Main Outcomes of Discussion of WHO Consultation on Nucleic Acid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perspectives for Therapeutic HPV Vaccine Development Andrew Yang1†, Emily Farmer1†,T.C.Wu1,2,3,4 and Chien-Fu Hung1,4,5*
Yang et al. Journal of Biomedical Science (2016) 23:75 DOI 10.1186/s12929-016-0293-9 REVIEW Open Access Perspectives for therapeutic HPV vaccine development Andrew Yang1†, Emily Farmer1†,T.C.Wu1,2,3,4 and Chien-Fu Hung1,4,5* Abstract Background: Human papillomavirus (HPV) infections and associated diseases remain a serious burden worldwide. It is now clear that HPV serves as the etiological factor and biologic carcinogen for HPV-associated lesions and cancers. Although preventative HPV vaccines are available, these vaccines do not induce strong therapeutic effects against established HPV infections and lesions. These concerns create a critical need for the development of therapeutic strategies, such as vaccines, to treat these existing infections and diseases. Main Body: Unlike preventative vaccines, therapeutic vaccines aim to generate cell-mediated immunity. HPV oncoproteins E6 and E7 are responsible for the malignant progression of HPV-associated diseases and are consistently expressed in HPV-associated diseases and cancer lesions; therefore, they serve as ideal targets for the development of therapeutic HPV vaccines. In this review we revisit therapeutic HPV vaccines that utilize this knowledge to treat HPV-associated lesions and cancers, with a focus on the findings of recent therapeutic HPV vaccine clinical trials. Conclusion: Great progress has been made to develop and improve novel therapeutic HPV vaccines to treat existing HPV infections and diseases; however, there is still much work to be done. We believe that therapeutic HPV vaccines have the potential to become a widely available and successful therapy to treat HPV and HPV-associated diseases in the near future. -

Review of COVID-19 Vaccine Subtypes, Efficacy and Geographical Distributions Andre Ian Francis ,1 Saudah Ghany,1 Tia Gilkes,1 Srikanth Umakanthan2
Review Postgrad Med J: first published as 10.1136/postgradmedj-2021-140654 on 6 August 2021. Downloaded from Review of COVID-19 vaccine subtypes, efficacy and geographical distributions Andre Ian Francis ,1 Saudah Ghany,1 Tia Gilkes,1 Srikanth Umakanthan2 1Department of Clinical Medical ABSTRACT 2021, the Ad26.COV2.S, developed by Janssen Sciences, The Faculty of Medical As of 1 May 2021, there have been 152 661 445 (Johnson & Johnson) and Moderna on 30 April.4 Sciences, The University of the COVAX, coordinated by WHO, Gavi: The West Indies, St. Augustine, Covid-19 cases with 3 202 256 deaths globally. Trinidad and Tobago This pandemic led to the race to discover a vaccine Vaccine Alliance, the Coalition for Epidemic 2Pathology unit, Department to achieve herd immunity and curtail the damaging Preparedness Innovations (CEPI), acts as a of Paraclinical Sciences, The effects of Covid-19. This study aims to discuss the most programme that supports the development of University Of The West Indies, St. COVID-19 vaccine candidates and negotiates their Augustine, Trinidad and Tobago recent WHO-approved Covid-19 vaccine subtypes, their status and geographical scheduled updates as of 4 pricing to ensure low- and- middle- income countries have a fair shot at receiving vaccines.5 Correspondence to May 2021. The keywords “Covid-19, Vaccines, Pfizer, Mr. Andre Ian Francis, The BNT162b2, AstraZeneca, AZD1222, Moderna, mRNA- This article aims at discussing the most recent University of the West Indies, St. 1273, Janssen, Ad26.COV2.S” were typed into PubMed. WHO- approved COVID-19 vaccine subtypes, their Augustine, Trinidad and Tobago; Thirty Two relevant PubMed articles were included in status and geographical scheduled updates as of 4 andre. -

V.5 3/18/2021 1 COVID-19 Vaccine FAQ Sheet
COVID-19 Vaccine FAQ Sheet (updated 3/18/2021) The AST has received queries from transplant professionals and the community regarding the COVID-19 vaccine. The following FAQ was developed to relay information on the current state of knowledge. This document is subject to change and will be updated frequently as new information or data becomes available. What kinds of vaccines are available or under development to prevent COVID-19? There are currently several vaccine candidates in use or under development. In the United States, the Government is supporting six separate vaccine candidates. Several other vaccines are also undergoing development outside of the United States government sponsorship and further information can be found here: NYTimes Coronavirus Vaccine Tracker: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine- tracker.html Washington Post Vaccine Tracker: https://www.washingtonpost.com/graphics/2020/health/covid-vaccine-update- coronavirus/ v.5 3/18/2021 1 The types of vaccines are as follows (March 1, 2021) 1: Table 1: Vaccines Under Development or Available Through EUA Vaccine Type Compound Name [Sponsor] Clinical Notes Trial Phase mRNA mRNA-1273 [Moderna] Phase 3 Emergency use in U.S., E.U., other countries Approved in Canada BNT162b2 (Comirnaty) [Pfizer] Phase 2/3 Emergency use in U.S., E.U., other countries Also approved in Canada and other countries Replication- AZD1222 (Covishield) Phase 2/3 Emergency use defective [AstraZeneca] in U.K., India, adenoviral other countries vector (not U.S.) JNJ-78326735/Ad26.COV2.S -

An Update on Self-Amplifying Mrna Vaccine Development
Review An Update on Self-Amplifying mRNA Vaccine Development Anna K. Blakney 1,* , Shell Ip 2 and Andrew J. Geall 2 1 Michael Smith Laboratories, School of Biomedical Engineering, University of British Columbia, Vancouver, BC V6T 1Z4, Canada 2 Precision NanoSystems Inc., Vancouver, BC V6P 6T7, Canada; [email protected] (S.I.); [email protected] (A.J.G.) * Correspondence: [email protected] Abstract: This review will explore the four major pillars required for design and development of an saRNA vaccine: Antigen design, vector design, non-viral delivery systems, and manufacturing (both saRNA and lipid nanoparticles (LNP)). We report on the major innovations, preclinical and clinical data reported in the last five years and will discuss future prospects. Keywords: RNA; self-amplifying RNA; replicon; vaccine; drug delivery 1. Introduction: The Four Pillars of saRNA Vaccines In December 2019, the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus emerged, causing a respiratory illness, coronavirus disease 2019 (COVID-19), in Hubei province, China [1,2]. The virus has spread globally, with the World Health Organization (WHO) declaring it a Public Health Emergency of International concern on 30 January 2020 and a pandemic officially on 7 March 2020 [3]. There is a strong consensus globally that a COVID-19 vaccine is likely the most effective approach to sustainably controlling the COVID-19 pandemic [4]. There has been an unprecedented research effort and global Citation: Blakney, A.K.; Ip, S.; Geall, coordination which has resulted in the rapid development of vaccine candidates and A.J. An Update on Self-Amplifying initiation of human clinical trials. -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -

Plant-Made HIV Vaccines and Potential Candidates
Plant-made HIV vaccines and potential candidates Jocelyne Tremouillaux-Guiller1, Khaled Moustafa2, Kathleen Hefferon3, Goabaone Gaobotse4, and Abdullah Makhzoum4 1Faculty of Pharmaceutical Sciences, University François Rabelais, Tours, France. 2Arabic Science Archive – ArabiXiv (https://arabixiv.org). 3Department of Microbiology, Cornell University, USA. 4Department of Biological Sciences & Biotechnology, Botswana International University of Science & Technology, Botswana. Correspondence: [email protected]; [email protected] Highlights HIV/AIDS is a partially treatable but not completely curable pandemic disease. Major advances have been made to treat patients living with HIV/AIDS. Developing HIV vaccines is an ongoing endeavor and moves at an accelerated pace Plant molecular pharming is a valuable tool in HIV/AIDS vaccine research. Abstract Millions of people around the world suffer from heavy social and health burdens related to HIV/AIDS and its associated opportunistic infections. To reduce these burdens, preventive and therapeutic vaccines are required. Effective HIV vaccines have been under investigation for several decades using different animal models. Potential plant-made HIV vaccine candidates have also gained attention in the past few years. In addition to this, broadly neutralizing antibodies produced in plants which can target conserved viral epitopes and neutralize mutating HIV strains have been identified. Numerous epitopes of glycoproteins and capsid proteins of HIV-1 are a part of HIV therapy. Here, we discuss some recent findings aiming to produce anti-HIV-1 recombinant proteins in engineered plants for AIDS prophylactics and therapeutic treatments. Keywords: plant made pharmaceuticals; HIV vaccine; AIDS drug; plant molecular pharming/farming; multiepitopic HIV vaccine. 1 Introduction Acquired Immunodeficiency Syndrome (AIDS) is one of the greatest challenges to global public health today. -

Revision Rápida
REVISION RÁPIDA EVALUACIÓN DE LAS CARACTERÍSTICAS DE ALMACENAMIENTO, TRANSPORTE Y DISTRIBUCIÓN DE LAS VACUNAS COVID-19 EN ESTUDIO, Y LAS CARACTERÍSTICAS CLÍNICAS DE LA POBLACIÓN CANDIDATA A VACUNACIÓN Noviembre de 2020 El Instituto de Evaluación Tecnológica en Salud – IETS, es una corporación sin ánimo de lucro, de participación mixta y de carácter privado, con patrimonio propio, creado según lo estipulado en la Ley 1438 de 2011. Su misión es contribuir al desarrollo de mejores políticas públicas y prácticas asistenciales en salud, mediante la producción de información basada en evidencia, a través de la evaluación de tecnologías en salud y guías de práctica clínica, con rigor técnico, independencia y participación. Sus miembros son el Ministerio de Salud y Protección Social – MinSalud, el Departamento Administrativo de Ciencia, Tecnología e Innovación – Colciencias, el Instituto Nacional de Vigilancia de Medicamentos y Alimentos – INVIMA, el Instituto Nacional de Salud – INS, la Asociación Colombiana de Facultades de Medicina – ASCOFAME y la Asociación Colombiana de Sociedades Científicas – ACSC. Autores Lucas López Quiceno. Médico y cirujano, Especialista en Epidemiología, Magister en Epidemiología, Magíster en economía de la salud (c). Instituto de Evaluación Tecnológica en Salud - IETS. Jhyld Carolaind Camacho Barbosa, Nutricionista y Dietista, Magister en Epidemiología. Instituto de Evaluación Tecnológica en Salud - IETS. Kelly Estrada-Orozco. Médica, Magister en Epidemiología Clínica, Magister en Neurociencia. Doctorado en Salud Pública (actual). Doctorado en Epidemiología Clínica (actual). Instituto de Evaluación Tecnológica en Salud - IETS. Revisores Cortes-Muñoz, Ani Julieth. Bacterióloga y laboratorista clínica. MSc. Epidemiología. Instituto de Evaluación Tecnológica en salud - IETS. Ospina-Lizarazo, Nathalie. Nutricionista Dietista. MSc. Epidemiología Clínica. Instituto de Evaluación Tecnológica en salud - IETS. -

Covid-19 Messenger Rna Vaccine
COVID-19 MESSENGER RNA VACCINE A Piece of the Coronavirus The SARS-CoV-2 virus is studded with proteins that it uses to enter human cells. These so-called spike proteins make a tempting target for potential vaccines and treatments. Image of Coronavirus and spike proteins. Spike CORONAVIRUS protein Spikes gene Like the Pfizer vaccine, Moderna’s vaccine is based on the virus’s genetic instructions for building the spike protein. mRNA Inside an Oily Shell The vaccine uses messenger RNA, genetic material that our cells read to make proteins. The molecule — called mRNA for short — is fragile and would be chopped to pieces by our natural enzymes if it were injected directly into the body. To protect their vaccine, Pfizer and BioNTech wrap mRNA in oily bubbles made of lipid nanoparticles. Lipid nanoparticles surrounding mRNA Entering a Cell After injection, the vaccine particles bump into cells and fuse to them, releasing mRNA. The cell’s molecules read its sequence and build spike proteins. The mRNA from the vaccine is eventually destroyed by the cell, leaving no permanent trace. Vaccine Particle Translating mRNA fuses into Spike Spike Protien, which beaks it into Protein fragmentsmRNA and then destroyed by the Translatingcell nucleus. mRNA Spike Three spike Proteins Combine Cell Nucleus Spike Proteins and Fragments Protruding Displaying Protein Fragments Spikes Some of the spike proteins form spikes that migrate to the surface of the cell and stick out their tips. The vaccinated cells also break up some of the proteins into fragments, which they present on their surface. These protruding spikes and spike protein fragments can then be recognized by the immune system. -

Soluble Spike DNA Vaccine Provides Long-Term Protective Immunity Against SARS-Cov-2 in Mice and Nonhuman Primates
Article Soluble Spike DNA Vaccine Provides Long-Term Protective Immunity against SARS-CoV-2 in Mice and Nonhuman Primates Yong Bok Seo 1, You Suk Suh 2, Ji In Ryu 1, Hwanhee Jang 1, Hanseul Oh 3, Bon-Sang Koo 3, Sang-Hwan Seo 4, Jung Joo Hong 3, Manki Song 4, Sung-Joo Kim 5 and Young Chul Sung 1,2,* 1 Research Institute, SL VaxiGen Inc., Korea Bio Park, Seongnam 13488, Korea; [email protected] (Y.B.S.); [email protected] (J.I.R.); [email protected] (H.J.) 2 Research Institute, Genexine Inc., Korea Bio Park, Seongnam 13488, Korea; [email protected] 3 National Primate Research Centre, Korea Research Institute of Bioscience and Biotechnology, Cheongju, Chungcheongbuk 34141, Korea; [email protected] (H.O.); [email protected] (B.-S.K.); [email protected] (J.J.H.) 4 Science Unit, International Vaccine Institute, Seoul 08826, Korea; [email protected] (S.-H.S.); [email protected] (M.S.) 5 GenNBio Inc., Seoul 06026, Korea; [email protected] * Correspondence: [email protected] Abstract: The unprecedented and rapid spread of SARS-CoV-2 (severe acute respiratory syndrome- coronavirus-2) has motivated the need for a rapidly producible and scalable vaccine. Here, we Citation: Seo, Y.B.; Suh, Y.S.; Ryu, J.I.; developed a synthetic soluble SARS-CoV-2 spike (S) DNA-based vaccine candidate, GX-19. In mice, Jang, H.; Oh, H.; Koo, B.-S.; Seo, S.-H.; immunization with GX-19 elicited not only S-specific systemic and pulmonary antibody responses Hong, J.J.; Song, M.; Kim, S.-J.; et al. -
Candidate SARS-Cov-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D
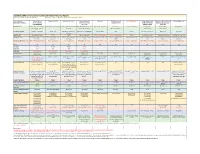
Candidate SARS-CoV-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D. Grabenstein, RPh, PhD All dates are estimates. All Days are based on first vaccination at Day 0. Vaccine Sponsor Univ. of Oxford ModernaTX USA BioNTech with Pfizer Johnson & Johnson Novavax Sanofi Pasteur with CureVac with Bayer CanSino Biologics with Sinopharm (China National Sinovac Biotech Co. [with Major Partners] (Jenner Institute) (Janssen Vaccines & GlaxoSmithKline Academy of Military Biotec Group) (Beijing IBP, with AstraZeneca Prevention) Medical Sciences Wuhan IBP) Headquarters Oxford, England; Cambridge, Cambridge, Massachusetts Mainz, Germany; New York, New Brunswick, New Jersey Gaithersburg, Maryland Lyon, France; Tübingen, Germany Tianjin, China; Beijing, China; Beijing, China England, Gothenburg, New York (Leiden, Netherlands) Brentford, England Beijing, China Wuhan, China Sweden Product Designator ChAdOx1 or AZD1222 mRNA-1273 BNT162b2, tozinameran, Ad26.COV2.S, JNJ-78436735 NVX-CoV2373 TBA CVnCoV Ad5-nCoV, Convidecia BBIBP-CorV CoronaVac Comirnaty Vaccine Type Adenovirus 63 vector mRNA mRNA Adenovirus 26 vector Subunit (spike) protein Subunit (spike) protein mRNA Adenovirus 5 vector Inactivated whole virus Inactivated whole virus Product Features Chimpanzee adenovirus type Within lipid nanoparticle Within lipid nanoparticle Human adenovirus type 26 Adjuvanted with Matrix-M Adjuvanted with AS03 or Adjuvanted with AS03 Human adenovirus type 5 Adjuvanted with aluminum Adjuvanted with aluminum 63 vector dispersion dispersion vector AF03 -

DNA-Launched RNA Replicon Vaccines Induce Potent Anti-SARS-Cov-2
www.nature.com/scientificreports OPEN DNA‑launched RNA replicon vaccines induce potent anti‑SARS‑CoV‑2 immune responses in mice Inga Szurgot*, Leo Hanke, Daniel J. Sheward, Laura Perez Vidakovics, Ben Murrell, Gerald M. McInerney & Peter Liljeström The outbreak of the SARS‑CoV‑2 virus and its rapid spread into a global pandemic made the urgent development of scalable vaccines to prevent coronavirus disease (COVID‑19) a global health and economic imperative. Here, we characterized and compared the immunogenicity of two alphavirus‑ based DNA‑launched self‑replicating (DREP) vaccine candidates encoding either SARS‑CoV‑2 spike glycoprotein (DREP‑S) or a spike ectodomain trimer stabilized in prefusion conformation (DREP‑Secto). We observed that the two DREP constructs were immunogenic in mice inducing both binding and neutralizing antibodies as well as T cell responses. Interestingly, the DREP coding for the unmodifed spike turned out to be more potent vaccine candidate, eliciting high titers of SARS‑CoV‑2 specifc IgG antibodies that were able to efciently neutralize pseudotyped virus after a single immunization. In addition, both DREP constructs were able to efciently prime responses that could be boosted with a heterologous spike protein immunization. These data provide important novel insights into SARS‑ CoV‑2 vaccine design using a rapid response DNA vaccine platform. Moreover, they encourage the use of mixed vaccine modalities as a strategy to combat SARS‑CoV‑2. Te severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged as the causative agent of COVID- 19 in late 20191,2. Te disease pathology ranges from asymptomatic infection to severe acute respiratory distress and death3,4. -

COVID-19 Vaccine Frequently Asked Questions for Healthcare Professionals
COVID-19 Vaccine Frequently Asked Questions for Healthcare Professionals Table of Contents Vaccine Development and Approval 7 1) Is there a vaccine that protects against COVID-19 (SARS-CoV-2)? 7 2) When can we expect a vaccine to be available? 7 3) Why is this COVID-19 vaccine development timeline so condensed compared to when other vaccines are licensed? 7 4) The development and production of a COVID-19 vaccine has been called “Operation Warp Speed”, does this mean shortcuts have been taken? 8 5) What types of COVID-19 vaccines are in clinical trials? 9 6) How does the size of COVID-19 vaccine clinical trials compare to clinical trials for other vaccines routinely used in the United States? 10 7) Are people from different races and ethnicities being included in clinical trials for COVID- 19 vaccines? 10 8) What will be needed to license a COVID-19 vaccine in the United States? 10 9) What is Emergency Use Authorization? 11 10) Can you explain the difference between EUA and a Biological License Application (BLA)? 11 11) Why might the FDA issue an EUA before a BLA for a COVID-19 vaccine? 11 COVID-19 Vaccine Safety and Efficacy 12 12) Is the COVID-19 vaccine safety tested? 12 13) What is the current safety and efficacy of COVID-19 vaccines in clinical trials? 12 14) What is efficacy? Is there a difference between vaccine efficacy and effectiveness? 12 15) How does the efficacy of the Pfizer and Moderna vaccines compare to other vaccines? 13 16) What is the efficacy of the COVID-19 vaccine if I only receive one dose? 13 17) Is it true that people in the COVID-19 vaccine clinical trials died? 13 18) How will safety of the COVID-19 vaccine be monitored? 13 19) Is the COVID-19 vaccine being studied in children or pregnant women? 14 20) If vaccine trials do not include people with autoimmune conditions, how will we know if they can be vaccinated? 14 1 21) Do COVID-19 vaccines cause people to faint? 14 22) Can individuals with an allergy to latex receive a COVID-19 vaccine? 14 23) I heard reports of anaphylaxis following receipt of the Pfizer COVID-19 vaccine.