Supplemental 1 (PDF)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perspectives for Therapeutic HPV Vaccine Development Andrew Yang1†, Emily Farmer1†,T.C.Wu1,2,3,4 and Chien-Fu Hung1,4,5*
Yang et al. Journal of Biomedical Science (2016) 23:75 DOI 10.1186/s12929-016-0293-9 REVIEW Open Access Perspectives for therapeutic HPV vaccine development Andrew Yang1†, Emily Farmer1†,T.C.Wu1,2,3,4 and Chien-Fu Hung1,4,5* Abstract Background: Human papillomavirus (HPV) infections and associated diseases remain a serious burden worldwide. It is now clear that HPV serves as the etiological factor and biologic carcinogen for HPV-associated lesions and cancers. Although preventative HPV vaccines are available, these vaccines do not induce strong therapeutic effects against established HPV infections and lesions. These concerns create a critical need for the development of therapeutic strategies, such as vaccines, to treat these existing infections and diseases. Main Body: Unlike preventative vaccines, therapeutic vaccines aim to generate cell-mediated immunity. HPV oncoproteins E6 and E7 are responsible for the malignant progression of HPV-associated diseases and are consistently expressed in HPV-associated diseases and cancer lesions; therefore, they serve as ideal targets for the development of therapeutic HPV vaccines. In this review we revisit therapeutic HPV vaccines that utilize this knowledge to treat HPV-associated lesions and cancers, with a focus on the findings of recent therapeutic HPV vaccine clinical trials. Conclusion: Great progress has been made to develop and improve novel therapeutic HPV vaccines to treat existing HPV infections and diseases; however, there is still much work to be done. We believe that therapeutic HPV vaccines have the potential to become a widely available and successful therapy to treat HPV and HPV-associated diseases in the near future. -

An Update Review of Globally Reported SARS-Cov-2 Vaccines in Preclinical and Clinical Stages
International Immunopharmacology 96 (2021) 107763 Contents lists available at ScienceDirect International Immunopharmacology journal homepage: www.elsevier.com/locate/intimp Review An update review of globally reported SARS-CoV-2 vaccines in preclinical and clinical stages Hamid Motamedi a, Marzie Mahdizade Ari b, Shirin Dashtbin b, Matin Fathollahi a, Hadi Hossainpour a, Amirhoushang Alvandi a,c, Jale Moradi a, Ramin Abiri a,d,* a Department of Microbiology, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran b Department of Microbiology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran c Medical Technology Research Center, Health Technology Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran d Fertility and Infertility Research Center, Health Technology Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran ARTICLE INFO ABSTRACT Keywords: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent of the rapidly spreading COVID-19 pandemic COVID-19 in the world. As an effective therapeutic strategy is not introduced yet and the rapid genetic SARS-CoV-2 variations in the virus, there is an emerging necessity to design, evaluate and apply effective new vaccines. An Vaccines acceptable vaccine must elicit both humoral and cellular immune responses, must have the least side effects and the storage and transport systems should be available and affordable for all countries. These vaccines can be classified into different types: inactivated vaccines, live-attenuated virus vaccines, subunit vaccines, virus-like particles (VLPs), nucleic acid-based vaccines (DNA and RNA) and recombinant vector-based vaccines (repli cating and non-replicating viral vector). According to the latest update of the WHO report on April 2nd, 2021, at least 85 vaccine candidates were being studied in clinical trial phases and 184 candidate vaccines were being evaluated in pre-clinical stages. -

Gamma-Irradiated SARS-Cov-2 Vaccine Candidate, OZG-38.61.3, Confers Protection from SARS-Cov-2 Challenge in Human ACEII-Transgen
www.nature.com/scientificreports OPEN Gamma‑irradiated SARS‑CoV‑2 vaccine candidate, OZG‑38.61.3, confers protection from SARS‑CoV‑2 challenge in human ACEII‑transgenic mice Raife Dilek Turan1,2,19, Cihan Tastan1,3,4,19*, Derya Dilek Kancagi1,19, Bulut Yurtsever1,19, Gozde Sir Karakus1,19, Samed Ozer5, Selen Abanuz1,6, Didem Cakirsoy1,8, Gamze Tumentemur7, Sevda Demir2, Utku Seyis1, Recai Kuzay1, Muhammer Elek1,2, Miyase Ezgi Kocaoglu1, Gurcan Ertop7, Serap Arbak9, Merve Acikel Elmas9, Cansu Hemsinlioglu1, Ozden Hatirnaz Ng10, Sezer Akyoney10,11, Ilayda Sahin8,12, Cavit Kerem Kayhan13, Fatma Tokat14, Gurler Akpinar15, Murat Kasap15, Ayse Sesin Kocagoz16, Ugur Ozbek12, Dilek Telci2, Fikrettin Sahin2, Koray Yalcin1,17, Siret Ratip18, Umit Ince14 & Ercument Ovali1 The SARS‑CoV‑2 virus caused the most severe pandemic around the world, and vaccine development for urgent use became a crucial issue. Inactivated virus formulated vaccines such as Hepatitis A and smallpox proved to be reliable approaches for immunization for prolonged periods. In this study, a gamma‑irradiated inactivated virus vaccine does not require an extra purifcation process, unlike the chemically inactivated vaccines. Hence, the novelty of our vaccine candidate (OZG‑38.61.3) is that it is a non‑adjuvant added, gamma‑irradiated, and intradermally applied inactive viral vaccine. Efciency and safety dose (either 1013 or 1014 viral RNA copy per dose) of OZG‑38.61.3 was initially determined in BALB/c mice. This was followed by testing the immunogenicity and protective efcacy of the vaccine. Human ACE2‑encoding transgenic mice were immunized and then infected with the SARS‑CoV‑2 virus for the challenge test. -

Main Outcomes of Discussion of WHO Consultation on Nucleic Acid
MAIN OUTCOMES OF DISCUSSION FROM WHO CONSULTATION ON NUCLEIC ACID VACCINES I. Knezevic, R. Sheets 21-23 Feb, 2018 Geneva, Switzerland CONTEXT OF DISCUSSION • WHO Consultation held to determine whether the existing DNA guidelines were due for revision or if they remained relevant with today’s status of nucleic acid vaccine development and maturity towards licensure (marketing authorization) • Presentation will cover alignment to existing guidelines • Current status of development of DNA and RNA vaccines, both prophylactic & therapeutic • Main outcomes of discussion • Next steps already underway & planned STATUS OF DEVELOPMENT OF NUCLEIC ACID VACCINES • First likely candidate to licensure could be a therapeutic DNA vaccine against Human Papilloma Viruses • Anticipated to be submitted for licensure in 3-5 years • Other DNA vaccines are likely to follow shortly thereafter, e.g., Zika prophylaxis • RNA vaccines – less clinical experience, but therapeutic RNAs anticipated in 2021/22 timeframe to be submitted for licensure • For priority pathogens in context of public health emergencies, several candidates under development (e.g., MERS-CoV, Marburg, Ebola) MAIN OUTCOMES - GENERAL • Regulators expressed need for updated DNA guideline for prophylaxis and therapy • Less need at present for RNA vaccines in guideline but need some basic PTC • Flexibility needed now until more experience gained for RNA vaccines that will come in next few years • Revisit need for a more specific guideline at appropriate time for RNA vaccines • Institutional Biosafety Committees are regulated by national jurisdictions & vary considerably • How can WHO assist to streamline or converge these review processes? Particularly, during Public Health Emergency – can anything be done beforehand? MAIN OUTCOMES - DEFINITIONS • Clear Definitions are needed • Proposed definition of DNA vaccine: • A DNA plasmid(s) into which the desired immunogen(s) is (are) encoded and prepared as purified plasmid preparations to be administered in vivo. -
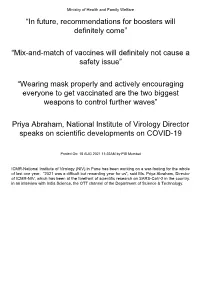
Mix-And-Match of Vaccines Will Definitely Not Cause a Safety Issue”
Ministry of Health and Family Welfare “In future, recommendations for boosters will definitely come” “Mix-and-match of vaccines will definitely not cause a safety issue” “Wearing mask properly and actively encouraging everyone to get vaccinated are the two biggest weapons to control further waves” Priya Abraham, National Institute of Virology Director speaks on scientific developments on COVID-19 Posted On: 18 AUG 2021 11:22AM by PIB Mumbai ICMR-National Institute of Virology (NIV) in Pune has been working on a war-footing for the whole of last one year. “2021 was a difficult but rewarding year for us”, said Ms. Priya Abraham, Director of ICMR-NIV, which has been at the forefront of scientific research on SARS-CoV-2 in the country. in an interview with India Science, the OTT channel of the Department of Science & Technology. Giving a quick overview of vaccine development process carried out at the institute which has been at the forefront of scientific research on SARS-CoV-2 in the country, she explained: “We quickly isolated and gave a strain to Bharat Biotech International Limited (BBIL) by the end of April (2020), after which they developed a whole virion-inactivated vaccine in the month of May and gave us back for review. We checked it for its complete inactivation, did its complete characterisation and started pre-clinical trials on hamsters and non-human primates, that is, monkeys. Those are very difficult experiments to do. These were conducted in our highest Bio-Safety Level-4 level containment facilities. In the next phase, we assisted them in the Phase I, II and III clinical trials in areas such as diagnostic aspect and laboratory support”. -

US and International Responses to the Global Spread of Avian
Order Code RL33219 CRS Report for Congress Received through the CRS Web U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Updated January 11, 2006 Tiaji Salaam-Blyther and Emma Chanlett-Avery Coordinators Foreign Affairs, Defense, and Trade Division Congressional Research Service ˜ The Library of Congress U.S. and International Responses to the Global Spread of Avian Flu: Issues for Congress Summary One strain of avian influenza currently identified in Asia and Europe is known as Influenza A/H5N1. Although it is a bird flu, it has infected a relatively small number of people — killing around 50% of those infected. Scientists are concerned that H5N1 may cause the next influenza pandemic. Flu pandemics have occurred cyclically, roughly between every 30 and 50 years. Since 1997, when the first human contracted H5N1 in Hong Kong, the virus has resurfaced and spread to more than a dozen countries in Asia and Europe — infecting more than 140 people and killing approximately half. Britain and Taiwan both reported avian flu cases of H5N1 in 2005. In the latter cases, the infected birds were identified as imports, and died in quarantine. A global influenza pandemic could have a number of consequences. Global competition for existing vaccines and treatments could ensue. Some governments might restrict the export of vaccines or other supplies in order to treat their own population. Some countries might face a shortage of vaccines, antiviral medication, or other medical equipment, because of limited global supply. Hospitality and airline industries, and international trade could be negatively impacted. If global travel and trade were to suddenly drop, there could be productivity losses and service disruptions. -

(ACIP) General Best Guidance for Immunization
8. Altered Immunocompetence Updates This section incorporates general content from the Infectious Diseases Society of America policy statement, 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host (1), to which CDC provided input in November 2011. The evidence supporting this guidance is based on expert opinion and arrived at by consensus. General Principles Altered immunocompetence, a term often used synonymously with immunosuppression, immunodeficiency, and immunocompromise, can be classified as primary or secondary. Primary immunodeficiencies generally are inherited and include conditions defined by an inherent absence or quantitative deficiency of cellular, humoral, or both components that provide immunity. Examples include congenital immunodeficiency diseases such as X- linked agammaglobulinemia, SCID, and chronic granulomatous disease. Secondary immunodeficiency is acquired and is defined by loss or qualitative deficiency in cellular or humoral immune components that occurs as a result of a disease process or its therapy. Examples of secondary immunodeficiency include HIV infection, hematopoietic malignancies, treatment with radiation, and treatment with immunosuppressive drugs. The degree to which immunosuppressive drugs cause clinically significant immunodeficiency generally is dose related and varies by drug. Primary and secondary immunodeficiencies might include a combination of deficits in both cellular and humoral immunity. Certain conditions like asplenia and chronic renal disease also can cause altered immunocompetence. Determination of altered immunocompetence is important to the vaccine provider because incidence or severity of some vaccine-preventable diseases is higher in persons with altered immunocompetence; therefore, certain vaccines (e.g., inactivated influenza vaccine, pneumococcal vaccines) are recommended specifically for persons with these diseases (2,3). Administration of live vaccines might need to be deferred until immune function has improved. -

Updated May 26, 2021 Cross-Border Industry Partnerships on COVID-19 Vaccines and Therapeutics Vaccines • Curevac O Celonic Wi
Updated May 26, 2021 Cross-Border Industry Partnerships on COVID-19 Vaccines and Therapeutics Vaccines • CureVac o Celonic will manufacture 100 million doses of CureVac’s vaccine at its plant in Heidelberg, Germany, providing bulk substance for 50 million doses by the end of 2021. (press release) o Novartis will manufacture CureVac’s vaccine. (press release) o GlaxoSmithKline plc and CureVac N.V. announced a new €150m collaboration, building on their existing relationship, to jointly develop next generation mRNA vaccines for COVID-19 with the potential for a multi-valent approach to address multiple emerging variants in one vaccine. (press release) o Rentschler Biopharma SE will manufacture CureVac’s vaccine. (press release) o Bayer will support the further development, supply and key territory operations of CureVac’s vaccine candidate. (press release) o Fareva will dedicate a manufacturing plant in France to the fill and finish of CureVac’s vaccine. (press release) o Wacker Chemie AG will manufacture CureVac’s vaccine candidate at its Amsterdam site. (press release) o CureVac will collaborate with Tesla Grohmann Automation to develop an RNA printer that works like a mini-factory and can produce such drugs automatically. (press release) • Moderna o Samsung Biologics will provide large scale, commercial fill-finish manufacturing for Moderna’s vaccine in South Korea. (press release) o Baxter International will provide fill/finish services and supply packaging for Moderna. (press release) o Sanofi will manufacture 200 million doses of Moderna’s COVID-19 vaccine starting in September 2021. (press release) o Rovi will produce bulk substance for Moderna’s COVID-19 vaccine, expanding an agreement between the companies. -

COVID-19 Situation Report 210
For citation: Centre for Infectious Disease Epidemiology and Research-NUS. COVID-19 Situation Report 210. 27 August 2020 Aug 27 COVID-19 Situation Report 210 Centre for Infectious Disease Epidemiology and Research (CIDER) For citation: Centre for Infectious Disease Epidemiology and Research-NUS. COVID-19 Situation Report 210. 27 August 2020 i. Background In December, China notified the World Health Organization (WHO) of several cases of human respiratory illness, which appeared to be linked to an open seafood and livestock market in the city of Wuhan. The infecting agent has since been identified as a novel coronavirus, previously known as 2019-nCoV and now called SAR-CoV-2; The new name of the disease has also been termed COVID-19, as of 11th February 2020. Although the virus is presumed zoonotic in origin, person-to-person spread is evident. Screening of travellers, travel bans and quarantine measures are being implemented in many countries. Despite these precautions, it is anticipated that more cases will be seen both inside China and internationally. The WHO declared the outbreak of COVID-19 constitutes a Public Health Emergency of International Concern on 30 January. On 11 March, 2020, WHO declared the coronavirus outbreak a pandemic as the global death toll rose above 4,600 and the number of confirmed cases topped 125,000. This report aims to update Global Risk Assessment, Global Epidemiology, Quarantine Orders, Travel Ban/Advisory by countries, WHO’s and CDC’s Guidance and Protocols and Scientific publication on a daily basis. New updates in the tables are bolded. 1 | P a g e Centre for infectious di sease epidemiology and research For citation: Centre for Infectious Disease Epidemiology and Research-NUS. -

COVID-19 Vaccination Strategy in China: a Case Study
Article COVID-19 Vaccination Strategy in China: A Case Study Marjan Mohamadi 1,†, Yuling Lin 1,*,† ,Mélissa Vuillet Soit Vulliet 1,†, Antoine Flahault 1, Liudmila Rozanova 1 and Guilhem Fabre 2 1 Institute of Global Health, University of Geneva, 1211 Geneva, Switzerland; [email protected] (M.M.); [email protected] (M.V.S.V.); antoine.fl[email protected] (A.F.); [email protected] (L.R.) 2 Department of Chinese, UFR 2, Université Paul Valéry Montpellier 3, 34199 Montpellier, France; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The coronavirus disease 2019 (COVID-19) outbreak in China was first reported to the World Health Organization on 31 December 2019, after the first cases were officially identified around 8 December 2019. However, the case of an infected patient of 55 years old can probably be traced back on 17 November. The spreading has been rapid and heterogeneous. Economic, political and social impacts have not been long overdue. This paper, based on English, French and Chinese research in national and international databases, aims to study the COVID-19 situation in China through the management of the outbreak and the Chinese response to vaccination strategy. The coronavirus disease pandemic is under control in China through non-pharmaceutical interventions, and the mass vaccination program has been launched to further prevent the disease and progressed steadily with Citation: Mohamadi, M.; Lin, Y.; 483.34 million doses having been administered across the country by 21 May 2021. China is also Vulliet, M.V.S.; Flahault, A.; acting as an important player in the development and production of SARS-CoV-2 vaccines. -

Vaccins Contre La Covid-19 Et Utilisation De Cellules D'origine Fœtale
Vaccins contre la Covid-19 et utilisation de cellules d’origine fœtale : un questionnement éthique pour les chrétiens. Dr Michel Cambrelin La pandémie Covid-19 due au nouveau Coronavirus SARS-CoV-2 n’épargne pas nos sociétés occidentales, qui sont fortement ébranlées malgré leur richesse et leur technologie, et notre pays ne fait pas exception1. Après les échecs successifs des tentatives de contenir cette épidémie, la vaccination nous est présentée comme la planche de salut. Cette vaccination a pour principe de présenter à l’organisme receveur des éléments inoffensifs appartenant au virus, ce qui va lui permettre de fabriquer des anticorps prêts à le défendre lorsque le virus essaiera de le pénétrer. Pour ces vaccins différentes techniques ont été utilisées, qui pour certaines sont assez nouvelles, que nous expliquerons plus loin. De multiples questions et rumeurs circulent sur les vaccins Covid en particulier à ARN messager (ARNm), auxquelles l’OMS2 et la Société de Pathologie Infectieuse de Langue Française3 ont apporté leurs réponses. Bien que les Français y semblaient réticents au départ, une politique de vaccination croissante se met en place, dont on critique maintenant la lenteur du démarrage. Cependant une autre question interpelle les chrétiens, respectueux de la vie humaine constituant un don de Dieu dès la conception4, question qui n’est pas abordée dans les médias ni dans les recommandations scientifiques : certains vaccins contre la Covid auraient été élaborés à l’aide de cellules de fœtus avortés ! Nous allons tenter d’apporter les éléments de réponse nécessaires à cette question, qui semble ignorée du débat public, sans aborder les autres questions d’innocuité et d’efficacité de ces vaccins qui ont aussi leur importance éthique. -

Considerations for Causality Assessment of Neurological And
Occasional essay J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2021-326924 on 6 August 2021. Downloaded from Considerations for causality assessment of neurological and neuropsychiatric complications of SARS- CoV-2 vaccines: from cerebral venous sinus thrombosis to functional neurological disorder Matt Butler ,1 Arina Tamborska,2,3 Greta K Wood,2,3 Mark Ellul,4 Rhys H Thomas,5,6 Ian Galea ,7 Sarah Pett,8 Bhagteshwar Singh,3 Tom Solomon,4 Thomas Arthur Pollak,9 Benedict D Michael,2,3 Timothy R Nicholson10 For numbered affiliations see INTRODUCTION More severe potential adverse effects in the open- end of article. The scientific community rapidly responded to label phase of vaccine roll- outs are being collected the COVID-19 pandemic by developing novel through national surveillance systems. In the USA, Correspondence to SARS- CoV-2 vaccines (table 1). As of early June Dr Timothy R Nicholson, King’s roughly 372 adverse events have been reported per College London, London WC2R 2021, an estimated 2 billion doses have been million doses, which is a lower rate than expected 1 2LS, UK; timothy. nicholson@ administered worldwide. Neurological adverse based on the clinical trials.6 kcl. ac. uk events following immunisation (AEFI), such as In the UK, adverse events are reported via the cerebral venous sinus thrombosis and demyelin- MB and AT are joint first Coronavirus Yellow Card reporting website. As of ating episodes, have been reported. In some coun- authors. early June 2021, approximately 250 000 Yellow tries, these have led to the temporary halting of BDM and TRN are joint senior Cards have been submitted, equating to around authors.