcastle, Callaghan 2308, Australia; [email protected] 2 Faculty of Pharmacy, Philadelphia University, Amman 19392, Jordan; [email protected] 3 Independent Scholar, Amman 11731, Jordan; [email protected] 4 School of nursing and Midwifery, Western Sydney University, Sydney 2560, Australia; [email protected] * Correspondence: [email protected] Abstract: Background: The review seeks to shed light on the administered and recommended COVID- 19 treatment medications through an evaluation of their efficacy. Methods: Data were collected from key databases, including Scopus, Medline, Google Scholar, and CINAHL. Other platforms included WHO and FDA publications. The review’s literature search was guided by the WHO Citation: Al-Masaeed, M.; solidarity clinical trials for COVID-19 scope and trial-assessment parameters. Results: The findings Alghawanmeh, M.; Al-Singlawi, A.; indicate that the use of antiretroviral drugs as an early treatment for COVID-19 patients has been Alsababha, R.; Alqudah, M. An useful. It has reduced hospital time, hastened the clinical cure period, delayed and reduced the Examination of COVID-19 need for mechanical and invasive ventilation, and reduced mortality rates. The use of vitamins, Medications’ Effectiveness in minerals, and supplements has been linked to increased immunity and thus offering the body a Managing and Treating COVID-19 fighting chance. Nevertheless, antibiotics do not correlate with improving patients’ wellbeing and Patients: A Comparative Review. -

Solidarity” Clinical Trial for COVID-19
WHO’s “Solidarity” Clinical Trial for COVID-19 • Given the extreme pressure that COVID-19 is placing on health care systems worldwide, there is a pressing need to expeditiously identify therapies that can slow the progression of the disease in patients and/or increase the chances of survival. While randomized clinical trials normally take years to design and conduct, the world is currently in the midst of a fast-moving pandemic, and time is not on our side. • As a result, on March 20th, the World Health Organization (WHO) announced “Solidarity,” an international clinical trial that seeks to rapidly identify effective treatments for COVID-19. Currently, 1200 patients have already been randomized from five countries, with 600 hospitals ready to begin enrolling patients this week. • The trial seeks to compare the safety and efficacy of four different medications: Remdesivir, an experimental drug that has shown some promise in animal tests on two other coronaviruses—MERS and SARS; Lopinavir/Ritonavir, a drug combination used to treat HIV; Interferon beta-1a, used to treat multiple sclerosis; and chloroquine and hydroxychloroquine, drugs that are used to treat malaria and rheumatological conditions, respectively. As data becomes available, the list of drugs being tested could be modified, with the addition of new therapies or deletion of older ones. • The trial is designed to be as simple as possible so that it can be replicated even in hospitals that have been overwhelmed by an onslaught of cases. When a patient is deemed eligible to participate and consents, a physician will enter the patient’s data, including underlying conditions that could affect the course of treatment, into a WHO website which will then randomly assign a treatment option, consisting of either the local standard of care or the local of standard of care plus one of the above-mentioned treatments. -

Infodemic: How Has the Epidemic of Misinformation Affected the Response to COVID-19?
20 Infodemic: How Has the Epidemic of Misinformation Affected the Response to COVID-19? Series | COVID-19 & response strategy Authors: Carlos Chaccour (ISGlobal), Rafael Vilasanjuan (ISGlobal)* [ This is the twentieth Misinformation has played an impor- ment of the president of the United document in a series tant role during the COVID-19 pandem- States—as well as the inclusion of iver- of discussion notes ic. A general public desperate for reliable mectin in the national therapeutic guide- addressing fundamental data and a scientific publishing industry lines of Peru and Bolivia on the basis of questions about still characterised by many features of the in vitro experiments and fraudulent data2. COVID-19 and response Gutenberg era have contributed to a par- Other critical areas where false or mis- strategies. These allel pandemic: an infodemic. The term represented information has played a role documents are based infodemic refers to an overabundance of during this pandemic include the debate on the best scientific information—some accurate, some not— around the protection of children dur- information available on a particular subject. The World Health ing confinement, theuse of face masks and may be updated as Organisation (WHO) has long used this and the actual level and duration of im- new information comes term to describe an excess of information to light.] munity to the virus. This epidemic of about a topic, including many hoaxes or misinformation has been exacerbated by rumours, which make it difficult to find rushed scientific publication, the prioriti- reliable sources and guidance. sation of partisan activism over evidence, Most aspects of the COVID-19 debate and a general excess of opinions and de- have been burdened by this infodemic. -

Vaccines in Development to Target COVID-19 Disease April 9, 2020
Vaccines in Development to Target COVID-19 Disease April 9, 2020 BACKGROUND development, including funding research into the development and use of platform technologies and investigational vaccines Since its emergence in December 2019 in Wuhan, China, the against novel pathogens.6 Given the abundance of vaccines under SARS-CoV-2 virus has caused more than 1.3 million cases and development, this fact sheet will focus on the vaccine candidates nearly 75,000 deaths globally as of April 06, 2020.1 Currently, for which research is currently being funded at least in part by no vaccine or proven treatment exists for this virus or any CEPI, as well as candidates that are undergoing clinical trials. coronavirus. The rapid spread and unprecedented dramatic rise Vaccine candidates are listed by developer below. of COVID-19 deaths and cases has led many research groups worldwide to explore potential vaccine candidates against SARS-CoV-2.2 The World Health Organization (WHO) has Phase I Clinical Trials worked to develop a Research and Development Blueprint that outlines key areas for research and innovation to address gaps • CanSino Biological, Inc., and Beijing Institute of in controlling COVID-19.3 Additionally, as of April 4, 2020, Biotechnology WHO has identified more than 60 vaccine candidates currently CanSino Biological, Inc., a China-based company, is being investigated against the SARS-CoV-2 virus across a range collaborating with the Beijing Institute of Biotechnology to of platforms, including nucleic acid, live attenuated, protein develop a nonreplicating viral vector vaccine2 and has recently subunit, and viral vector (Table 1).2 Of these, 2 are undergoing begun phase I clinical trials, with more than 100 participants 7,8 phase 1 clinical trials, while the remaining candidates are aged 18 to 60 years old, in a hospital located in Wuhan, China.